- Risk factors for developing lip cancer
- Pathomorphology
- Diagnosis of lip cancer
- Prognostic factors
- Clinical picture
- Lip cancer treatment
- Disease prognosis
- Rehabilitation
- Prevention of lip cancer
Lip cancer is a malignant tumor of the stratified squamous epithelium of the red border of the lower and upper lips. Cancer of the upper lip in relation to cancer of the lower lip is 2-5% and is observed more often in women.
In the structure of incidence in relation to all malignant tumors, lip cancer is 1.8% in men and 0.53% in women. Among the CIS countries, this figure is the highest in Tajikistan: 2.7% for men and 1.5% for women, the lowest is for men in Azerbaijan - 0.6% and women in Armenia - 0.4%.
The standardized incidence rates for lip cancer in Russia in 2000 for men were 5.7; for women – 1.6; and the average age of sick men is 64.6 years; women – 72.3 years. During the period from 1990 to 2000, the incidence of lip cancer decreased from 7.5 to 4.6 in men and from 1.1 to 0.73 in women per 100 thousand inhabitants of Russia.
Risk factors for developing lip cancer
In almost all patients, the appearance of lip cancer is preceded by various background processes and precancerous conditions of the lip mucosa. The etiological factors causing lip cancer are:
- Long-term exposure to adverse meteorological factors (solar radiation, wind, sudden fluctuations in air temperature, ionizing effects).
- Exposure to carcinogenic substances of endogenous and exogenous nature.
- Bad habits: smoking, alcohol, chewing various mixtures (us, betel, etc.).
- Injuries to the red border of the lips: mechanical: carious teeth, sharp edges of tooth roots, tartar, incorrectly made dentures, biting the lip, pressure from a tube, mouthpiece, cigarette or cigarette;
- chemical carcinogens of tobacco: compounds of arsenic, mercury, bismuth; anthracite, liquid resins, petroleum distillation products from persons of relevant professions;
- thermal: burns from hot food, cigarettes.
Depending on the pathological changes in the red border, precancerous diseases with a high frequency of malignancy (15-30%) are obligate and with a low frequency of malignancy (6-10%) - facultative, as well as background processes.
Obligate precancers: warty precancer, limited hyperkeratosis, Manganotti cheilitis.
Optional precancers: verrucous leukoplakia, keratoacanthoma, cutaneous horn, papilloma with keratinization, erosive-ulcerative and hyperkeratotic forms of lupus erythematosus and lichen planus, post-radiation cheilitis.
Background processes: flat leukoplakias, chronic ulcers and fissures of the lips, atmospheric and actinic cheilitis.
Treatment of cheilitis, lupus erythematosus and lichen planus is medicinal with mandatory microscopic monitoring if there is no effect.
Treatment of other pathological changes is carried out by cryogenic, surgical, laser and photodynamic therapy.
Precancerous diseases of the red border of the lips (RBL) and oral mucosa (ORM)
I. K. Lutskaya
Doctor of Medical Sciences, Professor, Head of the Department of Therapeutic Dentistry BelMAPO (Minsk)
Diseases characterized by a high tendency to malignancy (obligate precancers of the oral mucosa and red border of the lips) require special consideration in dental practice. They are characterized by the absence of objective signs of a cancerous tumor, but in the presence of pathogenic factors they become malignant. The clinical manifestations of this group of diseases are quite diverse, which makes their diagnosis difficult. On the other hand, the prognosis depends on a number of factors, primarily the nature of the carcinogens, as well as the local status and general condition of the body. If adverse effects are excluded, reverse development of the lesion elements, stabilization of the process without significant changes, or further development without a tendency to degeneration are possible. The persistence of an unfavorable background leads to malignancy of the lesion.
The main signs of malignant degeneration can be the following symptoms: a sharp change in the clinical picture, namely acceleration of the development of a tumor or ulcer, exophytic growth or ulceration of the tumor (Fig. 1).
Rice. 1 a. Signs of malignancy.
Rice. 1 b. Signs of malignancy.
The next signal points are bleeding of the lesion, the appearance of hyperkeratosis, infiltration and compaction at the base (Fig. 2). The lack of effect of conservative treatment within 7-10 days is the basis for referring the patient for consultation to an oncologist or maxillofacial surgeon. Malignancy is confirmed by the results of morphological studies, namely the identification of atypical cells in the biopsy material.
Rice. 2. Bowen's disease.
Systematics of keratoses as precancerous conditions
I. Keratoses without a tendency to malignancy (initial form of leukoplakia, soft leukoplakia, geographic tongue, etc.).
II. Optional precancer with the possibility of malignancy up to 6% (flat form of leukoplakia, hyperkeratotic form of lichen planus; pemphigoid form of lichen planus, etc.).
III. Optional precancer with a tendency to malignancy (malignancy tolerance) from 6 to 15% (elevating form of leukoplakia; warty form of leukoplakia; erosive form of leukoplakia; warty form of lichen planus; erosive form of lichen planus; rhomboid glossitis - hyperplastic form, etc.).
IV. Obligate precancerosis with the possibility of malignancy over 16% (ulcerative form of leukoplakia; keloid form of leukoplakia; ulcerative form of lichen planus; follicular dyskeratosis; Bowen's syndrome; atrophic keratosis; xeroderma pigmentosa, ichthyosis vulgaris, etc.).
Bowen's disease
Bowen's disease has the highest potential risk of malignancy (Bowen, 1912), since its histological picture is cancer in situ (intraepithelial cancer without invasive growth). Clinical manifestations of Bowen's disease vary depending on the location, stage of the disease, and associated factors. The patient's complaints can be reduced to discomfort, roughness of the corresponding parts of the mucous membrane, more or less pronounced itching. In some cases, there are no subjective sensations, so the lesion will be detected during a routine examination of the oral cavity.
The favorite localization of lesion elements in the form of spots, papules, scales, erosions, and areas of keratinization are the posterior sections of the mucous membrane: the palatine arches, the root of the tongue. Clinical manifestations of the disease on the cheeks, lateral surface of the tongue, and soft palate are described. More often one, less often two or three areas of altered mucosa are found.
Most typical for the initial stages of the disease is the appearance of a limited area of hyperemia, which has a nodular-spotted or smooth appearance (Figure 3). A distinctive feature may be the peculiar velvety surface as a result of small papillary growths. The further clinical picture resembles leukoplakia or lichen planus due to the formation of areas of hyperkeratosis. There is a tendency to erosion. The lesion will rise above the level of surrounding tissues if nodules form and merge into plaques. With a long course, atrophy of the mucous membrane develops, and in such cases the affected area seems to sink.
Diagnosis is difficult when a small focus of hyperemia subsequently becomes covered with scales, resembling leukoplakia or lichen planus in appearance. The diagnosis of Bowen's disease is made on the basis of a histological picture: giant cells with an accumulation of nuclei in the form of lumps, the so-called monstrous cells, are found in the spinous layer.
The prognosis of the disease is unfavorable: the development of lesions within 2-4 months ends with invasive growth without a tendency to regression (reverse development).
Treatment for Bowen's disease involves complete excision of the lesion, which may include surrounding healthy tissue. In some cases, close-focus X-ray therapy is used.
Warty precancer
Warty precancer is an independent clinical form (A. L. Mashkilleyson). It is characterized by a pronounced tendency to malignancy: already 1-2 months after the onset of the disease. The patient's complaints boil down to the presence of a cosmetic defect and discomfort. The favorite localization of the lesion (usually single) on the red border of the lower lip allows for a detailed study of the clinical picture. The main element of the lesion is a nodule with a diameter of up to 10 mm, protruding above the level of the mucosa and having the usual color of the red border of the lips or a persistent red color (Fig. 4). The surface of the nodule may be covered with thin, tightly attached scales that cannot be removed when scraped. The tissue surrounding the lesion is not changed. Upon palpation, the compacted consistency of the nodule is determined, there is no pain.
Differential diagnosis with a wart, keratoacanthoma, papilloma is carried out on the basis of the clinical picture with mandatory pathological confirmation. Clinically, a common wart is characterized by a lobulated structure or papillary growths with a rim of stratum corneum along the periphery. Keratoacanthoma is characterized by a large number of keratinized cells filling the depression in the form of a funnel formed by a dense ridge of surrounding hyperemic mucosa. The papilloma has a stalk of soft consistency.
Treatment of warty precancer is only surgical with complete excision of the lesion and histological examination of the tissue. Confirmation of warty precancer is the proliferation of the epithelium due to the spinous layer both towards the surface and deep into the mucosa.
Rice. 3. Warty precancer.
Limited precancerous hyperkeratosis
As an independent disease, limited precancerous hyperkeratosis has a less pronounced degree of malignancy than warty precancer: the lesion can remain in a stable phase for months, even years. However, clinical signs of malignant degeneration are very unreliable, since increased keratinization processes, the appearance of erosion and compaction can be detected some time after the onset of malignancy. Therefore, the basis is histological examination. The patient makes no complaints or indicates a cosmetic defect. The characteristic localization of an area of altered polygonal mucosa on the red border of the lips makes it possible to diagnose limited hyperkeratosis. The grayish lesion may sink or rise above the surrounding unchanged red border without spreading to the skin or Klein's area (Fig. 5). The elevation of the lesion above the level of the lip is associated with the layering of scales, which cannot be removed when scraped. On palpation, the compaction at the base is not detected, but the dense consistency of the surface of the lesion is felt.
It is necessary to differentiate limited precancerous hyperkeratosis from leukoplakia, lichen planus, and lupus erythematosus. A diagnostic sign can be the lesion itself, which is small in size from a few mm
up to 1.5
cm
of polygonal shape with a tendency to form scales on the surface, which is not typical for leukoplakia. When localized on the lip, lichen planus is characterized by hyperemia, infiltration, whitish stripes, spots, and significant prevalence. With lupus erythematosus, inflammation, atrophic scars, and often erosion and diffuse damage to the red border are detected. Since histological examination is critical for the diagnosis of malignancy, biopsy should be performed as early as possible.
Treatment of limited hyperkeratosis consists of surgical removal of the lesion within healthy tissue; wedge-shaped excision is advisable. It is mandatory to exclude local irritants and bad habits: smoking, lip biting.
Rice. 4. Limited hyperkeratosis.
Abrasive precancrosis cheilitis Manganotti
The disease was first described by Manganotti (1913) and is considered in the group of obligate precancers due to its tendency to malignancy. It differs from other diseases of this group in its long course, tendency to regression (remissions), reappearance and development. Degeneration may occur after several months or many years.
A single lesion (rarely there are two) is localized on the red border of the lips in the form of oval or irregularly shaped erosion (Fig. 6). The surface of the erosion, having a bright red color, looks polished, can be covered with a thin layer of epithelium and does not tend to bleed. Drops of blood can be detected when crusts or crusts (serous, bloody) are separated, which can appear in the form of layers on the surface of erosions.
Rice. 5. Heilith Manganotti.
The element is localized on the unchanged red border of the lips. In some cases, congestive hyperemia and infiltration can be detected, but the background inflammation in Manganotti cheilitis is unstable.
Palpation does not detect changes in tissue consistency or pain. A feature of the clinical course of the disease is its intermittent nature: once it appears, erosion can spontaneously epithelialize, and then reappear in the same or another place, limited in size from 5 to 15 mm
.
It is necessary to differentiate Manganotti cheilitis from erosive-ulcerative forms of hyperkeratoses (leukoplakia, lichen planus, lupus erythematosus), herpetic lesions at the erosion stage, pemphigus, erythema multiforme. It is based on a characteristic picture of bright red erosion, often oval in shape, without bleeding or with the formation of bloody crusts on the surface. There are no lesions characteristic of hyperkeratosis in the form of spots, papules, stellate scars, or persistent hyperemia. In contrast to vesicular and vesicular lesions, fragments of blisters and specific cells are not identified (with pemphigus, herpetic stomatitis).
Erythema multiforme is characterized by an acute onset and pronounced prevalence of the process. Erosion in herpetic stomatitis is distinguished by scalloped edges as a result of the fusion of vesicles. If you have the habit of biting a portion of your lip, swelling and hyperemia are clearly visible, and signs of inflammation may transfer to the skin. Upon examination, individual point erosions or erosions merging into one are determined. Frequent lip biting confirms the traumatic nature of the disease. The history, as a rule, reveals a primary lesion in the form of a herpetic, mechanical, chemical, etc. lesion.
In doubtful cases, a histological examination is carried out, the diagnosis is confirmed by detecting epithelium infiltrated with histiocytes, lymphocytes, mast cells, as well as changes in the spinous layer and connective tissue.
Treatment of Manganotti cheilitis includes general and local treatments. Vitamins are prescribed internally to stimulate regeneration processes. Drugs that have an epithelializing effect are used locally: oil solutions of vitamins A, E, methyluracil, solcoseryl. In the presence of background inflammatory phenomena, it is possible to use corticosteroid ointments.
Conservative treatment of Manganotti cheilitis in the absence of signs of degeneration and a positive effect (the onset of stable remission) can last 2-3 months. Frequent recurrence, clinical growth, especially the appearance of the slightest signs of malignancy serve as an indication for surgical treatment (removal of the lesion within healthy tissue) with histological examination of the material.
Eliminating bad habits, irritating factors, and sanitation of the oral cavity are mandatory.
Tactics of a dentist
| Possible situations | Dentist tactics |
| Local manifestations in the presence of a local etiological factor: traumatic injuries, Vincent’s ulcerative necrotizing stomatitis | - diagnostics and treatment at the dentist — additional research is possible - therapy is usually local |
| Local manifestations in the presence of a common cause: chronic recurrent herpetic stomatitis, fungal infections, erythema multiforme | — diagnosis and treatment by a dentist after additional research and consultation with a specialist — local therapy, general therapy is possible |
| Local lesions against the background of general diseases: diseases of the gastrointestinal tract, cardiovascular system; allergic reactions, neurogenic and endocrine disorders; childhood infections, radiation sickness, myocardial infarction, blood diseases, tuberculosis, pemphigus | - dental examination — the final diagnosis is made by a doctor specializing in the field of this disease (hematologist, dermatovenerologist, allergist, etc.) - treatment by a specialist in the profile of pathology - general (etiotropic, pathogenetic), by a dentist - local, often symptomatic |
Particular vigilance should be exercised in cases of detection of a possible social risk or threat to the patient’s life. Depending on the specific clinical situation, the dentist bases his actions, including the following general rules.
- Each patient is admitted using personal protective equipment and sterile instruments.
- The initial examination of the oral mucosa is carried out only using instruments (mirror, probe, spatula, tweezers). Before special studies (serological, bacteriological, cytological) are carried out, the elements of the lesion are not palpated.
- In all doubtful cases, which include the primary detection of lesions on the mucous membrane or the lack of effect of treatment for a previously detected soft tissue change, the patient must be examined for syphilis and HIV infection. This recommendation is due to the fact that even a clinically clear local picture of the disease can accompany a general severe or infectious disease (for example, herpetic eruptions in AIDS, aphtha-like plaque in syphilis).
- Identification of positive serological blood reactions to syphilis or detection of Treponema pallidum in the lesion elements serves as an indication for treatment of the patient in a specialized institution. The situation is similar when identifying the causative agent of tuberculosis. HIV-infected people are served in AIDS centers, but they can also receive the necessary help from a dentist, which every outpatient doctor should remember.
- The initial detection of an ulcer with hardened edges or the lack of effect of treatment during an ulcerative process (7-10 days) requires consultation with an oncologist or maxillofacial surgeon, accompanied by a cytological or histological (biopsy) examination of the affected tissue. If signs of a tumor malignant process are detected, surgical treatment methods are used.
- A diagnosis confirmed by laboratory tests and excluding oncological or contagious diseases serves as the basis for prescribing conservative treatment, taking into account the etiology and associated factors.
General examination scheme
The first stage of interaction between a doctor and a patient is the collection of factual material, that is, the identification of symptoms of deviation from the norm. Next comes the clarification of the information received until the final diagnosis is made.
Research methods used in dentistry can be divided into the following groups: interviewing the patient (his relatives), examination, palpation, instrumental examination (probing, percussion of teeth, thermal diagnostics), assessment of gum and plaque condition indices, physical methods (electrical, radiological), laboratory studies (biochemical, bacteriological, cytological), special tests (blister test, histamine test, Kovetsky test, capillary resistance test), blood, urine, saliva tests.
Experts from the World Health Organization (WHO) recommend the following approach. The survey includes three parts: A
) extraoral region of the head and neck;
B
) perioral and intraoral soft tissues;
C
) teeth and periodontal tissues.
Settings, equipment and materials required (for all stages): adequate lighting, two dental mirrors and two gauze pads. We should not forget about gloves, a mask, and hygiene control.
The patient is in a sitting position.
First part of the examination - A
— requires a limited number of tools and takes no more than 5 minutes. The head, face, and neck are examined. The doctor evaluates changes in the size, color and shape of the parts of a given anatomical region.
When examining the skin, attention is paid to the presence of congenital changes (nevi, hemangiomas), as well as elements of damage in diseases. Notes the color, turgor, elasticity, moisture of the skin.
Some pathological changes, for example contractures, atrophy of facial muscles, are noticeable even during an external examination and must be recorded in the outpatient card (from a legal point of view, this is important in order to avoid a conflict situation when the patient is dissatisfied with the medical treatment provided).
It is necessary to pay attention to the shape and size of the pupils, which may reflect organic damage to the nervous system. Movement of the eyeballs is assessed, especially the presence of nystagmus (eye twitching). External examination of the facial muscles is insufficient. It is advisable to ask the patient to wrinkle his forehead, nose, open his mouth wide, and show his teeth. With facial nerve paralysis, tic-like twitching of the affected facial muscles, changes in the width of the palpebral fissure, and increased mechanical excitability of the muscles are observed. Peripheral paralysis of the lingual muscles causes fibrillary twitching with atrophy of the tongue (which may be a symptom of syringobulbia or amyotrophic lateral sclerosis). Bilateral paresis of the tongue causes a speech disorder such as dysarthria. Articulation defects and scanned speech are identified during conversation and questioning of the patient.
Part Two - B
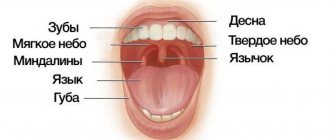
- includes 7 steps: red lip border; mucous membrane and transitional fold of the lips; corners of the mouth, mucous membrane and transitional fold of the cheeks; gums and alveolar margin; language; floor of the mouth; hard and soft palate.
B1 - lips are examined with the mouth open and closed. The color, shine, and consistency of the red border are recorded.
B2 - examine the mucous membrane of the lips and transitional fold (color, consistency, moisture, etc.). Normally, small elevations are sometimes found on the inner surface of the lip due to small mucous glands, which is not a pathology.
B3 - using two mirrors, first examine the right, then the left cheek (mucous) from the corner of the mouth to the palatine tonsil (pigmentation, color change, etc.). Along the line where the teeth meet, there may be derivatives of the sebaceous glands, which should not be mistaken for a pathology. These pale yellow nodules with a diameter of 1-2 mm do not rise above the mucous membrane. It must be remembered that at the level of the 17th and 27th teeth there are papillae on which the excretory duct of the parotid gland opens, sometimes also mistaken for deviations.
B4 - gums: first examine the buccal and labial areas, starting from the right upper posterior area, then move along the arc to the left. They descend onto the lower jaw from the left back and move to the right along an arc. Then the lingual and palatal areas of the gums are examined: from right to left on the upper jaw and from left to right along the lower jaw. Discoloration, swelling and swelling of various shapes and consistencies may occur on the gums. Along the transitional fold there are fistulous tracts, which most often arise as a result of a chronic inflammatory process in the apical periodontium.
B5 - tongue: consistency, mobility, all types of papillae are assessed. The shape, size, color of the tongue, the nature of the location and development of the papillae are determined. A healthy tongue has a soft pink color, its back is velvety, clean, in the morning it is somewhat whitish due to keratinization of the filiform papillae. Deviations from the norm should be considered changes in the size of the tongue, the presence of plaque, areas of increased desquamation of the epithelium, swelling, erosion, excoriation, ulcers, changes in relief, various anomalies of shape, attachment of the frenulum, etc.
B6 - floor of the mouth: changes in color, vascular pattern, etc. are recorded.
B7 - palate: examined with the mouth wide open and the head tilted back; Use a wide spatula to carefully press the root of the tongue, and use a dental mirror to examine the hard and then the soft palate.
When characterizing lesions of the mucous membrane, they clarify the boundaries of the pathological focus (clear, fuzzy), the relationship of its edges with the surrounding tissues (at the same level, roller-shaped edges), color (white, gray, pink, yellowish, cyanotic), the nature of the surface of the lesion (moist, shiny , dull), surface relief (smooth, lumpy, covered with small papillary processes), vascular pattern (number, shape and diameter of capillaries, uniformity of vessels, their color, presence or absence of deformation, flask-shaped swelling, intermittency).
Third part - C
- includes examination of the dentition and periodontium.
C1 - first, all teeth are examined. Otherwise, the true cause may remain undetected if the pain radiates to a healthy tooth or there is a phenomenon of repercussion, complications or a combination of diseases. In addition, examination of the dentition during the first visit allows you to outline a general treatment plan, that is, sanitation, which is the main task of the dentist.
It is recommended to carry out the examination in the same order, according to a certain system, using a dental mirror and probe. The mirror allows you to examine poorly accessible areas and direct a beam of light to the desired area, and the probe allows you to check all fissures, depressions, pigmented areas, and defects. If the integrity of the enamel is not broken, then the probe glides freely over the surface of the tooth without getting caught in the grooves and folds of the enamel. If there is a carious cavity in the tooth, sometimes invisible to the eye, the probe gets stuck in it.
The occlusal and proximal surfaces are carefully examined and probed, on which it is quite difficult to detect a cavity, especially a small one.
The examination of the dentition ends with the registration of the dental formula in the outpatient card and the calculation of the CP with an analysis of its structure.
C2 - during periodontal examination, in addition to determining the condition of the gums ( see
. stage B4), describes the state of the dentogingival attachment.
Optimal determination of periodontal parameters is ensured by the study of special indices.
Pathomorphology
Depending on the type of tumor growth, papillary and warty, as well as ulcerative and ulcerative-infiltrative forms of lip cancer are distinguished.
In 95% of cases it is squamous cell keratinizing cancer, in 5% it is squamous cell non-keratinizing cancer, characterized by a more malignant course (infiltrative growth and early metastasis to regional lymph nodes).
Depending on the prevalence of the tumor process, the stage of cancer is determined - from 0 to IV, which is taken into account when developing a treatment plan and assessing the prognosis (outcome) of the disease.
Diagnosis of lip cancer
In 2000 in Russia, 16% of patients with lip cancer were diagnosed in stages III-IV.
Reasons for delayed diagnosis: lack of oncological alertness among doctors of the general medical network, insufficient sanitary and educational work in a number of regions with a low culture of the population and, in connection with this, late access to a doctor.
If there are pathological changes on the red border, a mandatory set of diagnostic measures should include:
- study of complaints and history of the disease (duration of changes, dynamics, effectiveness of treatment);
- examination and palpation (palpation) of the lesion and regional (nearby) lymph nodes;
- taking fingerprint smears or scrapings from the surface of ulcerations, cracks, and punctate lip seals without signs of ulceration for microscopic examination. If necessary, a biopsy (taking a piece of tissue) should be performed to clarify the diagnosis.
- ultrasound examination (ultrasound) of the lymph nodes of the neck;
- differential diagnosis with tuberculosis and syphilis.
When the diagnosis of lip cancer is confirmed, an X-ray examination of the chest organs, general clinical and laboratory examination (ECG, blood tests, urine tests, etc.) are performed.
Precancerous skin diseases
Despite the fact that the malignant process of the skin is visually accessible, however, the stages and variability of its development, as well as the wide variety of benign dermatological pathologies, often do not allow timely recognition of a cancerous tumor.
In connection with the above, the problem of early diagnosis and treatment of a “pre-morbid” disease or pathological condition, that is, precancer, against which the development of a malignant neoplasm is more or less likely, has become of great relevance in dermatology and oncology.
Precancerous skin diseases are multiple or single papules, nodules, growths, spots, foci of hyperkeratosis or irritation of various shapes, colors and sizes, etc. They are benign epithelial formations and pathological conditions of non-tumor origin, but which can transform into malignant tumors.
The cause of malignancy can be:
- various external factors of a nonspecific nature - frequent or constant mechanical irritations or injuries, prolonged contact with chemicals (aniline dyes, petroleum derivatives, coal, arsenic, pesticides), exposure to temperature factors (frostbite and burns), excessive solar radiation, ionizing radiation, weathering;
- endogenous factors (in the body itself) - endocrine disorders, dysfunction of the immune system and some others;
- lack of timely treatment of benign pathology;
- age - among middle-aged and elderly people, transformation into cancer occurs much more often.
Diagnosis and treatment of precancerous skin pathologies are carried out by dermatological or oncological specialists.
Classification and diagnosis
A generally accepted classification of precancerous pathologies of the skin has not yet been developed due to the lack of sufficiently clear theoretical ideas about these pathological conditions. Therefore, the main ones are very conditionally divided into 2 groups:
- Obligate.
- Optional.
Obligate precancerous skin diseases
Obligate pathological conditions are characterized by a high probability of transformation into a malignant formation. These include:
- xeroderma pigmentosum;
- limited precancerous hyperkeratosis of the skin of the red border of the lips;
- Bowen's disease;
- Keir's erythroplasia;
- Paget's disease.
The last three pathologies are currently considered as a special form of skin cancer ( cancer in situ ), which is a local pre-invasive (intraepithelial) malignant process that does not extend beyond the skin. However, traditionally they are still classified as precancerous pathological conditions.
Xeroderma pigmentosum
It is a genetically determined, staged disease characterized by excessive sensitivity to even minor solar radiation. The first symptoms of this pathology with damage to the skin of the face and hands appear already in the first 3 years of a child’s life.
After a short exposure to the sun, limited erythematous spots and small pigmented yellowish-brown spots that resemble freckles appear on exposed areas of the skin. Their number gradually increases, the skin in these places becomes dry and flaky.
Subsequently, atrophic changes develop in their place, areas with telangiectasia and a smooth shiny surface appear. Even later, against this background, ulcerations and cracks appear, growths of a papillomatous and warty nature, transforming into a basal cell or squamous cell form of cancer, melanoma or sarcoma.
Malignancy occurs in 100% of cases. Malignant tumors have a high tendency to disintegrate and metastasize. Most patients die before the age of 15–20 years due to the generalization of the tumor process. However, although the gene for this pathology occurs in approximately 0.28% of people, it is inherited in an autosomal recessive manner, and therefore the disease develops in only one in 250 thousand cases.
Treatment of xeroderma pigmentosum is carried out after histological examination. For single growths, it involves electrical excision, laser or cryodestruction; for multiple growths, it involves a course of close-focus radiotherapy.
Limited precancerous hyperkeratosis of the skin of the red border of the lips
Unlike other obligate precancerous diseases, it often affects young and middle-aged people. Of all precancerous lip pathologies, 80% are due to this form of the disease. The lesion is polygonal in shape and sizes from 2 mm to 1.5 cm and is localized mainly on the lower lip directly on the red border.
It is surrounded by a whitish thin ridge, located approximately midway between the corner of the mouth and the center of the lip, soft and painful on palpation. The level of its surface in most patients is slightly lower than the level of the surrounding red border of the lip, which is why the lesion appears sunken. The surface is covered with grayish-brownish, densely spaced scales.
Usually the formation exists for several years in a benign state, but sometimes it transforms into a malignant tumor within the first year and even the first months from the moment of its appearance. The main symptoms that partially help in diagnosing malignancy are:
- the appearance of a compaction at its base;
- the appearance of erosion on its surface;
- strengthening of keratinization processes.
Treatment consists of electroexcision, laser destruction or surgical excision within healthy tissue, followed by histological examination. The decision on further treatment depends on the results of the latter.
Bowen's disease
Occurs with equal frequency among men and women over 40 years of age. Factors that provoke the development of a precancerous condition are ultraviolet rays and some toxic substances (arsenic, tar, tar). Any areas of the skin can be affected, but most often - closed areas (torso, genitals), less often - the face and neck.
Depending on the clinical manifestations, 4 forms of the disease are distinguished:
- papular-squamous;
- papular-cortical;
- atrophic;
- getting wet.
As a rule, the disease manifests itself as single or multiple plaques ranging in size from 1 mm to 10 cm. They tend to grow peripherally and have oval or irregular outlines, slightly rising above the surface of the skin, clear or blurred boundaries, yellow-red, and subsequently yellow-brown coloring Characteristically, there is an atrophic area of tissue or a scar in the central part of the plaque.
Sometimes the elements are covered with uneven crusts or scales, which resemble psoriatic elements. When these crusts or scales are removed, growths in the form of papillae with a smooth or warty surface may be exposed. When palpating the papules, the density of paper or cardboard is determined.
The course of Bowen's disease is long (years). Against this background, papillary (a type of squamous cell) cancer develops.
Erythroplasia Keira
It is a variant of the previous pathology and occurs only in 40–70-year-old men in the area of the glans penis or, less commonly, on the foreskin. In older men, the pathology is characterized by a more malignant course.
The disease manifests itself as single or multiple plaques with pronounced boundaries. The elements have raised edges and regular outlines, a smooth velvety surface of a reddish or bright red color. In case of infection, purulent or crumbly white deposits are possible.
Treatment of Bowen's disease and Keir's erythroplasia consists of electrical excision or cryodestruction of single lesions that are small in size. In other cases, the use of close-focus radiotherapy is recommended.
Paget's disease
It is a focus of erythema, accompanied by local pain, itching, tingling, burning. On its pinkish and slightly pigmented surface, reminiscent of eczema in appearance, epithelial scales, ulcerations and erosions appear.
The lesion has clearly defined boundaries and has a tendency to gradually slowly (over several years) expand and spread to neighboring tissues. Localization - mainly in the area around the nipple, but in 20% - in the face, head, back, thighs and buttocks, perineum and external genitalia, on the skin of the armpits.
The disease occurs after 50-60 years, mainly in women, but in men the course is more aggressive. Despite the slow development, there is always a transformation of precancerous pathology into an invasive malignant tumor. Treatment consists of radical resection of the mammary gland or complete mastectomy in combination with hormonal therapy, chemotherapy and radiotherapy. The extent of treatment depends on the extent of the lesion and is carried out after histological examination.
Optional precancerous skin diseases
Diseases in this group are united by a relatively low probability of degeneration into cancer. These mainly include:
- actinic, or solar, senile (senile) keratosis;
- cutaneous horn;
- keratoacanthoma;
Actinic keratosis
It develops, as a rule, in adulthood and old age in people with fair skin in open areas that are exposed to long-term (at least 10-20 years) sun exposure. The basis of the disease is dysplastic processes in the epithelium, as a result of which it can degenerate into squamous cell carcinoma.
Typically, senile keratosis is localized on sun-damaged skin (with uneven pigmentation, thinning) in the area of the back of the nose, cheeks, ears, scalp, lower lip and hands. Depending on the severity of clinical symptoms, stages or types of lesions are distinguished:
- Erythematous, which is the beginning of the disease and is characterized by the appearance of reddish-pink plaques and spots with sharply defined boundaries. The diameter of the elements initially does not exceed a few millimeters, and then gradually increases to 1-2 cm. Spots and plaques may have an irregular, oval or round shape and a lumpy, rough surface, against which telangiectasia occurs and bleeding occurs after slight scraping.
- The keratotypic stage of the precancerous condition represents the further development of lesions. They acquire a yellowish-brown or grayish-black color due to dense, easily detachable fatty layers of horny epithelium in the form of crusts. The lesions are surrounded by a narrow inflammatory border.
- Severe hyperkeratosis - elements protrude significantly above the surrounding skin surface and can transform into a cutaneous horn.
The development of senile keratosis is slow (over several years), after which malignancy in the form of squamous cell carcinoma is possible (20-25%). With malignant degeneration, itching, increased inflammatory symptoms, compaction of the base and increase in the thickness of the lesion, and the formation of an erosive, easily bleeding surface occur.
Single large lesions are removed surgically, by electroexcision, cryodestruction or laser therapy. Treatment of multiple lesions is carried out through applications of fluorouracil ointment, tretinoin, and imiquimod cream.
Cutaneous horn
It is an epithelial tumor with pronounced hyperkeratosis and is currently considered as a variant of senile keratosis. The formation can develop both against the background of scars, lupus erythematosus, lichen planus and other keratoses, and on externally unchanged skin.
The cutaneous horn is localized mainly on the head, face, and also on areas of the body that are subject to constant or frequent friction or pressure. In rare cases, it can occur in the red border of the lips.
Clinically, the cutaneous horn is a cylindrical, cone-shaped or branched formation, consisting of a dense accumulation of masses of horny epithelium of a whitish, dirty-grayish, brownish-gray or yellowish-brown color. It is firmly fused to its base, grows quite slowly, reaching sizes generally 0.5-1 cm, but often 4-5 cm.
Malignancy does not depend on the duration of the disease and is possible in 12-15% of cases. Its onset is accompanied by the appearance of pain, hardening of the base, inflammation around the tumor and sometimes a sharp acceleration of keratinization.
Treatment is only surgical. The formation is removed along with nearby healthy tissue.
Keratoacanthoma
It is, as a rule, a single, less often multiple, epidermal tumor, occurring in older people (usually 60–65 years of age). It is characterized by rapid growth, cyclical course and spontaneous regression. Malignancy occurs quite rarely (in 7%).
The development of keratoacanthoma is provoked by prolonged and intense solar radiation, inflammatory forms of dermatoses (seborrheic dermatitis, eczema), exposure to chemicals, and chronic trauma to the skin. The disease begins with the appearance of a small papule, which increases in diameter to 1.5-2 cm within 3-4 weeks.
The morphological basis of a precancerous tumor is the so-called “horny cup”. The formed formation has a grayish-pink color, dense consistency and hemispherical shape. It rises above the surrounding surface and is not fused to the underlying tissue (it is movable when attempting to move). In the “sinking” central part of the formation there are grayish dense horny masses, surrounded by a zone that rises in the form of a roller. Around the “horny cup” the skin texture is smoothed.
In the absence of independent reverse development of a solitary keratoacanthoma, treatment with cryodestruction, laser destruction or surgical excision is necessary, and in rare cases, with the use of radiation therapy. In case of multiple formations, oral methotrexate is prescribed.
Although the primary diagnosis of precancerous skin diseases is based on the clinical picture described above, histological examination plays the main role. In practical terms, the meaning of the concept of “cutaneous precancerous pathology” is that it makes it possible to identify groups with an increased risk of developing cancer from a significant number of people with dermatological pathology and carry out systematic monitoring of these patients with more in-depth studies. In medicine, the current strategy for combating malignant pathology is based on early detection and treatment of various forms of precancerous pathology.
Prognostic factors
Prognosis (outcome) factors for lip cancer are:
- prevalence of the process (size of the primary tumor, presence of metastases);
- clinical and anatomical form of cancer growth (exophytic forms proceed more favorably);
- morphological type of cancer (the non-keratinizing type is more aggressive);
- nature of tumor growth (primary or recurrent);
- age (patients under 40 years of age have a more malignant course).
The prognosis for lip cancer is generally favorable.
A worsening prognosis is associated with locally widespread infiltrative growth and significant regional and distant metastasis.
Clinical picture
Symptoms of lip cancer are varied and are determined by previous precancerous diseases and the morphological type of tumor.
In the early stages, a small roller-like rim appears around the edges around the compaction or erosion, which indicates a malignant process.
Papilloma, cutaneous horn, focus of verrucous leukoplakia, warty or nodular precancer develop into exophytic forms of cancer. The process lasts a long time, the infiltration of the underlying tissues increases gradually.
Destructive forms of dyskeratosis, Mangannotti cheilitis, and other ulcerative processes develop into endophytic forms of cancer - ulcerative and ulcerative-infiltrative.
In later stages, the boundaries between the clinical and anatomical forms of cancer are blurred. If untreated, the bottom of the ulcer reaches the muscle layer, tumor infiltration spreads to the entire lip, chin tissue, floor of the mouth, cheeks, and lower jaw.
Tissue breakdown intensifies, secondary infection occurs, nutrition is disrupted, and exhaustion develops.
Lip cancer is characterized by lymphogenous metastasis.
Metastases can develop on both sides (25%). Metastasis of cancer of the lower lip at stage I is observed in 2-6% of cases, at stage II - in 15-20%, at stage III - in 35% and at stage IV - in 70% of cases.
Distant metastases of lower lip cancer are rare (2%), mainly to the lungs.
Cancer of the upper lip, as a rule, is more malignant due to the characteristics of lymph circulation and metastasis.
Lip cancer treatment
The choice of treatment method depends mainly on the extent of the process (stage) and the type of tumor growth.
It is necessary to take into account the patient's age and the presence of concomitant pathology. Treatment consists of influencing the primary focus and areas of regional metastasis.
In stages I-II, cure for lip cancer can be achieved by several methods:
The cryogenic method is the effect of liquid nitrogen with a boiling point of -196 degrees C on the tumor. This method is the most effective with 100% cure, functionally sparing, because indicated for elderly people and those suffering from severe concomitant pathologies; it can be used once on an outpatient basis.
Radiation method – close-focus X-ray therapy (50-65 Gy), interstitial radiation therapy (50-70 Gy), electron therapy (SOD 50-70 Gy).
The surgical method is used when it is impossible to use cryogenic or radiation treatment.
Photodynamic therapy is laser exposure against the background of local or intravenous administration of a photosensitizing drug for limited superficial lesions.
Preventive surgery on the neck in stages I-II is indicated only if there is no possibility of dynamic observation by an oncologist in patients with unfavorable prognosis factors (young men, non-keratinizing type of squamous cell carcinoma, infiltrative growth form).
In stage III without metastases in regional lymph nodes, treatment can be carried out:
Cryogenic method , using cryoapplication, cryo-irrigation or a combination thereof. Preventive surgery on the neck is performed for the same indications as stages I-II.
Neck surgery can be performed simultaneously with cryogenic exposure.
Radiation method (combined radiation treatment at 60-70 Gy). The zone of radiation exposure includes areas of regional metastasis.
Combined method (preoperative gamma therapy with a dose of 40-50 Gy on the primary tumor and areas of regional metastasis, followed by surgery.
For locally advanced lip cancer without metastases or with single metastases in regional lymph nodes (stage IV), combined treatment followed by extended surgery and primary or delayed plastic surgery is possible.
Chemotherapy is carried out with platinum drugs , fluorouracil , methotrexate , bleomycin .
For limited recurrences of lip cancer, surgical or cryogenic treatment is indicated.
In case of widespread relapses, it is possible to perform extended surgical interventions with simultaneous plastic surgery.
Diagnostics
Methods for examining patients with precancerous conditions
Due to the absence of subjective sensations in the initial stages of precancerous conditions, a thorough examination of the oral mucosa should be carried out in all patients who consult a dentist.
Diagnosis of diseases of this group requires the dentist to have knowledge of dermatology, pathology of internal organs and systems, neurology, psychiatry, etc. In difficult cases, you should seek advice from specialists in the relevant field.
Patients with precancerous conditions require special examination. It should be carried out as planned and in a certain sequence, which will allow the doctor to study the picture of the disease in detail without missing a single symptom. The examination begins with a survey. It is important to exclude cancerophobia. As a rule, patients with precancers have no special complaints. Complaints may include a feeling of roughness in some area of the mucous membrane, bulging, sensation of a foreign body, burning or pain when eating hot or spicy food. Many patients have no complaints at all. Particular attention is paid to hereditary history, the presence of bad habits, occupational hazards, past and concomitant diseases.
After clarification of complaints, they proceed to inspection. It must be carried out in natural light, because... artificial changes the color of the mucous membrane and can contribute to diagnostic errors. The patient should be placed in a comfortable position for examination in a chair. The examination begins with the skin of the face, because... many mucosal diseases are combined with skin lesions. On the mucous membrane of the cheeks and lips one can notice reduced sebaceous glands, usually located in groups in the form of yellowish nodules. Using a spatula or mirror, the vestibule of the oral cavity is examined. The function of the parotid salivary glands, the excretory ducts of which open at the level of the second upper molars, is studied. Then the oral cavity is examined. The function of the submandibular salivary glands, tongue, and pharynx are examined.
A very important element in examining a patient is palpation . Cheeks, lips, tongue are palpated with two fingers; thumb and index finger or bimanually. In this case, the consistency, mobility, and soreness of organs and tissues are determined; Regional lymph nodes (all groups!) are subject to mandatory palpation.
Dentistry is the most acceptable diagnostic method in dental practice. If necessary, it can be used to select the site for biopsy. In 1959, Schönemann reported the first applications of the Ginzelmann colposcope for stomatoscopy. Currently, a photodiagnoscope is used for this purpose, which allows simultaneous photographing of areas of interest to the mucous membrane.
Dentistry (simple) is carried out as follows. The patient sits on a chair, places his chin on a special stand at a distance of 30-40 cm from the device. Focus and begin the study, starting with the red border of the lips and further, following the sequence as described above. Extended stomatoscopy is used to obtain greater clarity of the mucosal pattern. To do this, one or another vital staining method is first used (4% acetic acid, 2% Lugol’s solution, 1% toluidine blue solution, hematoxylin according to A.B. Derazhnya).
Acetic acid test: apply a cotton swab soaked in 2-4% acetic acid for 20-30 seconds. Acid helps quickly eliminate mucus that interferes with examination. Swelling of the epithelium occurs, as a result of which the vessels disappear from view and do not interfere with studying the surface of the mucous membrane. The action of acetic acid lasts for 1-1.5 minutes. This test is most indicative of the buccal mucosa.
Iodine reaction ( Schiller test ) - use a 2% aqueous Lugol solution. The technique consists of applying an application of a cotton swab moistened with Lugol's solution for 1 minute on the area under study, covering 1 - 2 cm of visually normal mucous membrane. Then the result is examined using a stomatoscope. It should be borne in mind that with this test the mucous membrane is colored differently.
In mobile areas (lips, cheeks, transitional folds, sublingual area), a dark brown color is observed, and the red border of the lips, gums, mucous membrane of the hard palate, and the back of the tongue are iodine-negative, since they are covered with epithelium that has a small layer of keratinization. The essence of this test is as follows: the active protective functions of regeneration and keratinization are accompanied by high energy metabolism in the epithelium.
The synthesis and accumulation of large amounts of glycogen are characteristic of stratified squamous epithelial cells. Most of all, it accumulates in those parts of the mucous membrane where the epithelium is not normally subject to keratinization (mobile areas of the mucosa). In the keratinizing epithelium (stationary areas), glycogen is normally completely absent or there are traces of it.
It is believed that glycogen plays the role of an energy source or plastic material for the synthesis of keratin protein. In the non-keratinizing epithelium there are no cells with keratin, but it contains many lumps and grains of glycogen. In those areas of the mucosa where the epithelium undergoes keratinization, glycogen is quickly consumed for the synthesis of protein - keratin and therefore is not detected during histochemical examination. With the development of inflammation in the tissue, the processes of keratinization sharply weaken or stop completely, and the amount of glycogen increases greatly. This can be used for differential diagnosis.
There are 3 degrees of iodine negativity:
- 1st degree - complete absence of staining,
- 2nd degree - iodine negativity in pathological conditions of the mucous membrane, accompanied by parakeratosis of the epithelium,
- 3rd degree - iodine negativity is detected in areas of supposed (visually) normal mucous membrane and in the surrounding area of the lesion.
Prevention of lip cancer
- Preventive examinations of the population, clinical examination of persons constituting a high-risk group, sanitary and educational work.
- Carrying out hygienic measures, sanitation of the oral cavity, adequate prosthetics.
- Treatment of underlying diseases, precancerous changes in the mucous membrane: the use of indifferent ointments and hygienic lip protection products in persons whose profession is associated with harmful effects on the lips and are exposed to prolonged adverse meteorological factors;
- giving up bad habits (smoking, eating chewing mixtures that irritate the mucous membrane of the lips) and eliminating harmful environmental factors;
- normalization of gastrointestinal tract function, increased immunity.
Prevention
Sanitation of the oral cavity, prevention of injuries to the red border of the lips during work and at home, avoidance of burns from smoking, protection from adverse weather conditions, excessive insolation. Persons with dry skin should use moisturizing creams.
It is useful to take vitamin A concentrate 5-7 drops orally 3 times a day for 2 months, repeating 2-3 courses per year. Long-term intake of B vitamins is also recommended. Smoking and drinking alcoholic beverages are avoided. It is necessary to treat actinic and hayandular cheilitis, eliminate the consequences of vesicular lichen and prevent its relapses. Prevention of chronic trauma to the oral mucosa with teeth, dentures, fillings, exclusion of chemical, thermal, bacteriological damage to it. Salt-free, alcohol-free diet. Avoid spicy foods.