Causes of development of cleft palate in the fetus
The list of factors that can provoke this pathology is quite wide. Among them are both related to the expectant mother and external:
- genetic predisposition;
- toxicosis;
- exposure to bacteria and viruses;
- chronic diseases of the mother (gynecological, respiratory organs);
- infectious diseases of the mother (herpes, sore throat, influenza, otitis and bronchitis);
- smoking and alcohol abuse during pregnancy;
- taking medications (antibiotics, salicylates, sulfonamides);
- work in hazardous production;
- stress;
- sudden changes in atmospheric pressure;
- radiation, including solar;
- environmental violations [2, 3].
Environmental influence is last on the list, but not least. As a result of rapid technogenic development, the state of the environment is steadily deteriorating. Largely because of this, the percentage of newborns with cleft palates has tripled over the past 100 years [4].
Why carry out the procedure?
The main indications for this type of operation are congenital malformations, which are associated with impaired formation of the soft tissues of the lips, nose, soft and hard palate during intrauterine development. In this case, veloplasty is performed to eliminate the cleft of the soft palate; usually such operations are accompanied by uranoplasty (hard palate plastic surgery) and cheiloplasty (restoring the shape of the lip).
One of the possible indications for veloplasty is snoring associated with sagging of the soft palate and an increased size of the uvula. To prescribe this operation for such a problem, the doctor must carefully examine the patient’s condition and accurately identify the etiology of snoring.
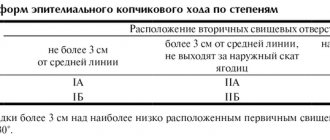
Classification of defects
Based on their shape and anatomical features, congenital clefts are divided into several types and subtypes. First of all, they focus on localization:
- clefts that affect only the soft palate;
- clefts affecting both the hard and soft palates;
- clefts of the soft, hard palate and alveolar process;
- clefts of the alveolar process and the anterior part of the hard palate.
Then the degree of expression is assessed.
- Hidden: located within the muscle tissue of the soft palate and the bone tissue of the hard palate, without extending to the mucous membrane.
- Incomplete: the palate is partially cut.
- Full: completely cut through the palate.
They also describe whether the defect appears on one or both sides of the face. As a result, the classification takes the following form:
- clefts of the soft palate can be hidden, incomplete or complete;
- the same varieties in clefts of the soft and hard palate;
- clefts of the soft, hard palate and alveolar process are always complete and can be one- or two-sided;
- clefts of the alveolar process and the anterior part of the hard palate can be complete or incomplete, in both cases - unilateral or bilateral [4].
Risks of the procedure
When performing an operation to restore the soft palate, complications such as complete dehiscence of the suture, slit-like or perforated defects, malocclusion (oblique or mesial bite), immobility of the palate, rough scars, and tissue necrosis are possible. In case of improper care or poor quality of surgery, infectious complications are possible.
When eliminating snoring through conventional surgery, laser therapy or cryotherapy, complications such as loss of function of the soft palate are possible, which may include impaired swallowing and nasal breathing, cicatricial stenosis of the pharynx, nasal speech, and lack of obturator function of the palate. The most modern and safe method of treating snoring is somnoplasty.
Surgical treatment of cleft palate
Maxillofacial surgeons perform the first simple operation in infancy - usually before 2 years. We are talking about eliminating a defect in the soft palate, or veloplasty. Thanks to it, blood supply to tissues and development of the muscles of the soft palate improves. Moreover, even the bone plates of the hard palate also begin to grow after surgery [2].
However, veloplasty is sufficient only for cleft soft palate - the mildest form of pathology. If the cleft palate also affects the hard palate, the main stage of treatment is a much more complex operation - the so-called uranoplasty. Such interventions have a history of almost 200 years, and during this time several effective techniques have been developed. Essentially, they all boil down to three main tasks:
- close the cleft palate;
- lengthen the soft palate;
- narrow the middle part of the pharynx.
The main differences lie in the surgical protocol: it can be radical, when all corrections are performed in one intervention, or gentle, in which the surgeon’s actions are divided into two stages [4].
Gentle uranoplasty was developed primarily in order to perform operations as early as possible. Therefore, it is faster to return the child to normal life and begin rehabilitation. However, there is still no consensus among specialists about the optimal period for surgical intervention. Some doctors believe that it is best to eliminate the cleft at 2–4 years of age. Others, on the contrary, argue that it is not advisable to operate before 4 years of age [4].
Regardless of the operation protocol, preparation for it plays the most important role. Uranoplasty is a complex intervention (including when performed in childhood), and to minimize risks, all actions are carried out with special care:
- restorative treatment;
- sanitation of the oral cavity and pharynx;
- examination of all organs and systems of the body;
- swab from the throat and nose for pathogenic microflora;
- testing the protective palatal plate and, if necessary, correcting deficiencies;
- preoperative speech therapy training, which greatly facilitates the work of a speech therapist after uranoplasty [4].
The maxillofacial surgeon is the main coordinator in the rehabilitation of the child. Then ENT doctors, orthopedists, dentists , audiologists, and neonatologists (in the early stages) are involved, who guide the child according to the specifics of the corresponding pathologies.
Then we get team play and an integrated approach to rehabilitation. Grichanyuk D. A., Ph.D., Associate Professor of the Department of Maxillofacial Surgery of BelMAPO, member of the American and European Association of Craniomaxillofacial Surgeons [1]
Cleft palate
It happens that absolutely healthy parents give birth to a baby with severe pathology. In this case, the diagnosis of a neonatologist in the delivery room may sound like a death sentence. But do not despair and give up: modern medicine and, in particular, plastic surgery are quite capable of coping with even the most complex defects.
A cleft palate is a congenital anomaly of the development of the maxillofacial system, in which a cleft forms in the place of the palate in a child during the prenatal period, connecting the oral and nasal cavities.
This condition requires multi-stage surgical correction, but with proper treatment, the child will live and develop absolutely fully, not lagging behind his peers in any way. What are the dangers of problems with the palate, what ways can you correct them and how to help your child cope with an unpleasant feature, read on TecRussia.ru:
↑ Why does a cleft palate appear?
According to medical statistics, cleft palate is the most common birth defect in newborns. On average, it is detected in one out of 750–800 infants, and over the past 20 years the number of such children has increased by one and a half times.
It has now been established that the pathology appears due to a genetic mutation of one of the X chromosomes. It can be transmitted to the child by one of the parents, or arise already at the stage of its intrauterine development. There are several reasons for the defect to appear:
- parents working in hazardous industries, living in an area with unfavorable ecology;
- severe toxicosis of pregnant women;
- taking medications by the mother that can harm the fetus, as well as taking alcohol, drugs, smoking;
- lack of folic acid;
- maternal obesity;
- parents' age over 35 years;
- severe emotional turmoil for a woman during pregnancy.
If there are no other complications, then the child’s intellectual and physical development does not suffer (subject to proper care). If the cleft palate is combined with other defects, the prognosis is often unfavorable and depends on which vital functions of the body are impaired.
↑ Types of congenital anomalies
In maxillofacial anatomy, a distinction is made between the soft and hard palate:
- the soft consists of muscles, aponeurosis (a special connective tissue layer) and mucous membrane;
- the hard one is formed by the processes of the upper jaw, which are located horizontally and along the midline are connected to the unpaired bone of the facial part of the skull by the vomer;
In cases where the cleft affects only the soft palate, they speak of incomplete cleft. If it stretches from the uvula to the alveolar process of the jaw, then it is called complete. In some cases, the defect can move from the palate to the outer part of the mouth, then a combination of cleft palate and cleft lip is diagnosed (see also the article “Cleft lip in children”).
↑ Consequences of the disease
Cleft palate disrupts a number of natural processes, which can ultimately cause a slowdown in the child’s physical and intellectual development:
| Function | Possible problems |
| Breath | The air that enters the lungs of children with a cleft palate is not moistened or warmed as it normally is. Therefore, such children are more susceptible to bronchitis and pneumonia. With a significant size of the defect, inhaled air can partially escape through the slightly open mouth or through the nose, resulting in a chronic lack of oxygen, affecting the development of the brain and intelligence. |
| Sucking | The presence of a cleft prevents the child from sucking, he does not receive enough nutrients and does not gain weight. Any liquid that enters the mouth also pours into the nasal cavity, flows into the sinuses and Eustachian tubes (canals that connect the middle ear to the nasal cavity). Hence the risk of developing sinusitis and otitis media. The latter can lead to hearing loss over time. |
| Chewing | If the cleft reaches the alveolar ridge of the upper jaw (the part where the teeth grow), a malocclusion can form. In this case, chewing food is disrupted, creating additional stress on the digestive system. |
| Speech | The absence of a full soft palate makes it difficult to pronounce sounds. A complete cleft leads to the appearance of open rhinolalia (nasal sound, distortion of spoken sounds). |
| Social skills | If the developmental defect is not corrected in time, then children with a cleft palate begin to shun their peers, become shy, and withdraw into themselves. A decrease in self-esteem negatively affects social adaptation and leads to an even greater decrease in the quality of life. |
↑ How to fix a cleft palate? Features of the operation and other aspects of treatment
Recreating the correct shape of the hard and soft palate is not a matter of one day. In the simplest cases, to obtain a satisfactory result, you can get by with one plastic surgery, but as a rule, you will need much more: from 2 to 7. This figure in each specific case will be determined by the length of the cleft and the presence of accompanying defects.
To carry out comprehensive treatment and complete rehabilitation of children with cleft palate, the help of specialists in a wide range of fields is needed:
- pediatrician: helps the mother establish breastfeeding, and also selects special devices for feeding liquid and solid foods, monitors the baby’s weight gain and development;
- plastic or maxillofacial surgeon: performs palatoplasty to close the gap between the nasal and oral cavities. Also, eliminates cleft lip, if any;
- orthodontist: corrects, if necessary, the growth of teeth, forms the correct bite;
- speech therapist, neurologist, ENT doctor, etc.
Another difficulty is that it is impossible to close the palate defect immediately after the birth of the child: the upper jaw is still too small to perform surgical manipulations on it. Operation on the soft palate can be performed no earlier than after 3-6 months, and on the hard palate - after one and a half to two years.
↑ Preoperative care for children with cleft palate
The very first thing you need to worry about is feeding. There are several ways to do this correctly:
- Breastfeeding using special pads. If the defect is not very pronounced, then it is quite possible to use mother’s milk. For this purpose, special devices are selected that are attached to the chest and close the child’s cleft palate.
- Feeding with a bottle or spoon. If the defect is large and breastfeeding is not possible, you can choose special nipples for the bottle, in which the hole is located not on the top, but on the side, so as to direct a stream of milk into the baby’s mouth and not into the nasal cavity. You can also feed from a spoon, pouring in milk or formula in small portions (the baby must be positioned almost vertically).
Another important point is respiratory protection. Since the air is not heated or humidified in the nasal cavity, before entering the lungs, it is necessary to create an optimal microclimate in the room. A humidifier or household climate control station, which maintains not only air humidity, but also its temperature at a constant level, will help cope with this task. On the street, it is advisable to wear a gauze bandage for such a child.
↑ The main types of plastic surgery used for cleft palate
There are several surgical techniques to recreate the natural shape of the palate. The optimal method or combination of methods is determined by the doctor based on an in-person examination and the individual characteristics of his little patient. In children with cleft palate, the location of the facial muscles is always disturbed and their attachment points are changed. Therefore, the goal of the surgeon, regardless of the chosen technique, will be not only to recreate the barrier between the nasal and oral cavities, but also to give the muscles the correct position so that in the future they can fully perform their functions.
- Veloplasty
Used to eliminate clefts of the soft palate. If the defect extends to bone structures, then veloplasty is performed as the first stage of its closure. During this operation, the surgeon makes fairly large incisions in the mucous membrane, through which he isolates and sutures the muscles that form the main thickness of the soft palate and ensure its participation in the act of breathing, swallowing and sound production. As a result of medical manipulations, the soft palate should have sufficient length and form a velopharyngeal valve (shutter), thanks to which the upper respiratory tract will be protected from food entering them when swallowing.
| Results of operations to remove cleft palate: | |
- Simultaneous plastic surgery of cleft hard and soft palate
This technique involves closing the hard palate defect with soft tissues of the oral and nasal cavities. It is advisable to carry it out only if the child’s cleft is narrow or incomplete. To do this, the tissues of the oral cavity are shifted in such a way as to close the bone defect as much as possible. The tissues of the nasal mucosa are mobilized in the same way. As in the previous case, during one-stage plastic surgery, the muscles of the soft palate are given the correct position, its normal length and velopharyngeal seal are recreated.
| Scheme of incisions and suturing during surgery on the soft (Fig. 1) and hard (Fig. 2) palate: | |
The result obtained will not be final, since simply covering the bone defect with soft tissue is not enough. However, after such an operation, feeding and caring for the child becomes much easier, and the likelihood of developing respiratory diseases, otitis media and sinusitis decreases. In addition, optimal conditions are created for the growth of the bone structures of the upper jaw, due to which after a few months the thickness of the lumen in the hard palate can be reduced to a narrow strip of 2-3 mm and in the future it will be much easier for the surgeon to eliminate it.
- Uranoplasty
Allows you to completely remove the cleft of the hard palate and restore the continuity of its bone structure. To close the lumen, fragments of the periosteum are used: they are moved to the defect area along with the vessels that will supply the transplanted areas with blood. Between the sheets of periosteum, over time, its own bone tissue forms, which finally closes the cleft palate.
It is considered inappropriate to perform uranoplasty on children who have not yet reached one and a half to two years of age, since the intervention can lead to retarded growth of the bones of the upper jaw. In some cases, the operation is postponed for an even longer period - up to 4 years, if the surgeon considers that the conditions for it at an earlier age are unsuitable.
- Cheiloplasty
Surgical lip plastic surgery is used in cases where a child’s cleft palate is combined with a cleft lip. It is usually performed at the first stage of a two-stage velo-cheilouranoplasty. The operation is performed no earlier than 8 months, since before this time the sizes of the lips and nose are still very small, which means there is a high risk of incorrectly matching the tissues and obtaining an unsatisfactory aesthetic result. At the same time, doctors do not recommend over-delaying this plastic surgery, since it creates optimal conditions for the proper development of the entire maxillofacial system, breathing, sucking, swallowing and speech.
| Photos before and after operations: | |
↑ Features of postoperative care
- All of the above interventions are performed under general anesthesia. The child receives antibiotics before surgery, and then painkillers are added to them. Discharge from the hospital occurs on the 5-7th day.
- In the first week, the area of postoperative wounds is usually covered with special napkins with an antiseptic solution. When the stitches are removed, the napkins are also removed. In the future, after each meal you will need to rinse your mouth or spray the mucous membrane with a disinfectant spray. From the second week, on the recommendation and under the supervision of a doctor, it is necessary to carry out a soft finger massage of the palate to accelerate tissue regeneration processes.
- If another stage of the operation is planned, it will be necessary to use a special obturator for a long time to isolate the nasal cavity from the oral cavity (the minimum interval between stages is at least 1 year).
↑ General treatment prognosis
The effectiveness of surgical removal of the cleft palate is very high: complete restoration of the integrity of the soft and hard palate is achieved in 98% of cases. The timing for the operations is selected taking into account the completion of treatment by 6-7 years, so that the defect does not have time to affect the child’s social skills and psyche.
After the correction is completed, disability is immediately removed if it was caused by a cleft palate - as a result, all the troubles are left behind and only almost invisible scars on the inside of the oral cavity will remind you of them.
Orthodontic treatment of cleft palate
In addition to surgery, the assistance of an orthodontist . Medical measures are carried out from the first days after the birth of children with cleft palates until adulthood, and, if necessary, throughout adult life.
Pre-teething period
The primary task is to provide nutrition to the baby so that milk does not enter the mouth and nose during feeding. The problem is solved with the help of specially designed nipples and obturators.
Already at 1–4 months, they begin to correct the shape of the upper jaw using a removable apparatus with a sliding screw. Subsequently, it is replaced with a retention plate that closes the cleft. Before veloplasty, the orthodontist makes a new protective plate for the hard palate.
Period of temporary occlusion
Before uranoplasty, the orthodontist must help the surgeon narrow the cleft of the hard palate. For this purpose, a plate with special devices - pelota - is used. They put pressure on the mucous membrane along the edges of the cleft, irritating it and thereby stimulating the growth of bone tissue.
From 5–6 years of age, the doctor needs to ensure that the jaws develop evenly: restrain the growth of the lower jaw and optimize the growth of the upper one. The first problem is solved by a cap with a chin sling, the second by orthodontic devices for correcting anomalies (activators and regulators).
Mixed dentition period
Before uranoplasty, the orthodontist makes the next protective plate, which is necessary during the recovery stage. After 1–1.5 months, it is replaced with a removable denture with missing teeth.
Replacing baby teeth with permanent ones is the most important time for an orthodontist. Morphological defects worsen, some teeth begin to tilt, overcrowding and crossbite appear. The doctor must diagnose and minimize all these negative changes in a timely manner. At the same time, measures for balanced jaw development are continued.
Period of permanent dentition
At this stage, multibonding systems ( braces ) begin to be included in the process of correcting the bite. Fixed structures help expand narrowed areas of the dentition and correct the position of individual teeth. The upper jaw is also retained: by this time it can already be expanded sufficiently, but the new position is still unstable and requires support. After completing hardware treatment, the teenager should undergo examinations by an orthodontist once every six months [2].
A cleft palate is a serious pathology, but with the coordinated and professional actions of specialists, the defect and its consequences can be completely eliminated. In the future, the person lives a full life, without experiencing discomfort while eating or communicating.
List of sources
- “Cleft palate and cleft lip”, interview with D. A. Grichanyuk, maxillofacial surgeon, Ph.D. // URL: https://www.the-village.me/village/city/people/271423-hirurg (accessed 09/02/2020).
- Special issues of orthodontics. Educational and methodological manual / Tokarevich I. V., Gorbatsevich N. A., Moskaleva I. V., Gorbatsevich D. V., Chernyavskaya M. V., Vasilenko E. P., Kolomiets E. G., Korneeva A. S., Minsk: BSMU, 2012. // URL: https://www.bsmu.by/downloads/kafedri/k_ortodont/3.pdf (access date 09/02/2020).
- Alexandrova L.I. Comprehensive assessment of the results of early preoperative orthopedic therapy taking into account dynamic indicators of the quality of life of children with congenital cleft lip and palate: dissertation. Ph.D. honey. Sciences: 01/14/14 - dentistry. Perm, 2022. // URL: https://www.psma.ru/index.php?option=com_mtree&task=att_download&link_id=218&cf_id=24 (date accessed 09/02/2020).
- Surgical methods of treatment of children with congenital cleft lip and palate: textbook / Chuikin S.V., Davletshin N.A., Averyanov S.V., Chuikin O.S., Ufa: State Educational Institution of Higher Professional Education "Bashkir State Medical University of Roszdrav" , 2011. // URL: https://library.bashgmu.ru/elibdoc/elib491.pdf (accessed September 2, 2020).
The operation is over. What's next?
The baby is prescribed treatment aimed at preventing the occurrence of rough postoperative scars of the upper lip. Scars worsen the aesthetics of the face, limit the mobility of the upper lip, which causes impaired articulation and deformation of the dentition. Physical therapy will help prevent such scars.
If the cleft lip is deep and extends into the nasal cavity, then during the postoperative period the child should wear a “nasal liner” (endonasal retainer). This is a device that creates the correct shape of the child’s nostril on the side of the cleft. The retainer is a conical tube formed along the outer edge, in the shape of a healthy nostril. The retainer is made by the orthodontist before surgery.
Children with congenital clefts need regular examinations by an otolaryngologist because they are three to four times more susceptible to ENT diseases due to abnormal communication between the mouth and nasal cavity.
Regular visits to the dentist will ensure timely sanitation of the mouth. This is an important condition for successful rehabilitation.
An important stage in the rehabilitation of a child with a cleft is sessions with a speech therapist.
Olga Legostaeva, speech therapist at the Rehabilitation Center for Speech Development at the Institute of Congenital Diseases of the Maxillofacial Region, Professor Gonchakov, explains exactly what kind of help speech therapists can provide:
“90% of children with facial clefts need speech therapy help. Sometimes such children are diagnosed with “rhinophonia” - the so-called “nasality”, the pronunciation of sounds “in the nose”. Sometimes - “rhinolalia” (voice disturbance, nasalization plus specific pharyngeal pronunciation, some sounds are replaced by exhalation through the nose, speech becomes completely incomprehensible). Sometimes, if a cleft is one of the signs in the structure of a particular syndrome (Pierre Robin syndrome, etc.), delayed speech development is possible. But even in this case, the prognosis can be favorable.
An important point is that working with those children who had facial clefts differs from working with other disorders. Often children come to us whose parents complain: “We have been working with the child for two or three years, no results. - What are you doing? - Speech therapy massage. But in this case it is not necessary to do a massage. If the child is not breathing properly, the massage will be of no use.
The most effective in this case are breathing exercises and exercises for the formation of the velopharyngeal ring.
Breathing exercises are needed to teach your child to breathe using the diaphragm and abdominal muscles. Our children with clefts usually use their collarbones and shoulders to breathe. If you teach a child to use the abdominal muscles, take a deep breath through the nose and exhale strongly through the mouth, and open the mouth correctly, correct breathing will be formed. Then it will be easy to put sounds.
The second set of exercises is necessary in order to develop the muscles of the velopharyngeal ring. Due to physiology, our children cannot close their throats, so when they phonate, the air goes into their nose. But such simple exercises as coughing, yawning, swallowing liquid in small portions, arranged in a certain system, help develop the velopharyngeal ring and create the conditions for good sound. Vocal phonopedia perfectly develops the palate.
This work is not quick, it is long, painstaking work that requires the constant participation of parents. Parents are always present at our classes; they not only write down the lessons in a notebook, but also learn how to correctly present tasks to the child and ensure that he completes them correctly.
You should start classes as early as possible. We don’t have the concept of “started studying too early.” If a child does not speak after surgery at two to two and a half years old, this is a reason to see a speech therapist. If he is three years old and speaks “in his nose,” this is also a reason to see a speech therapist.
In my experience, three-year-olds are much easier to deal with than five-year-olds. Five-year-olds have quite a long speaking experience. And in order to correct their speech defects, they have to be “broken.” Three year olds are more flexible. Therefore, I recommend starting to practice as early as possible. Usually, if we start teaching a child at three years old, by the age of five or six he no longer has problems with pronunciation. At an early age, many speech problems can be corrected.
It is only important to understand that the rehabilitation of children with facial clefts must be comprehensive. A facial cleft is not only an anatomical defect, it is a defect that impairs breathing, hearing, and speech. Therefore, when working with such children, a speech therapist alone is not enough. In our center, for example, there is a team that includes a speech therapist, a phonologist and a psychologist.”
A phonopedist is a speech pathologist who restores physiologically correct sound production.
Natalya Borisovna Silkina is a phonopedist; for three years she worked at the Rehabilitation Center for Speech Development at the Institute of Congenital Diseases of the Maxillofacial Region, Professor Gonchakov.
“90% of children with facial clefts hear worse than ordinary children,” says Natalya Borisovna. — Their hearing loss occurs due to the fact that they do not hear all frequencies. This defect can be eliminated with the help of exercises to develop phonemic hearing (starting from two years), and with the help of vocals.
It is best if the mother sings with the baby. Always. At trainings, we teach mothers to sing continuously, almost around the clock. Only in this case do the kids begin to sing on their own. The fact is that such children are not able to perceive those songs that sound from electronic media. The speed is too high. For them it is background, noise.
Moreover, it is better to talk to them slowly and loudly, pronouncing the words clearly: they will not hear enough. Therefore, when I practice with them in the center, I pronounce everything and sing it five times slower.
Older children can be taken to a vocal studio. Vocal exercises stretch tissues and relax the apparatus. The palate is the same muscle, only its sensitivity is reduced due to the suture. Vocal exercises allow you to gently work this muscle. But ideally, vocals should be studied with a phonopedist who knows the features of rhinolalia and rhinophony.”
How does the procedure work?
Palatoplasty to remove clefts is performed using a standard set of surgical instruments. This technology is called Z-plasty or Furlow plastic. It consists of sequentially isolating and stitching triangular flaps of the mucous membranes of the oral and nasal cavities, taking into account all the anatomical features of the structure of these structures. Veloplasty is usually accompanied by other types of surgical operations aimed at the correct formation of the hard palate and lips.
A surgical solution to snoring problems involves the surgeon excision of part of the soft palate and removal of the uvula, but more advanced methods are now being used to solve this problem.
Using a laser after preliminary anesthesia, the doctor makes small wounds, which, as they heal, lift the soft palate. The essence of cryotherapy is exactly the same, except that the operation is performed using a cryoapplicator. Radio wave therapy is the most gentle and effective method. All these procedures usually do not require hospitalization and are carried out within 10-15 minutes. The rehabilitation period is individual.