It's all the virus's fault!
The term "stomatitis" is derived from the merger of two Greek words: stoma (mouth) and itis (inflammation). There are a great variety of different types of disease - serous, aphthous, allergic, etc. The most dangerous is herpetic, or cold sore, stomatitis caused by a virus. Its main manifestations are painful ulcers covering the oral mucosa. The trigger mechanism of the disease is the activation of herpes simplex virus types 1 and 2. First of all, the disease threatens those who have a weakened immune system and, as a result, the body simply does not have the strength to give a worthy rebuff to viruses.
Forms of the disease
Lightweight
It is considered the most beneficial for the body. In this form, people with high immunity suffer from herpes stomatitis. It flows without temperature. It is distinguished by single rashes that do not cause discomfort and disappear on their own without consequences.
Average
General disorders are added: weakness, drowsiness, fatigue, loss of appetite. Rashes appear in several places at the same time. The temperature rises to 37-37.6°C.
Heavy
This form of stomatitis indicates extremely low immunity. The rashes are multiple and painful. Severe headache, chills, and vomiting appear. The temperature exceeds 38oC.
If the disease is mild, the patient may not notice any external signs!
How to distinguish herpes from stomatitis?
Many patients try to find an answer on the Internet to the question: “Do I have stomatitis or herpes? How to recognize? Herpes stomatitis can be easily distinguished from ordinary stomatitis by 3 key signs.
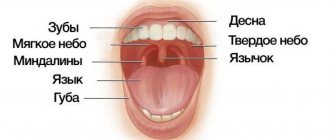
- With herpes infection, the rash is localized in the gum area. Whereas with stomatitis - on the soft tissues of the oral cavity (tongue, cheeks).
- A herpes rash first appears as blisters, which then ulcerate, while stomatitis begins with the appearance of ulcers.
- Herpetic stomatitis is characterized by a stable appearance of the rash in the same places, and with ordinary stomatitis its location often changes.
Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Herpetic or aphthous?
It will be somewhat more difficult to distinguish between herpetic and aphthous stomatitis. The latter got its name from the Greek term “aftha”, which means “ulcer”.
If with herpetic stomatitis there are many ulcers, but they are small, then with aphthous stomatitis there are few of them, and the size can reach 7–8 mm.
The second important distinguishing feature is the absence of swelling of the gums with aphthous stomatitis.
If you are looking for differences between herpetic and aphthous stomatitis, then the third thing you should pay attention to is the localization of the rash. Aphthous is characterized by the appearance of ulcers in the oral cavity, while herpes infection can spread to the border of the lips.
Symptoms of inflammatory diseases
Inflammation in the oral cavity is manifested by both general and local symptoms [1]. Even before the onset of local manifestations, general malaise, pain, irritation, rashes in the mouth, increased body temperature, and decreased appetite are noted [1]. In addition, inflammation in the mouth itself can act as a symptom of another disease or general pathology [1].
Symptoms of certain inflammatory diseases
Stomatitis is a wide group of diseases that can be caused by individual pathogens, for example, fungi (candidal stomatitis) or the herpes simplex virus (herpes stomatitis), and systemic diseases, for example, chronic diseases of the gastrointestinal tract (aphthous stomatitis) [2] .
Most often, stomatitis appears as rashes (ulcers, blisters or other forms) on the oral mucosa. The nature of the rash is a striking distinctive feature that plays an important role in diagnosis. For example, with aphthous stomatitis, the ulcers never appear on the outer surface of the lips, as is the case with lesions caused by the herpes simplex virus [2].
Herpetic stomatitis, as a rule, accompanies a general infection of the body and is characterized by rashes on the inner surface of the cheeks, tongue, palate, and lips [2].
With insufficient oral care, bacterial microflora may develop and cause deeper lesions of the mucous membrane.
If the necessary treatment of acute herpetic stomatitis is not carried out, a recurrent form occurs, which is accompanied by regular rashes on the oral mucosa of vesicles and aphthae "Microbiology, virology and immunology of the oral cavity", ed. Doctor of Medicine V. N. Tsareva.
Catarrhal stomatitis occurs quite often and develops due to the lack or poor hygiene and the presence of chronic foci of infection in the oral cavity. Symptoms of this type of stomatitis are swelling of the mucous membrane, the appearance of plaque on it, first white, then brown, and bad breath [1].
Candidiasis (candidal stomatitis, thrush) is caused by fungi of the genus Candida, which are normally always present in the mouth in small quantities [2]. Factors contributing to the sharp growth of fungi are long-term use of antibiotics and some other drugs, hypovitaminosis, endocrine and other disorders.
A striking symptom of candidiasis is the appearance of a white or yellowish-white coating on the tongue and the mucous membrane of the cheeks due to the development of inflammation in the mouth. The plaque is easily removed, revealing reddened, inflamed and eroded areas of the oral mucosa underneath.
Leukoplakia refers to chronic inflammatory diseases. It develops in response to constant irritation of the oral mucosa, for example, from a part of a denture, a sharp edge or chipped tooth, hot drinks or food, alcoholic beverages, or smoking [1]. Leukoplakia manifests itself in the form of whitish thickenings, usually in the cheek area along the line of closure of the teeth, in the corners of the mouth, on the back and on the lateral surfaces of the tongue.
How to distinguish herpes sore throat from stomatitis?
Despite the fact that these medical terms have the same grammatical root, herpetic sore throat and herpetic stomatitis are two different diseases. Unlike stomatitis, herpes sore throat occurs not due to the penetration of the herpes virus, but as a result of an adenovirus infection (in particular, the Coxsackie A virus). Children are more likely to suffer from this disease than adults. The rashes are localized, for the most part, on the soft palate and tonsils. Typical symptoms of stomatitis include pain in the abdomen and abnormal bowel movements.
Attention!
The disease begins acutely, with a jump in temperature to 40 degrees, and is severe, so differential diagnosis should only be carried out by a doctor.
Skin rashes in children: rashes, exanthemas, enanthemas
Rashes on the skin (exanthema, exanthema ) and mucous membranes (enanthema, enanthema ) can occur not only with viral and bacterial infections, but also with diseases of a non-infectious nature.
It is important to decide whether these changes represent a primary injury to the child's skin or whether the clinical signs have changed due to secondary factors (infection, trauma, or treatment). Examination by a pediatric dermatologist Moscow - Markushka clinic.
Elements of rashes in a child, children. Primary and secondary elements
There are primary and secondary elements of rashes. Primary elements are classified as roseola, spot, papule, nodule, wheal, vesicle, vesicle, hemorrhage. Secondary elements include pigmentation and depigmentation, scale, crust, erosion, crack, abrasion, ulcer, scar, cicatricial atrophy, lichenification, vegetation.
Primary elements of rashes in a child, children: roseola, spot, erythema, hemorrhage, pinpoint hemorrhages - petechiae, papule, tubercle, node, blister, vesicle, bubble
Roseola is a pale pink or red speck ranging in size from 1 to 5 mm. The shape is round or irregular, the edges are clear or blurred, does not protrude above the skin level, disappears when the skin is pressed and stretched. Roseola occurs in many infectious diseases, especially typhoid fever. Multiple roseola 1-2 mm in size are usually described as a pinpoint rash (with scarlet fever), in the process of resolution they become covered with scales or disappear without a trace.
The spot (makula) has the same color as roseola, size - from 5 to 20 mm, does not protrude above the skin level. The shape is most often incorrect. The spot disappears when pressure is applied to the skin and appears again after the pressure is removed. Multiple spots ranging in size from 5 to 10 mm are described as a small-spotted rash (for example, with rubella - a child is vaccinated against rubella at the Markushka children's clinic). Spots 10-20 mm in size form a large-spotted rash (for example, with measles, allergies - examined by a pediatric allergist in Moscow, Markushka clinic).
Erythema is large areas of hyperemic skin that are red, purple-red, or purple in color. It occurs as a result of the fusion of large spots formed by the dilation of blood vessels not only of the papillary layer of the skin, but also of the subpapillary vascular plexus. Spots larger than 20 mm that tend to coalesce should be considered erythema. Erythema is most typical for erysipelas, thermal, and ultraviolet burns .
Hemorrhage (haemorrhagia) is bleeding into the skin as a result of destruction of skin vessels. It looks like dots or spots of various sizes and shapes and does not disappear when the skin is stretched. The color is initially red, purple or violet, then, as the hemorrhage resolves, it becomes yellow-green and finally yellow (formation of hemosiderin during the breakdown of red blood cells). Color changes are clearly visible in larger hemorrhages.
Pinpoint hemorrhages are called petechiae (petechia). Multiple round hemorrhages measuring 2 to 5 mm are described as purpura . Irregular hemorrhages measuring more than 5 mm are called ecchymoses . Hemorrhages may overlap with other elements of the rash. In such cases, they speak of petechial transformation of roseolas, spots, papules. As a rule, this is observed in severe cases of the disease. Hemorrhagic rashes are detected with typhus (often in combination with roseola - roseola-petechial rash), hemorrhagic fevers, and sepsis. Hemorrhagic elements of irregular shape on a dense basis (stellate rash) are characteristic of meningococcemia and pneumococcal sepsis. Minor hemorrhages can also have a non-infectious origin (capillary toxicosis, toxic-allergic vasculitis, vitamin deficiency C, etc.).
Papule (papula) is an element of the rash that rises above the level of the skin, which is often determined by touch. It has a flat or dome-shaped surface, size - from 1 to 20 mm. The shape and color are the same as those of roseolas and spots. Papules often leave behind pigmentation and flaking of the skin. Papules that merge with each other form plaques, and when the latter merge, areas appear that are located on large areas of the skin, the size of a palm or more. Often, during a routine clinical examination of a child, it is very difficult or even completely impossible to distinguish roseola from papules. On the other hand, the same sick child can simultaneously have roseola, papules (typhoid fever, paratyphoid fever, infectious mononucleosis), papules and spots (measles - child measles vaccination, children's medical).
A tubercle (tuberkulum) is a limited, dense, cavityless formation protruding above the surface of the skin with a diameter of 1-2 to 5-10 mm. The tubercles are formed as a result of the accumulation of a specific inflammatory infiltrate in the dermis. Clinically, the tubercle is similar to a papule, but differs from it in that when palpating the tubercle, a dense infiltrate in the skin is always clearly visible. In addition, tubercles, unlike papules, undergo necrosis during reverse development, often form ulcers and leave behind a scar or cicatricial atrophy of the skin. The tubercles are most typical of cutaneous leishmaniasis, leprosy and tuberculous skin lesions, tertiary and late congenital syphilis.
A node (nodus) is a cavityless, limited compaction that goes deep into the skin, often standing above the skin level. The size of the knots ranges from a hazelnut to a chicken egg and more. They are formed as a result of the accumulation of cellular infiltrate in the subcutaneous tissue and the dermis itself. Inflammatory nodules have a soft or doughy consistency, unclear boundaries, and the skin over them is red. Nodules that appear as a result of specific inflammation (colliquatic tuberculosis, syphilitic gumma) have a dense consistency, are sharply demarcated from the surrounding tissues, and are prone to decay and ulceration with subsequent scarring.
A blister (urtica) is an acutely inflammatory, cavity-free element slightly elevated above the skin level, measuring from 2-3 to 10-15 cm or more, has a round or oval shape, and is often accompanied by itching. Color - from white to pale pink or light red. The blister usually forms quickly and disappears quickly, leaving no trace behind. It occurs as a result of limited acute inflammatory swelling of the papillary layer of the skin and simultaneous expansion of the capillaries. The appearance of urticarial elements is characteristic of allergic reactions of various origins (drug, food, cold allergies), including those of an infectious nature. Sometimes occurs in the pre-icteric period of hepatitis B (vaccination of a child against hepatitis in the Markushka children's clinic).
A vesicle (vesicula) is a cavity element measuring from 1 to 5 mm, representing a detachment of the epidermis. Usually the bubbles are filled with transparent, cloudy or bloody contents, they can shrink and give a transparent or brown crust. If the cover of the bubble is opened, then erosion is formed - a wet surface of pink or red color limited by the size of the bubble. The bubbles do not leave any scars on the skin. If a large number of leukocytes accumulate in a vesicle, it turns into an abscess - a pustule. Inflammatory changes are noted at the base and around the vesicle. Pustules are divided into single-chamber (chickenpox) and multi-chamber (natural smallpox). A group of blisters located on inflamed skin is called herpes. Vesicles are characteristic of herpes and enterovirus infections, chickenpox and natural pox. Chickenpox vaccination - Markushka Children's Clinic.
Bubble (bulla) is a cavity element with a diameter of up to 3-5 cm, located in the upper layers of the epidermis and under the epidermis. The contents of the blisters can be serous, bloody, or purulent. They can collapse, forming a crust, or open up, forming an erosive surface that turns into unstable pigmentation. The bubble occurs more often against the background of an erythematous spot, less often - against the background of unchanged skin (neonatal pemphigoid). The elements can be located both inside the epidermis, in the styloid layer (pemphigus vulgaris), and under the epidermis (multiform exudative erythema, dermatosis herpetiformis). It is observed with bullous form of erysipelas, sometimes with chicken pox, thermal burns.
Secondary elements of rashes in a child, children: hyperpigmentation, depigmentation, scales, erosion, abrasion, ulcer, cracks, tears, crust, scar, lichenification, vegetation
Secondary morphological elements are formed as a result of the evolution of the primary elements of the rash .
Hyperpigmentation (hyperpigmentatio) is a change in skin color as a result of an increase in melanin in it or the deposition of hemosiderin of primary elements.
Depigmentation (depigmentatio) occurs as a result of a decrease in the melanin content in the skin, observed after the disappearance of a nodule, tubercle - resolution of spotty-flaky (pityriasis versicolor, eczematoids) and papular (psoriasis) elements.
Scale (sguama) is an accumulation of rejected cells of the stratum corneum, sometimes the underlying layers of the epidermis. Scales occur on primary morphological elements - papules (psoriasis, syphilis), tubercles, after the resolution of blisters (eczema), etc.
Erosion (erosio) is a skin defect within the epidermis as a result of the opening of a vesicle, blister, or abscess, repeating their shape and size. When vesicles and pustules merge, erosions have scalloped edges. Erosion can also occur as a result of maceration of the skin in the area of folds or during maceration of other elements of the rash, most often papules. When erosion heals, there is no scar left; usually there is only temporary pigmentation.
An abrasion (excoriatio) is a violation of the integrity of the skin that occurs as a result of scratching, scratching, or other damage. Abrasions can be superficial - within the epidermis, sometimes involving the papillary dermis, and heal without a scar. Deeper abrasions, involving the deeper layers of the dermis, leave behind a scar. Abrasions are characterized by a tendency to become infected.
An ulcer (ulcus) is a deep skin defect that reaches the dermis, subcutaneous fat, fascia, muscles, and bones. It occurs as a result of the breakdown of the tissue of the primary element (tubercle, node, ecthyma). Its size is from 1 mm to the size of a coin or palm and more; the shape can be round, oval, linear, oblong, irregular. The surrounding tissue is either inflamed (edema, hyperemia) or infiltrated. Ulcers always heal with the formation of scars.
Cracks, tears (fissura, rhagades) - linear damage to the skin in the form of its rupture, resulting from excessive dryness due to loss of elasticity due to inflammatory infiltration or overstretching of the skin. Cracks can be located within the epidermis and dermis. They are usually localized in the corners of the mouth, interdigital folds, on the palms, soles, above the joints, and in the anus. A superficial crack after healing leaves no traces. After healing of deep cracks, linear scars remain.
A crust (crusla) is formed on the skin as a result of drying of the discharge of a weeping surface (vesicle, vesicle, abscess, ulcer, erosion). The crusts can have different colors (with serous exudate, transparent with a yellowish tint; with purulent exudate, yellow, greenish or brown; with hemorrhagic exudate, brown or black) and shape (layered, oyster-like, etc.).
A scar (cicatrix) is the formation of connective tissue at the site of a deep defect. Occurs after healing of deep skin defects at the site of ulcerated tubercles, deep pustules, nodes, deep burns, wounds. Scar formation is accompanied by the death of sebaceous and sweat glands, hair follicles, blood vessels and elastic fibers, and the disappearance of the skin pattern. Typically, scars are located below the skin level or are at its level, less often they rise above the skin level - hypertrophic scars.
Lichenification (lichenificatio) is a focus of increased skin pattern, accompanied by thickening and compaction, hyperpigmentation, and dryness. Foci of lichenification are most often localized in the neck, elbow and popliteal folds, wrist and ankle joints, inguinal folds, scrotum and occur in chronic dermatoses accompanied by itching (eczema, neurodermatitis).
Vegetation (vegetatio) is a papillary thickening of the skin that occurs as a result of the growth of the styloid layer of the epidermis and papillomatosis of the dermis during a long-term inflammatory process. More often it forms in the area of papular elements and ulcers. Vegetations can erode, bleed, and are prone to secondary infection.
Bacterial or viral?
In addition to viral origin, the disease can be caused by bacteria: streptococci and staphylococci are normally present in the microflora of the oral cavity and begin to multiply uncontrollably during the inflammatory process. The latter may be caused by caries or periodontitis (read more about the disease in the article).
How to distinguish viral stomatitis from bacterial one? It is extremely difficult to do this at home, so it is better to consult a doctor. The main differential feature is the localization of the rash. With viral herpetic stomatitis, vesicles with transparent contents first appear on the tongue (its tip, along the side surfaces and under it), and then can even spread to the pharynx and tonsils.
For bacterial stomatitis, the location of the rash on the gums and those areas where the skin borders the mucous membrane (for example, on the red border of the lips) is more common. Also, with a disease caused by streptococci, “jams” are often observed - pustules on the corners of the mouth, which quickly begin to bleed, become covered with a crust, crack and cause constant discomfort while eating and talking.
Types of diagnostics
An experienced doctor can identify herpetic stomatitis in adults during an initial examination, relying on only two methods.
- Clinical picture.
Based on the totality of the patient’s specific complaints and distinctive external signs, the dentist will not only assess the severity of the disease, but also differentiate it from ordinary stomatitis, candidiasis, etc. - Immunofluorescence.
Express microscopy method, the most accurate for diagnosing acute herpetic stomatitis.
Change in structure with fluid accumulation
With such lesions, the structure of the mucous tissue changes so that a cavity filled with liquid is formed inside.
Bubbles and bubbles. They are formed in the epithelial layer or under it, filled with serous or hemorrhagic contents, and can be grouped. The cavity is closed by a thin layer of epithelium, which can break through. Bubbles can group and break quickly. Bubbles form and last longer. Both types of lesions provoke the formation of healing ulcers on the surface of the mucous membranes. They arise due to damage by viruses, traumatic injuries, and disturbances in tissue nutrition.
Ulcers. They can form from blisters or on unchanged mucosa. The cavity is filled with purulent exudate (whitish, yellowish, greenish contents with a pungent odor). They can be deep or superficial, often painful. Indicate an inflammatory process, appear after traumatic damage to the mucous membrane, due to infectious, viral diseases.
Cysts. A formation with dense walls that form a cavity. It is filled with transparent contents (can become purulent, serous, bloody). Appear due to blockage of gland ducts on the mucous membranes or as a symptom of periodontal diseases.
Causes of herpes stomatitis
There are two types of herpetic stomatitis: acute and chronic. Acute herpetic stomatitis, according to Dr. Komarovsky, occurs only in children under 3 years of age, when for the first time the child’s body, already deprived of antibodies to the herpes virus received from the mother, is first exposed to a viral attack from the outside. Moreover, the source of infection, as a rule, is the parents themselves - carriers of the virus, who kiss the baby or lick his pacifier or feeding spoon.
Recurrent or chronic stomatitis is already the lot of adults. The disease is recurrent in nature as soon as the body’s immune forces are weakened. In this case, primary infection can occur either through airborne droplets (sneezing), or through household contact (for example, through the use of the same dishes with a virus carrier) or hematogenous (through blood during injections, etc.). The incubation period of the disease can last up to two weeks depending on the state of the immune system.
Attention!
The pathogenesis of the disease in dentistry is still unknown. But if the body is weakened, any injury to the palate or gums can provoke activation of the herpes virus types 1 and 2!
Types of inflammatory diseases of the oral cavity
These diseases are classified depending on what causes the inflammation, as well as on the location of its source in the mouth.
Thus, general lesions of the mucous membrane are called stomatitis [1]. If the mucous membrane of only the tongue, lip, palate, gums or alveolar process becomes inflamed, they speak of glossitis , cheilitis, palatinitis, gingivitis or periostitis, respectively.
Depending on the reasons that caused the inflammatory process, these diseases are divided into:
- infectious;
- traumatic;
- symptomatic;
- specific.
If left untreated, inflammation can occur with complications and have negative consequences both for the teeth, gums, mouth and pharynx, and for the general health of a person.
Treatment of herpetic stomatitis
How to treat herpes stomatitis? Unfortunately, the herpes virus, once entered into a person’s blood, remains in a “dormant” state for the rest of his life. But treatment of viral stomatitis is possible provided that you do not delay visiting the dentist when the first signs of the disease are detected. During the period of therapy, in order to avoid infecting loved ones, you should eat and drink from separate containers and avoid kissing. The patient is recommended a diet that excludes spicy, smoked, sour and salty foods, which can irritate the damaged oral mucosa, and an increased drinking regimen (up to 2.5 liters per day), aimed at combating the manifestations of general intoxication of the body.
Primary malignant melanoma of the oral cavity
Primary melanoma in the oral cavity is a rare neoplasm with aggressive growth and developing from malignantly degenerated melanocytes of the oral mucosa. The World Health Organization defines this disease as a malignant neoplasm of melanocytes or their precursors. Melanoma is formed due to the proliferation of atypical melanocytes at the junction of the epithelium and connective tissue. The disease is also accompanied by upward migration of cells into the layers of the epithelium and the introduction of underlying connective tissue. Melanoma is usually found on the skin, but its localization is also possible on the oral mucosa. Over the past decades, the incidence of melanoma in the population has increased significantly (3-8% per year). In 1960, melanoma was thought to occur in 1:500 cases, then in 1992 the incidence was 1:600, in 1996 1:105, in 1998 1:88 and by 2000 1:75 cases.
Localization of melanoma in the oral cavity accounts for 0.2-8% of all cases of tumor development and 0.5% of the total number of all neoplasms of the oral cavity. Melanoma typically develops between 30 and 90 years of age (most often around age 60) and is slightly more likely to affect men than women. The main sites of localization include the hard palate and gums (affecting the upper jaw in 80% of cases). Slightly less common than the primary process is secondary melanoma as a metastasis of a distant tumor. In such cases, the typical localization is the tongue, parotid salivary gland and palatine tonsils. Melanoma of the oral mucosa is characterized by greater aggressiveness and clinically manifests itself mainly at the stage of nodule formation. Histologically, this tumor is defined as invasive, in situ, or a combination of invasive and in situ. About 85% of all melanomas that occur belong to the latter class.
No specific etiology of this disease has been identified. It is also still difficult to determine risk factors for melanoma. Like skin neoplasms, primary melanoma of the oral mucosa is most often formed from a nevus, pigment spots, or de novo (about 30% of cases). In this article, we offer for consideration four clinical cases of primary melanoma with different localizations.
Description of clinical cases
Clinical case 1
A 70-year-old woman came to the clinic with complaints of a rapidly growing dark-colored formation located in the anterior part of the oral cavity on the upper jaw, which appeared about 4 months ago. Approximately two months before treatment, the patient discovered a small, dark, dense formation in the anterior part of the oral cavity on the upper jaw, which was constantly increasing to its present state. The patient has a bad habit: she has been using chewing tobacco since she was 20 years old.
An external examination revealed a localized swelling in the area of the upper lip, the skin over the formation was unchanged. A dense swelling raises the upper lip (Photo 1). Lymphadenopathy of the cervical lymph nodes was not detected.
Figure 1: External and intraoral view showing a pigmented lobular swelling in the upper lip area.
An intraoral examination revealed a lobulated, raised, pigmented swelling. The mass was firm, inelastic, incompressible, non-contractile, without fluctuation or pulsation, with well-defined margins and occupied the anterior part of the maxilla from the mesial edge of tooth 13 to the distal edge of 24 (Figure 1).
An orthopantomogram revealed partial absence of teeth and a large radiolucent zone with poorly defined boundaries in the anterior part of the upper jaw, which extended from tooth 13 to tooth 23 (Photo 2).
Photo 2: Orthopantomogram showing a large, irregularly shaped radiolucent area.
A biopsy of the neoplasm was performed under local anesthesia, which showed the presence of layers of atrophic squamous epithelium with large round and oval melanocytes with vertical and radial growth. Modified proliferating round and oval melanocytes and chronic inflammatory cells were diffusely distributed in the connective tissue stroma (Photo 3).
Photo 3: Clinical case 1. Photomicrograph (10 x and 40 x). Round and oval melanocytes and melanin pigmentation distributed in the connective tissue stroma.
The totality of data obtained from clinical, radiological and histological studies gives the right to make a diagnosis of malignant invasive melanoma with a density of 0.90 mm. This conclusion was further confirmed using the immunohistochemical marker HMB-45 and Melan-A (Figure 4).
Photo 4: Clinical case 1. Immunohistochemical marker with the HMB-45 antibody, staining the cytoplasm of epithelial cells.
Due to the large size of the tumor, surgical treatment was not possible. It was decided to prescribe radiotherapy. Subsequent examinations revealed partial regression of the tumor. Next, surgical intervention was planned, but the woman did not return to the clinic. Ten months later, the patient was hospitalized, but refused the proposed immunotherapy and took only painkillers. Fifteen months later the patient died. An autopsy was not performed, so the exact cause of death remains unclear.
Clinical case 2
A 42-year-old man came to the clinic with complaints of a rapidly growing exophytic mass in the left cheek area.
Three months ago, the patient did not report any symptoms, then he noticed an ulcer the size of a coin on the mucous membrane of the cheek. The formation gradually increased to its present size.
An external examination revealed a single large, dense, palpable lymph node not fused to the tissues in the left submandibular region. A diffuse, dense, pliable swelling was also detected, located from the left corner of the mouth and from the lower edge of the lower jaw to the middle of the buccal region. Deviations of the corner of the mouth to the side were visually noted (Photo 5).
Photo 5: Photograph of the patient's appearance. Distortion of the face with a shift to the right side and enlarged submandibular lymph nodes.
An intraoral examination revealed two exophytic formations, black-brown in color, measuring 3 x 4 cm and 2 x 2 cm, with a lumpy surface and dense consistency, localized on the mucous membrane of the left cheek from the corner of the mouth to the area of tooth 38 (front-to-back) and from the vestibule of the oral cavity to 1 cm above the occlusal plane (top to bottom). An area of hyperpigmentation was noted in the retromolar area (Figure 6).
Figure 6: Intraoral view showing an exophytic lesion extending from the corner of the mouth to the area of tooth 38.
A biopsy of the tumor was performed, which showed the presence of dysplastic oval and spindle-shaped melanocytes in the lamina propria interspersed with melanin pigmentation (Figure 7).
Figure 7: Case 2. Photomicrograph (10x) showing invasive tumor growth, atypical melanocytes and melanophages.
The totality of data obtained from clinical, radiological and histological studies gives the right to make a diagnosis of malignant invasive and in situ melanoma. This conclusion was further confirmed using the immunohistochemical marker HMB-45 and Melan-A (Figure 4).
Wide excision of the lesion was performed as therapy. Histopathological examination confirmed melanoma with a maximum density of 1.10 mm, which infiltrated the superficial layers of the underlying tissues and metastasized to the regional lymph node.
Clinical case 3
A 65-year-old man was admitted to the clinic with complaints of a painful swelling in the oral cavity on the left side, which began to bother him approximately 15 days ago. Two weeks before presentation, the patient discovered a small, dense formation on the upper gum on the left.
An X-ray examination did not reveal any significant changes.
An external examination revealed submandibular lymph nodes, palpable on both sides, measuring 2 x 2 cm, dense, mobile and fused to the lower edge of the lower jaw.
An intraoral examination revealed a dense, raised, pigmented swelling on the upper gum, measuring 0.5 x 1.5 cm, located near teeth 21, 22, 23 and 24. The change in gum color affected the area from tooth 21 to 28 and on the palatal side from 21, 22, 23 to 26, 27 and 28. Pigmented areas were observed bilaterally on the mucous membrane of the cheeks and palate.
A biopsy of the neoplasm was performed, which showed the presence of atypical melanocytes interspersed with melanin pigmentation and located deep in the connective tissue stroma.
The totality of data obtained from clinical, radiological and histological studies gives the right to make a diagnosis of malignant invasive melanoma. This conclusion was further confirmed using the immunohistochemical marker HMB-45 and Melan-A (Figure 8).
Photo 8: Clinical case 3. Immunohistochemical study using Melan-A, staining the cytoplasm of cells.
As a therapy, resection of the upper jaw was performed with removal of the affected lymph nodes. Histopathological examination confirmed gingival melanoma measuring 3.20 mm with lymph node involvement (II).
Clinical case 4
A 40-year-old woman came to the clinic with complaints of painful swelling in the area of the right anterior gum on the upper jaw and a change in the color of the mucous membrane on the palatal side. The disease began 4-5 months ago, when the patient noticed a swelling in the area of the right anterior gum on the upper jaw and turned to the doctor for help. At the appointment, the specialist also revealed pigmentation of the mucous membrane on the side of the palate.
An X-ray examination did not reveal any significant changes.
An external examination revealed a single dense palpable submandibular lymph node measuring 5 x 5 cm on the right side.
An intraoral examination revealed dark pigmentation between teeth 21, 22, 23 and a pigmented dense flat swelling on the palatal side in the area of 11 and 12, measuring 1 x 1 cm, with irregular edges (Photo 9).
Photo 9: Intraoral photographs. Black pigmentation of the gums and palate.
A biopsy of the neoplasm was performed, which showed the presence of oval and spindle-shaped modified melanocytes in the connective tissue stroma (Photo 10).
Figure 10: Case 4. Photomicrograph (10x) showing atypical melanocytes in the connective tissue stroma.
The totality of data obtained from clinical, radiological and histological studies gives the right to make a diagnosis of malignant invasive melanoma. This conclusion was further confirmed using immunohistochemical markers.
After the diagnosis of primary gingival melanoma was made, treatment included resection of the left part of the alveolar process of the upper jaw with removal of the tumor on the gum. The defect was reconstructed using a cheek flap; the postoperative period passed without complications. Histopathological examination confirmed a 1.5 mm melanoma with lymph node involvement (I). The recovery period was uneventful.
Discussion
Oral melanoma can exhibit significant variability in morphology, development, and clinical presentation.
Research shows that from 20.41% to 34.4% of all melanomas are on the surface of the mucous membranes and 16% of them are inside the oral cavity. Scientists also report the most susceptible age group: 56 – 77 years. The average age of a patient with melanoma is 69.2 years. According to various sources, the distribution by gender (male:female) varies from 1:1 to 2:1.
Melanoma most often develops on the upper jaw, in most cases affecting the palate (32%), followed by the gums on the upper jaw (16%) and somewhat less often on the mucous membrane of the cheeks, gums on the lower jaw, lips, tongue and floor of the mouth. Our article describes three cases of a tumor on the gum of the upper jaw and one case on the buccal mucosa, the ratio of men to women is 1:1, which corresponds to the literature data (Table 1).
Table 1: Clinical and pathological data of patients with primary melanoma of the oral mucosa.
Melanoma can be classified as a primary tumor of the oral mucosa only if the criteria described by GREEN in 1953 are met: the presence of melanoma on the oral mucosa, the presence of proliferative activity and the absence of primary melanoma outside the oral cavity. In the cases we described, all the above criteria are met, so we can talk about primary melanoma occurring in the oral cavity.
To confirm the diagnosis, it is necessary to establish the presence of melanin pigment. This procedure is carried out using Fontana-Masson staining and suitable immunohistochemical markers such as HMB-45, Melan-A, Tyrosinase and Antimicropthalmia transcription factor. Also, an analysis for the presence of protein S-100 in melanoma is always positive. In the presented clinical cases, the diagnosis was confirmed using the markers HMB-45 and Melan-A.
For the development of primary melanoma in the oral cavity, the geographical feature does not matter, as, for example, for melanoma of the skin, in which the degree of ultraviolet radiation is of particular importance. Primary melanoma of the oral cavity is a fairly aggressive disease, and at the beginning of its development requires careful differential diagnosis with such conditions as Addison's disease, Kaposi's sarcoma and Peutz-Jeghers syndrome. Melanoma must also be differentiated from melanin pigmentations (both for racial reasons and those arising due to irritation), nevus, melanoacanthoma and other pigmentations of exogenous origin, for example, discoloration of the gums under the influence of amalgam.
Delgado Azanero and other scientists have proposed a practical and easily implemented method for diagnosing melanoma in the oral cavity and also differentiating this tumor from other pigmented lesions.
The clinical test is as follows: a piece of bandage is rubbed on the surface of the formation, and if it turns dark, the test is considered positive. The coloring is explained by the presence of melanin pigment in the surface layers of the tissue. The authors report that in 84.6% of cases the test was positive, however, a negative result does not exclude the presence of this tumor, since sometimes malignant cells do not penetrate the surface layers of the epithelium. Melanoma of the oral mucosa, which is characterized as nodular and has vertical growth with penetration into the submucosal layer, is considered even more aggressive. The prognosis in such cases is usually unfavorable and depends on the histological type of the tumor, the depth of its penetration and location. According to the literature, mucosal melanoma most often occurs in areas where tissue covers bone formations, for example, on the hard palate or on the gums. This localization further worsens the prognosis of the disease, since the tumor begins to penetrate the bone tissue very quickly.
The precursors of the disease have not yet been fully identified, however, some scientists talk about initial melanocytic hyperplasia, which can be considered the onset of the disease. Other researchers point to the important role of various types of pigmentations, which initially have horizontal growth and only then acquire an invasive - vertical type of growth. Also of some importance are ordinary nevi, which, interestingly, in the oral cavity are most often located on the hard palate, like melanomas. Primary melanoma in the oral cavity was first described by Weber in 1859, however, clear diagnostic criteria, as for melanoma of the skin, did not exist for a long time. Subsequently, many classifications of this disease were put forward, but none of them was accepted as universal.
Melanoma in the oral cavity must be distinguished from melanoma of the skin and divided into two histological types: invasive and in situ, as well as a combined version of an invasive tumor with an in situ component. If the result of a cytological examination of a neoplasm is doubtful, then the concept of “atypical melanocytic proliferation” should be used. This term is taken as a preliminary diagnosis, while the final one is made only after a clinical, pathological examination, repeat biopsy and constant monitoring. The diagnostic criteria used to identify cutaneous melanoma (asymmetry, irregular contours, discoloration, diameter greater than 6 mm, and elevation) may also be useful for diagnosing oral melanoma.
The scientific institute examined 50 cases of malignant melanomas, 15% of which were determined to be tumors in situ, 30% were invasive and 55% were of a mixed nature. In our article, 3 clinical cases describe invasive melanoma and one case describes mixed type melanoma (Table 1). Since all patients were treated at late stages of the disease, it is quite difficult to guess which component, invasive or in situ, appeared earlier. However, there is an opinion that the combined type of melanoma is often preceded by pigmentation located exactly at the site of future tumor development.
Localization on the mucous membrane makes it much more difficult for patients to detect the formation, which leads to untimely diagnosis and, ultimately, a large percentage of deaths. According to statistics, from 13 to 19% of all patients have metastases in the lymph nodes, and in 16-20% metastasis develops in a very short period of time. The aggressive clinical course of primary melanoma in the oral cavity causes even more problems. Malignant melanoma on the mucous membrane accounts for 0.2-8.0% of all melanomas and has a much worse prognosis for recovery than a similar disease on the skin. The five-year survival rate of patients affected by this tumor varies from 5.2 to 20%. However, the chances of recovery and recovery from melanoma are greatly increased if diagnosis and treatment can be carried out in the early stages of the disease.
Surgery remains the most effective treatment for malignant melanoma. It is important to note that surgical intervention must be radical and accompanied by a long postoperative observation period. However, wide excision of cutaneous melanoma involving 20-50 mm of healthy tissue, which is considered sufficient, is not always applicable for melanoma in the oral cavity.
Conclusion
It is very important to include an examination of the oral cavity in the general preventive examination of the skin. To prevent the development of oral melanoma, any densely pigmented areas that cannot be explained should be biopsied. Morphological variability, asymptomatic course, rarity of occurrence, poor prognosis, need for specialized treatment - all those factors that must be taken into account when diagnosing and choosing therapy for this malignant neoplasm.
Vigilance and careful analysis of these and other clinical cases can be very useful for creating a clear classification, early diagnosis, as well as contributing to timely treatment and improving the prognosis of this rare pathology.
Authors:
Ajay Kumar , Department of Dental and Maxillofacial Pathology with Microbiology, ITS Center for Dental Research, Muradnagar, Ghaziabad, Uttar Pradesh
Ruchi Bindal , Department of Dentistry and Radiology, ITS Center for Dental Research, Muradnagar, Ghaziabad, Uttar Pradesh
Devi C. Shetty , Department of Dental and Maxillofacial Pathology with Microbiology, ITS Center for Dental Research
Harkanwal P.Singh , Department of Dental Pathology and Microbiology, Swami Devi Dyal Dental College and Hospital, Pranchkula, Haryana, India
Drug therapy
Rinse
To stop the spread of infection throughout the oral cavity, as well as to prevent the occurrence of sore throat, anti-inflammatory drugs such as Stomatidine and Miramistin are prescribed. The greatest effect is achieved by repeating the rinsing procedure every 3 hours, strictly adhering to the instructions for medicinal solutions.
Antiviral drugs
To suppress the reproduction of the herpes virus, the patient is advised to take “Immudon” and “Acyclovir” orally according to the scheme, and for external use - “Viferon” ointment or “Silicea” gel.
Vitamin therapy
Tablet vitamin complexes such as “Complivit” help improve immunity.
Attention!
Before use, consultation with a specialist is recommended!
Treatment at home with folk remedies
On the Internet you can often come across the question: “How to treat herpetic stomatitis with folk remedies?” Let’s make a reservation right away: when treating this disease, you cannot rely solely on traditional medicine methods. Therapy must be comprehensive, and only a doctor can choose it correctly.
An effective folk remedy for rinsing the mouth is propolis tincture diluted with boiled water 1:3. In case of pronounced “jams” in the corners of the mouth and painful ulcers inside, applications with natural sea buckthorn oil have an analgesic and wound-healing effect.
Prevention measures
- Strengthening the immune system.
Avoid excessive exercise and stress. Take a multivitamin in the fall and spring. Regular exercise and hardening increase the vitality of the body. - Healthy lifestyle.
Get rid of bad habits: scientists have proven that excessive smoking and alcoholic beverages can become a catalyst for the activation of the herpes virus in the body. - Timely treatment of chronic diseases.
Do not forget that simple stomatitis, if you do not seek medical help in a timely manner, can develop into herpetic stomatitis. Chronic caries and acute respiratory viral diseases suffered “on the legs” also seriously undermine the body’s immune defense. - Maintain personal hygiene.
According to statistics, it is poor oral hygiene that most often opens the way for herpes infection. - Avoid oral trauma.
Even a minor microcrack from a prick with a fish bone or careless use of a toothpick can become an “entry gate” for the herpes virus.
Attention!
With reduced immunity, herpes stomatitis becomes chronic and relapsing: the disease can recur 2-6 months after recovery.
How to get rid of stomatitis and other inflammatory diseases of the oral cavity
Treatment of stomatitis and other inflammatory diseases is usually comprehensive, aimed at alleviating the patient’s condition, eliminating the root cause and risk factors.
Often, inflammation of the oral cavity is painful, accompanied by itching, irritation, and swelling of the mucous membrane. Because of this, patients have difficulty eating. To alleviate the condition, the affected areas are treated with various anesthetic and antiseptic rinses, powders, and solutions. This also prevents possible complications of diseases, for example, the transition of aphthae or foci of inflammation into ulcers, which require more time to heal.
Another important area of treatment is the elimination of local causes of inflammation of the oral mucosa. These include local foci of infection, for example, caries , dental plaque (tartar), traumatic chipped teeth, protruding parts of fillings or dentures [1]. For this purpose, appropriate treatment and professional hygiene are carried out.
And finally, a significant part of therapy is devoted to the diagnosis and elimination of a general disease that can provoke inflammation of the oral cavity (for example, endocrine disorders or chronic diseases of the gastrointestinal tract) [1]. In special cases, antiviral drugs [5], antimycotics [6] and antibiotics [1] are used.
Prevention of stomatitis and other inflammatory diseases includes [7]:
- treatment of major systemic diseases;
- strengthening general immunity: adherence to the principles of a healthy lifestyle, nutrition, giving up bad habits, eliminating hypo- and avitaminosis;
- strengthening local immunity: regular careful hygiene, avoiding injury and irritation of the mucous membrane in the mouth.
Regular individual and professional oral hygiene is a key way to prevent intraoral inflammation. It must include:
- brushing your teeth twice a day, after breakfast and before bed, with a soft-bristled brush and toothpaste;
- the right choice of toothpaste: if you are prone to inflammation of the mouth and gums, as prescribed by a specialist, you should give preference to pastes with anti-inflammatory and antiseptic properties;
- use of antibacterial rinses with anti-inflammatory effects;
- cleaning interdental spaces with dental floss or tape;
- regular visits to the dentist (once every 6 months) for a preventive examination and professional removal of dental plaque.