Oral leukoplakia is a disease that affects the mucous membrane and is characterized by its visual and structural changes.
In the initial stages, the pathology is manifested by keratinization and a whitish coating of the mucous membrane of the palate, gums, tongue, and the inside of the cheeks. In the future, the disease can “degenerate” into a malignant tumor formation.
Causes
Experts identify several main factors that provoke the development of oral leukoplakia. Most often, the cause of the disease is thermal damage or chemical irritation of the mucous membrane. A similar effect is caused by smoking (smoker's leukoplakia), drinking alcohol, and eating disorders (excess spicy, excessively hot, sour foods).
The most dangerous is the so-called smoker's leukoplakia, which is common among adult patients. Smoking provokes the occurrence of several forms of pathology at once and increases the risk of cancer.
Other factors that provoke the development of leukoplakia include:
- Mechanical injury with damage to the epithelial layer. This may include a bruise, gum burn, tongue biting, malocclusion, chipped teeth, incorrectly placed correction systems, for example, braces.
- Formation in the oral cavity of an environment favorable for the development of the disease. This is the galvanic environment that occurs in the presence of metal crowns. Metal oxidation provokes persistent irritation of the mucous membrane and degeneration of the epithelial layer.
- Leukoplakia can result from the use of a number of medications, a lack of vitamin A, and iron.
- The pathology is provoked by a number of diseases of the internal organs: diseases of the digestive tract, pathologies of the endocrine system (hormonal imbalances, diabetes). Hereditary factors also influence the development of the disease.
Electrocoagulation
Treatment using electrocoagulation is one of the cheapest. However, today few doctors recommend this traumatic procedure. The fact is that during electrosurgery the surrounding healthy tissues are also damaged, healing occurs very slowly and there remains a risk of recurrence of the disease and its further spread.
For example, leukoplakia of the oral mucosa can develop into a lesion of the larynx if the affected areas were not completely cauterized. And since leukoplakia of the throat is much more dangerous than damage to the oral mucosa, it is better to choose treatment that guarantees a 100% recovery result.
Symptoms of oral leukoplakia
Symptoms of oral leukoplakia vary depending on the degree of development of the pathology. General symptoms are expressed in the following manifestations:
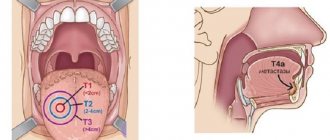
- The initial stage is characterized by the appearance of a gray-white or whitish coating, which is formed from dead epithelial cells. Small numbers of lesions are concentrated on the tongue, gums, palate, cheeks from the inside, lips, and in the sublingual area. On palpation, keratinization of the mucous membrane and compaction in the area of plaques are felt.
- The development of pathology is accompanied by the growth of lesions, their size increases in comparison with healthy epithelium. Over time, keratinized plaques become more sensitive and painful.
- The growth of spots is accompanied by a feeling of tightness, dryness and hard roughness. The sensations intensify under the influence of any irritant.
The uncontrolled course of leukoplakia leads to its persistent progression and the appearance of painful ulcerative and erosive lesions.
Leukoplakia in adults: what is it and what does it look like?
Symptoms of leukoplakia do not appear immediately. At first, minor swelling areas may appear, usually on the inside of the cheeks. The affected area can be one or several, sometimes their number increases. The patient feels roughness when touching the affected areas with the tongue; they can cause severe discomfort (itching and burning). Quite often, despite the presence of painful symptoms, patients are extremely dismissive of the manifestations of leukoplakia, turning to them only in the later stages of the disease.
As it progresses, the affected areas become covered with a hard white coating, which is easily removed, but appears again after a while. They do not cause painful sensations. It is noted that the pathology is often accompanied by fungal infection; and a tenth of cases become harbingers of cancer. In this case, leukoplakia of the oral mucosa usually remains at the stage of benign tumors, but leukoplakia of the tongue (pictured) or located in the lower part of the mouth is much more dangerous.
The main symptoms of the disease include:
- the appearance of papillary-shaped neoplasms;
- thickening of the area where the inflammation is located;
- rapid increase in the affected area;
- frequent injury and bleeding of diseased areas;
- development of erosions, ulcers, white crust,
- significant enlargement of lymph nodes.
Types and forms of oral leukoplakia
The main forms of oral leukoplakia:
- Flat.
- Verrucous.
- Erosive.
- Tappeiner's leukoplakia.
- Soft.
Oral flat leukoplakia
The most common type of disease is flat or simple oral leukoplakia. It is often characterized as the initial stage of a pathological condition. At this stage of development, the pathology does not manifest itself as severe pain.
Photo: leukoplakia of the tongue
The initial phase of the disease is accompanied by the appearance of whitish or gray-white plaques, irregularly shaped stripes located on the tongue, palate, inner surface of the cheeks, and in the corners of the mouth. The plaques are dry and rough, without pronounced elevation or hardening. You often feel tightness, burning, and excessive dryness in the area of the damaged areas.
Simple leukoplakia often affects the tongue, resulting in a decrease in its sensitivity and taste perception.
Inflammatory processes do not occur at this stage of development of the disease. In most cases, this type of pathology occurs without deterioration in general well-being or complications and can accompany a person throughout life.
Verrucous form
The uncontrolled course of leukoplakia with constant traumatic effects on the mucous membrane - irritation from chipped teeth, incorrect dentures, consumption of excessively hot food and liquid - provokes its development and transformation of the simple form of the disease into verrucous.
The dominant sign of the transformation of simple leukoplakia into verrucous is pronounced keratinization and elevation of the upper layer of epithelial cells of the affected area. At this stage of the disease, the plaques noticeably rise above the healthy epithelium; upon palpation, compaction is clearly felt.
Verrucous leukoplakia of the oral cavity is accompanied by a pronounced feeling of tightness and dryness, and the occurrence of painful sensations during eating.
According to external signs, leukoplakia is of two types:
- Plaque. Plaque areas appear on the oral mucosa. Plaques are characterized by pronounced roughness, density, and elevation above the healthy epithelium. Their color varies from milky to bluish.
- Warty. Lesions similar to warts appear on the mucous membrane. Compared to the plaque form of the disease, the wart is characterized by the appearance of more keratinized, lumpy compactions. The formations rise 2–3 mm above healthy epithelial cells and most often have a gray-white tint.
The verrucous form of the disease more often than others turns into a malignant lesion of the mucosal epithelium.
Erosive stage
The erosive form of the disease occurs with its progression and prolonged exposure to negative factors on epithelial tissues. This stage of oral leukoplakia is accompanied by a number of symptoms:
- Severe pain occurs, which intensifies when any type of irritant comes into contact with the lesion. Eating food, alcohol and hot drinks provokes pain.
- Externally, the disease is manifested by the appearance of cracks and ulcers and erosive lesions in the affected areas. Inflammatory foci are localized around erosive lesions, often accompanied by bleeding.
- Unpleasant sensations persist even at rest. There is a burning sensation, excessive dryness and roughness. The development of a lesion at the base of the tongue causes a sore throat and speech impairment (coughing occurs).
This type of pathological condition has the highest risk of relapse. The erosive stage of the disease is very difficult to treat; ulcerative lesions take a very long time to heal.
Soft oral leukoplakia
This type of pathology is a benign neoplasm. The main prerequisites for the development of soft leukoplakia of the oral cavity are hormonal imbalances, disturbances in the psycho-emotional background, and chronic fatigue.
Visually, a slight elevation of white plaques above the healthy epithelium is noted. The formations are rough and painless. There is slight compaction and dryness of the affected tissue. When the lateral surfaces of the tongue are affected, sensitivity to temperature influences decreases, and taste perception is impaired.
The mild form of pathology is divided into several more varieties:
- Partial (focal), manifested by the appearance of affected areas in the form of foci localized in certain places.
- A diffuse variety, characterized by the “spreading” of plaques over the entire surface of the mucosa. The formations have a spongy, porous surface, loose structure, and increased size. The lesions are painless, but interfere with talking and eating, creating the feeling of “extra” tissue.
Tappeiner's (smoker's) leukoplakia
Adult patients, especially long-time smokers, are most susceptible to this form of the disease. Tappeiner's leukoplakia is provoked by tobacco decay products and chemical irritation of the mucous membrane by tobacco smoke.
In most cases, the formations affect the palate and the gum tissue located next to it. Large folded plaques of brown or grayish color appear in the oral cavity. The affected areas are painless.
The appearance of formations leads to blockage of the salivary glands and the appearance of reddish nodules. This condition causes excessive dry mouth and “thick” saliva.
It is not difficult to treat this type of leukoplakia in the oral cavity. It is necessary to give up smoking by first reducing your consumption and then stopping smoking completely. Getting rid of a negative habit leads to the complete disappearance of the pathological condition.
Causes
Different localizations of leukoplakia are caused by different reasons and require an individual approach in developing a treatment strategy.
Hairy leukoplakia develops against a background of reduced and weakened immunity, so most often this type of disease is diagnosed in patients with HIV, various immunodeficiencies and during rehabilitation after organ transplantation, when a course of immunosuppressants is prescribed.
- Leukoplakia of the external genitalia in women develops most often during menopause, when reverse development processes occur in tissues and cells. Mucous tissues and skin become drier, hair loss is observed, which is a normal physiological process.
- Leukoplakia of the esophagus develops after heartburn or burns of the mucous membrane of this organ; more than half of the cases of this disease cause the appearance of a cancerous tumor.
- Leukoplakia in the oral cavity is most often localized on the mucous membranes of the inner side of the cheek, the hard and soft palate, as well as in the angular folds of the mouth. Leukoplakia of the tongue is extremely rare in medicine.
To this day, official medicine does not know the exact reasons for the development of this disease in the mouth. However, a number of factors have been identified that increase the chances of developing leukoplakia:
- metabolic disorders;
- genetic predisposition;
- lack of vitamin A;
- smoking;
- chronic injuries to the mucous membranes (for example, due to improperly manufactured dentures);
- activities associated with direct contact with coal and coal tar, as well as their processing processes;
- HIV and AIDS;
- chronic inflammatory processes in the mouth associated with neurological disorders.
Leukoplakia of the bladder is a protracted chronic disease that is characterized by the degeneration of transitional epithelial cells into squamous epithelial cells. The keratinized epithelium is unstable to urine components, which causes inflammation in the bladder cavity. The main cause of the development of the disease is ascending infection with sexually transmitted pathogens. Therefore, leukoplakia in the bladder develops more often in women - their urinary canal is much shorter than the male one, so it is easier for infections to penetrate through it.
In some cases, the cause of leukoplakia can be a downward infection, when a pathogen penetrates through the bloodstream from nearby organs: staphylococci, Proteus, streptococci, E. coli and others. The development of the disease is favored by:
- chronic diseases of the abdominal organs located next to the bladder;
- all factors that reduce immunity: hypothermia, stress, bad habits, chaotic lifestyle;
- foci of chronic inflammation located at a distance from the bladder: tonsillitis, caries, sinusitis, etc.;
- disturbances in the functioning of the endocrine system;
- the IUD was not removed in time in the uterine cavity;
- promiscuous sex life without the use of barrier contraception.
Leukoplakia of the cervix is called whitish formations (spots or plaques) that appear on the mucous membrane. To diagnose the disease, a preventive examination using a gynecological speculum is sufficient.
Like dysplasia, cervical leukoplakia requires mandatory treatment, since it is a precancerous disease. There are many reasons for the appearance of such tissue changes:
- decreased immunity for various reasons;
- injuries due to careless examination, termination of pregnancy, childbirth;
- interruptions in the functioning of the endocrine system;
- ovarian dysfunction;
- current or previous infectious diseases of the genital organs.
Diagnosis of the disease
The diagnosis is made based on examination and questioning of the patient. Mandatory diagnostic studies confirming the diagnosis include:
- Cytology is the collection of epithelial cells to identify cancerous lesions.
- Histology is taken to perform a biopsy, which allows examination of the affected epithelial tissue to detect cancer cells.
- Blood from a vein.
Additional clarifying studies make it possible to distinguish leukoplakia from other pathologies.
Prognosis and complications
The disease progresses rather slowly, i.e. represents a sluggish pathology, with periods of subsidence and increase in symptoms. But it is important that in the absence of treatment for oral leukoplakia , the disease is constantly growing and irreversible (that is, it does not go away on its own). The gradual transition (degeneration) into inhomogeneous forms is a transition to a precancerous state and even the onset of oral cancer.
The simple, most common form of leukoplakia (homogeneous form) degenerates quite rarely and practically disappears with treatment and elimination of provoking factors (for example, permanent damage to the mucous membrane by orthopedic structures). But other forms of the disease, such as oral verrucous leukoplakia, have a high risk of becoming cancerous. Therefore, even after successful treatment of oral leukoplakia, certain precautions and prevention must be taken, since this disease has a tendency to return.
Classic treatment of oral leukoplakia
The choice of treatment method for oral leukoplakia depends on the symptoms, the form of the pathology, and its severity. Initially, it is necessary to eliminate the negative factors that provoke the onset of the disease: giving up bad habits, changing your diet.
Photodynamic therapy
A number of physical procedures can be used to effectively treat the disease in a hospital. Such events include:
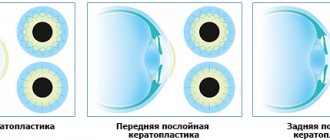
- Diathermocoagulation intervention to remove keratinized plaques. After a course of procedures, healing of the mucous membrane occurs within 10 days.
- Freezing the affected epithelial layer of the oral cavity (cryodestruction) for 1 minute. The course of treatment is 1 week.
- Carrying out photodynamic therapy (PDT). Pathogenic cells are destroyed by irradiation with a light wave.
The treatment regimen includes taking medications aimed at stopping infectious processes and inflammation. Local treatment of the mucous membrane is mandatory.
Features of treatment of leukoplakia of the tongue
When the disease is localized in the tongue, sanitation of the oral cavity is mandatory. If there are incorrectly installed dentures, fillings, or chips on the teeth, the fillings, dentures are polished (or replaced), and chipped teeth are restored. The affected areas are treated with antiseptics and wound healing solutions.
The flat form of the disease is easily treated. Sometimes it is possible to eliminate pathological plaque through laser or radio wave therapy. But if a patient is diagnosed with malignant tumors, treatment will be carried out in two stages - first, surgery is performed, then long-term radiotherapy is performed.
Upon completion of the treatment course, the patient should remain under outpatient observation, since leukoplakia of the tongue is characterized by a sluggish course, and symptoms of the disease may appear over several years.
How to treat hairy leukoplakia
Before starting treatment, you need to conduct a number of studies. The patient is referred to a therapist at the clinic. There, the doctor can prescribe laboratory tests: biochemical blood test, testing for sexually transmitted diseases, etc.
If a person is diagnosed with HIV infection, antiretroviral therapy is administered. With long-term use of drugs, the patient’s well-being improves, and the disease in the mouth goes away.
The dental clinic provides oral examinations, dental diagnostics, and professional hygiene. If sharp edges of fillings or failed prostheses are detected, they are replaced. Treatment of caries and its complications is carried out. Recommendations are given for home dental care: personal hygiene products (brushes, pastes, dental floss, rinses) are selected.
Keratolytic drugs are suitable for local treatment. In advanced cases, they resort to surgical manipulations: excision of the affected areas with a laser.
Treatment of oral leukoplakia at home
At home, treatment of leukoplakia of the oral cavity and tongue must begin with proper hygiene procedures. You need to use toothbrushes with soft bristles. Brushing your teeth and tongue should be done smoothly, without excessive intensity. After each meal, rinses and applications with anti-inflammatory and restorative properties are used. Particularly careful hygiene is required when treating leukoplakia of the tongue.
The affected areas must be treated with antiseptics: Chlorhexidine, Furacilin. Irrigation with antiseptic solutions is carried out up to 5 times a day. Taking vitamin complexes containing vitamins A and B groups helps to cure the pathological condition at home.
Folk remedies can be used as additional treatment. Decoctions of sage, chamomile, and calendula, which have an anti-inflammatory and calming effect, are considered particularly effective. A positive result is achieved by treating the affected areas with sea buckthorn oil and Kalanchoe juice.
Adult patients are recommended to consume natural juices, which have a general strengthening effect that increases immunity. Similar drinks include juices from apples, carrots, and cabbage. It is recommended to dilute freshly squeezed drinks with water.
Oral leukoplakia is a pathological condition that should not be left to chance. When the first signs of pathology appear, you must consult a specialist; self-medication is fraught with the development of serious complications and consequences.
Causes of oral leukoplakia
- taking strong medications (in particular, antibiotics, as well as constant use of drugs of various spectrums of action in large quantities);
- smoking, as harmful components penetrate through cigarettes and deplete the mucous membrane;
- poor nutrition and abuse of spicy, salty and sour foods;
- chronic gum disease in an advanced stage;
- abundant carious lesions of teeth;
- incorrectly placed fillings;
- incorrectly selected dentures that cause an allergic reaction;
- alcoholism;
- hormonal changes;
- bite problems;
- diabetes;
- HIV infection;
- avitaminosis;
- diseases of the stomach and intestines;
- stress;
- hereditary predisposition;
- unfavorable environmental conditions;
- harmful production activities.
Typically, at the initial stage, oral leukoplakia can be completely asymptomatic. That is why it is very important for people who are susceptible to risk factors to undergo regular dental examinations for prevention. The 32 Dent dental network will help you, even if the disease is in an advanced stage.