While expecting a child, the body of the expectant mother undergoes various changes associated with the restructuring of all organs and systems. Which must now ensure the vital functions of both the female body and the development of the unborn child. For this reason, a woman’s metabolism may change, a lack of microelements and vitamins in the body may be detected, etc. Very often this is reflected in the condition of the teeth, since a growing fetus requires a lot of calcium for its formation. Therefore, doctors strongly recommend taking care of your teeth during pregnancy to prevent their damage and loss in the future.
The more attention a wisdom tooth requires during pregnancy. Since “eights”, due to their characteristics, can cause a lot of inconvenience to any person, and when carrying a child this can become especially problematic.
Content:
- Pregnancy and wisdom teeth - how to recognize the process of active growth
- Pericoronitis - complication 2.1. Classification of pathology
- What can an expectant mother do on her own?
- Removal
- What you should never do
- Competent treatment
- Rehabilitation after surgery
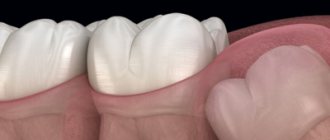
It happens that wisdom teeth begin to actively grow during pregnancy .
This is due to the fact that “eights” are cut later than other units. The process of their active growth can be triggered by hormonal and metabolic changes that occur in a woman’s body during pregnancy. The process of the appearance of eighth units in itself cannot be called negative - it is a variant of the norm. But for many expectant mothers it occurs with complications. It was also not uncommon for units to stand at the wrong angle and put extreme pressure on their “neighbors.” And this is an indication for emergency removal.
When is the best time for pregnant women to have their teeth treated?
If a woman took a responsible approach to pregnancy and had her teeth treated in advance, she still needs to visit the dentist regularly for preventive examinations. This will allow you to detect pathology at an early stage and use the safest treatment methods. When performing any dental procedure, not only the woman’s well-being matters, but also the duration of pregnancy. Each trimester has its own characteristics and risks that determine the choice of treatment method.
First trimester
1st trimester
– period
from 1 to 12 weeks
inclusive. At this time, the formation of organs and structures of the embryo occurs. The placenta does not yet protect the fetus well enough from external influences, and the woman’s body undergoes serious changes: hormonal, physiological, metabolic. Any interventions, including medications, can negatively affect the pregnancy process and the health of the baby.
If a pregnant woman has a toothache in the 1st trimester, treatment is carried out mainly using gentle methods
(ICON, ozone therapy, air abrasive method). For pulpitis, periodontitis, accompanied by acute pain and purulent discharge, local anesthesia based on articaine (Ultracaine, Melivastesin, Mepifrine, Skadonest) is used.
Second trimester
2nd trimester
– period
from 13 to 24 weeks
.
This is the safest time
for dental treatment, gum treatment, professional hygiene and other dental interventions. The tissues, organs, and systems of the fetus have already been formed; the placenta reliably protects the baby from external factors. All planned procedures are recommended to be performed during this period.
Third trimester
3rd trimester
– the period
from 25 weeks to childbirth
, quite difficult for a pregnant woman.
The stress on the body increases, the placenta becomes more susceptible to external factors. Treatment is carried out exclusively for acute conditions
that are dangerous for the mother and child. Planned procedures are postponed until the baby is born.
If there is a need for dental treatment in a pregnant woman, a new generation of anesthetics based on articaine is used. The components of these drugs do not penetrate the placental barrier, do not affect the uterine and placental blood flow, do not increase the tone of the uterus, and are safe for the expectant mother and child. An alternative to local anesthesia is treatment under sedation (during sleep).
Pregnancy and wisdom teeth - how to recognize the process of active growth
The symptoms that occur in pregnant women when the bone tissue above the figure eight “gives way” often differ from the classic picture. First, the woman notes that she began to get tired faster. Her performance decreases and her body temperature rises. In this case, the condition of the gums in the first days of symptoms may not change in any way.
Only after a few days (and sometimes weeks) it becomes clear that all the ailments are associated with teething. Signs characteristic of the situation are:
- pain when feeling the inflamed gum;
- acquisition of a red-blue hue by the mucous membranes located in the eruption zone;
- involuntary cheek twitching;
- enlarged and painful lymph nodes;
- the appearance of bad breath (it is not possible to get rid of it using standard hygiene products);
- hoarseness of voice;
- discomfort or throbbing pain in the ear on the causative side;
- painful sensations when chewing food, swallowing saliva, liquids.
If the first symptoms of the eruption of “eights” appear, it is important for the pregnant woman to calm down and not panic. It is quite possible that the emergence of new units will not be associated with any problems. But if the pain becomes severe, you should definitely get a dental consultation.
Is it possible to do x-rays?
Contrary to popular belief, X-rays can be taken during pregnancy. For this purpose, computer radiovisiographs are used. The radiation dose received by the patient when using a visiograph is minimal. If possible, the study should be carried out in the 2nd trimester
, excluding cases where urgent help is required - severe, acute pain in the teeth during pregnancy. X-ray examination is carried out observing all possible means of protecting the fetus.
“Fighting” radiation on the visiograph, women calmly fly south to eat fruit and bask in the sun. Not knowing that during a 2-3 hour flight a person receives 20-30 μSv. This is a radiation dose equivalent to 10-15 images on a visiograph. Ionizing radiation differs from light rays only in wavelength and has a damaging effect only under certain conditions.
Pericoronitis - a complication
Pericoronitis (pericoronitis) is a condition in which the soft tissues surrounding an erupting tooth become severely inflamed. Very often, this diagnosis is made to patients who have begun to see “figure eights” in their mouths. It is characterized by symptoms:
- sore gums;
- swelling;
- specific taste in the mouth.
For pericoronitis, surgery is most often indicated. During this procedure, the doctor excises the “hood” covering the unit to facilitate its eruption. Also, with this complication, there is sometimes a need for removal.
Classification of pathology
Pericoronitis is classified into:
- serous;
- purulent.
The disease always develops from the serous form. This is its initial stage. A large amount of serous fluid accumulates in the mucous tissues. Pain occurs when palpating the affected area.
If a woman does not go to the dentist on time, the serous form turns into a more dangerous one - purulent. Then the swelling becomes even stronger, and the body temperature periodically rises. A “hood” begins to cover the bone tissue, under which there is a large amount of pus.
The purulent form is treated exclusively surgically . After opening the “fistula,” the tissues are washed and the patient is prescribed antibiotics. Considering that such manipulations are extremely undesirable during the period of bearing a child, it is important not to start the disease and consult a doctor at the first sign of it.
What can an expectant mother do on her own?
Pregnant women should not self-medicate. But, if the eruption of wisdom teeth proceeds according to the classic scenario and does not cause negative symptoms, the woman can calm down. In this case, she does not need to run to the dentist.
To eliminate the occurrence of unpleasant sensations associated with putting pressure on the inflamed gum, you must try to chew food on the “healthy side”. After eating, be sure to rinse your mouth with warm water or a decoction of herbs. It is also permissible to purchase a special pharmacy rinse for this purpose.
If the pain intensifies, medical consultation is indicated. If for some reason it is impossible to get it right now, the expectant mother can take a no-shpa tablet to reduce the pain. But this should be a one-time “action”.
How to relieve pain yourself
Rinsing with a soda solution (1 teaspoon of soda per glass of warm water) will help temporarily relieve toothache during pregnancy. You need to rinse your mouth more often, every 2 hours. In addition to soda, you can use Furacilin solution, decoctions of medicinal herbs - chamomile, oak bark, yarrow.
Not recommended
use herbs containing essential oils (sage, eucalyptus, peppermint, cloves, etc.), they can cause severe uterine cramps.
Severe dental pain during pregnancy can be treated with a suitable anesthetic. Steroid-based drugs and drugs that penetrate the placental barrier are contraindicated.
Removal
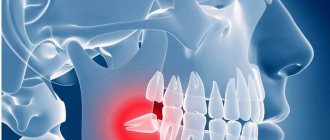
As practice shows, only in 5% of cases pregnant women have to pull out the “eight”. In other situations, it is possible to do without deletion. Extraction is permissible only if there are strict indications, including:
- inability to relieve severe pain using available painkillers;
- frequent recurrence of pericoronitis;
- the formation of an abscess affecting the facial nerve;
- destruction and suppuration of bone tissue;
- the formation of a hollow tumor on the bone in the figure eight area.
In all these cases, the woman is scheduled for dental surgery. Anesthesia is selected taking into account the duration of pregnancy and existing concomitant diseases. However, earlier than in the second trimester, extraction is contraindicated.
Is it possible for pregnant women to have dental x-rays?
Pregnancy is not considered a contraindication for dental radiography. Images are taken using computer radiovisiographs, which deliver a very small dose of radiation. The woman’s body is covered with a special protective apron, and the radiation beam is directed towards the jaw area.
However, such a procedure should be performed only when absolutely necessary and should be limited to taking pictures of one or two teeth. Long-term planned treatment, which periodically requires radiography, is best postponed until the birth of the child and completion of breastfeeding.
What you should never do
A pregnant woman is strictly prohibited from doing the following things, as they can lead to malformations of the fetus:
- Take analgesics without a doctor's prescription. All drugs of this pharmacological group have many side effects.
- Apply painkillers to the inflamed gum. Such advice is available on the Internet, but you cannot follow it. Such compresses increase inflammation and create conditions for the formation of ulcers. In addition, the active compounds of the medications used will be absorbed into the systemic bloodstream and negatively affect the health of the fetus.
- Warm the affected area. Heat increases local blood circulation and helps the purulent tumor grow faster.
Self-medication during pregnancy is unacceptable. This is important for all women in an “interesting” position to understand.
Prevention methods
- Every six months it is necessary to make an appointment at the dental clinic, especially before planning to conceive.
- Balance your diet to eliminate possible deficiencies of calcium and other microelements.
- Walk in the sun more, it helps to get vitamin D, which is necessary for the absorption of calcium.
- The advice is not very relevant for pregnant women, but: get rid of bad habits. Smoking causes tooth decay.
- Clean your mouth twice a day with a brush and paste, and after each meal with a mouthwash.
In the article, we told you at what week of pregnancy you can have teeth removed, how this will affect the fetus and the health of the expectant mother. And for quality dental services, make an appointment at Dentika.
Competent treatment
Doctors can offer pregnant women only three options for eliminating inflammation during the eruption of wisdom teeth:
- Excision of the hood. The operation is simple and is performed under local anesthesia. The doctor makes a small incision, which reduces the likelihood of an abscess forming and speeds up the process of the “figure eight” appearance.
- Excision of the upper tissues of the mucous membrane. It is carried out if the doctor sees an abnormal bone structure in the image. The altered structures are then removed to save the tooth.
- Ripping out. It is used rarely and only if previous methods have proven ineffective. If extraction is unavoidable, it should be postponed until the threat to the health of the fetus is minimal.
Is it necessary to remove a tooth?
Only a dentist can prescribe the correct treatment. Removal is recommended in difficult situations to prevent complications. If it is possible to do without surgery, it is not planned. When selecting a treatment method, the doctor takes into account the patient’s condition. Wisdom tooth removal is justified if:
- The process of growth causes unbearable pain;
- The inflammatory process in the gum tissue progresses;
- A cyst or granuloma has formed on the top of the tooth;
- Purulent exudate is released;
The operations are performed under anesthesia. Local anesthetics approved during pregnancy are used. Please note that the source of infection in the body is much more dangerous than anesthetic drugs. Therefore, it is necessary to cure or remove the figure eight in order to prevent serious complications in the fetus and the woman in labor.
It is better to operate within 13 – 32 weeks. It is contraindicated to carry out procedures later or earlier. Anesthetics used are those that do not penetrate into the placenta, in particular, ultracaine, primacaine. The correct dosage is extremely important. It is calculated depending on the age, general condition of the woman in labor, and the duration of pregnancy.
In addition to removal, dissection of the hood is practiced, when a minimal incision of the mucous membrane is made over the bone tissue. This prevents the accumulation of pus and speeds up the advancement of the unit. If the bone tissue structure is normal, excision may be recommended, when the upper section of the mucosa covering the site where the rudiment is cut is completely removed. This allows you to do without pulling out the figure eight.
Rehabilitation after surgery
If a woman was unable to avoid surgical treatment, she needs to pay maximum attention to the rehabilitation process. Recovery will be faster if the expectant mother:
- will follow all medical prescriptions;
- will provide complete rest to the damaged area (it should not be touched with hands, tongue, or foreign objects);
- will not eat solid foods;
- will carry out high-quality oral hygiene;
- He will come for a follow-up appointment when the dental surgeon says so.
Take care of the health of your smile. If you are planning to conceive, treat any existing oral diseases in advance. If the problem arose after conception, be sure to get dental care - do not risk your health and the health of your baby.
What to do after tooth extraction during pregnancy
Even if the procedure was successful, without pain, complications may develop during the recovery period. It is very important that after extirpation a blood clot is formed and firmly attached. It protects the resulting cavity with exposed bone and nerve endings from infection by bacteria and food.
The natural “plug” may come off in the following cases:
- sticking to a cotton swab (placed after surgery) if held for too long;
- licking the hole with the tongue;
- using a drinking straw;
- newly opened bleeding.
If the blood clot falls out, a new surgical intervention will be required. Otherwise, an inflammatory process will occur, which can lead to complications.
It is not recommended to get tired on the day of surgery. After the procedure, you need to go home and rest. You can eat after 3 - 4 hours. Food should be at a comfortable temperature, soft or liquid. Spicy, rough foods that injure soft tissues should be excluded. You should not smoke, as nicotine constricts blood vessels and interferes with healing.
You can rinse your mouth on the second day. As an antiseptic, pharmaceutical preparations, decoctions of medicinal plants, and an aqueous solution with salt and soda are used. Medicines will prevent the development of infection and speed up wound healing. Rinsing should be gentle and not intense, otherwise the blood clot will come off.
When brushing teeth, the surgical site is bypassed. You should use a toothbrush with soft bristles.
Until the wound heals, you should not overheat the body or exert physical stress. Otherwise, bleeding may resume.