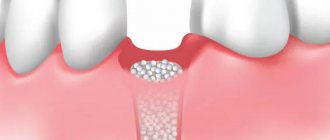
Osteoplasty in dentistry is the augmentation of bone tissue necessary for successful implantation. After a person has a tooth removed, the hard tissue tends to dissolve, and the new artificial tooth must be held securely in the jaw. Bone augmentation for dental implantation successfully solves this problem, but requires additional costs and more time (than, for example, with one-stage implantation, when the tissue volume is sufficient).
Webinars on using EthOss from world clinicians
REGISTRATION CERTIFICATE
Bone grafting is one of the most popular operations in maxillofacial surgery and dentistry. It is needed to prepare the patient for the installation of a dental implant. Due to various dental pathologies or prolonged absence of teeth, bones undergo atrophic processes and become thin. Since the bone must be sufficiently dense for the implant to be installed and survive well, bone grafting will help correct the bone deficiency.
Biological bone materials are usually created in two ways - either from the bone tissue of cattle, or from cadaveric biomaterials, that is, from the bones of deceased people. Yes, this is allowed in most countries, but you must admit that in the 21st century, using such a technique no longer seems like a completely modern way to restore a smile, and besides, there is a high risk of getting an allergic reaction, or the patient’s personal intolerance to these materials, as well as cross-infection of the bone.
Therefore, technology has not stood still for a long time, and British clinicians have found a way out of this situation and created a completely safe synthetic bone material that causes natural regeneration of human bones, consisting of calcium beta-triphosphate and calcium sulfate. This development is called - bone material EthOss (Ethos)
EthOss is a bone material developed by implantologists for implantologists. It consists of absolutely biocompatible materials that stimulate bone regeneration processes. Contains no animal or human ingredients.
The use of this material has achieved clinical success among a huge number of specialists, since EthOss eliminates the need for donor grafts and artificial scaffolds. The built-in barrier eliminates the need for additional membranes and speeds up the surgical process. This results in a faster operation with a minimally low pain threshold for the patient.
Pros and cons of bone grafting during implantation
Competitive advantages of bone grafting:
- restoration of functions, even if the patient has lost a large amount of hard tissue;
- the appearance of the gum tissue and the oral cavity as a whole is normalized;
- restoration of chewing functions - all types of bone tissue in dentistry are adapted to heavy loads;
- the ability to restore teeth, even in the most advanced situations.
Disadvantages of bone grafting:
- rehabilitation takes several months;
- high risk of block rejection;
- pain during tissue engraftment;
- considerable cost of the operation.
Who invented the bone material EthOss?
This composition of bone material was invented by two clinicians - Dr. Peter Fairbairn and Dr. Paul Harrison.
Dr. Peter Fairbairn, Professor at the University of Detroit School of Dentistry (Michigan, USA), Director of Education of the Association of Dental Implantology (UK), one of the Presidents of the London Dental Association, and Dr. Paul Harrison (member of PHD, MBA, BSC). He is also a global expert in dental product design.
Following an academic career at the University of Leeds, Dr Paul Harrison founded an independent advanced materials invention consultancy. One successful project involved the development of a bone stretching technique using external fixators to strengthen the union after a fracture. Thanks to this, Paul became interested in the subject of bone regeneration.
From the very beginning, EthOss was designed with dentists in mind. True bone regeneration is more than using bone materials to create volume and an artificial frame. The use of EthOss has been proven to promote faster growth of native bone with little pain. Since 2015, its popularity among dentists and patients has been growing very quickly, which was also facilitated by the British Online Academy. EthOss was conceived and developed by clinicians in the UK and is available worldwide.
What implants are used after bone grafting?
Are there “special implants” that are recommended in cases of bone grafting? Both with bone grafting and without bone grafting, it is necessary to use implants only from good, proven manufacturers, those that have a good clinical base. For example – Straumann, Nobel, Ankylos, Xive, Astra Tech.
There are a number of other implant systems that give good results. But at the German Implant Center we use only the best implant systems, only premium ones.
Examples of work “Before” and “After”
Restoration of chewing teeth of the lower jaw
Case: destruction of the chewing group of teeth of the lower jaw on the right under a bridge.
Basal implantology with instant loading
Case: The patient complained of an uncomfortable removable denture.
Restoration of all teeth on the upper and lower jaw - basal implantation
Case: partial absence of teeth on the upper and lower jaws, complicated by a severe form of periodontitis (tooth mobility).
Simultaneous implantation in the lateral sections of the upper and lower jaw
Case: tooth decay under crowns in the lateral sections of the upper and lower jaws.
Extranasal operations play a significant role in surgery of the paranasal sinuses [1, 2]. However, after extranasal operations on the paranasal sinuses, significant bone defects remain into which soft tissue grows. The result is stagnation of secretions in the sinus, proliferation of fibrous tissue and the development of scarring, which ultimately leads to a decrease in sinus volume and thickening of the bony walls of the sinus [3, 4]. The tendency to obliteration is most clearly manifested after Caldwell-Luc surgery in childhood [5]. In addition, retraction of the soft tissues of the face appears in the area of the defect [6], and neuralgic pain occurs due to compression of the branches of the trigeminal nerve by scar tissue [7].
Currently, most clinicians are of the opinion that it is necessary to close postoperative defects in the walls of the paranasal sinuses. However, despite the successes achieved in the use of drainage operations, in the practice of an otorhinolaryngologist such pathological conditions of the frontal-ethmoidal zone are observed when the preservation of the frontal sinus as an air cavity is not possible, and there is a need to obliterate the affected frontal sinuses [8-13].
For the purpose of obliteration, both auto- and allografts and adhesive osteoplastic compositions are used [14–19]. During surgery on the frontal sinus to obliterate it, all contents and all the mucous membrane are carefully removed from the sinus. Complete isolation of the sinus and graft from the external environment is achieved, and the contours of the frontal region are restored [20]. This technique has its drawbacks. The literature [19] describes cases of melting of the allograft with the formation of a cavity and purulent fistula of the frontal sinus, cases of the formation of a secondary pyomucocele and limited osteomyelitis of the anterior wall of the frontal sinus [19].
In search of another way to close defects in the walls of the sinuses, the most rational solution to the problem is plastic restoration of the walls of the paranasal sinuses using various materials. Today there is a huge amount of frame materials on the world market. Bone grafts are any implanted materials that, alone or in combination with other materials, promote bone formation by providing local osteoconductive, osteoinductive, or osteogenic activity.
Osteoconductive materials promote the attachment, proliferation and differentiation of poorly differentiated cells into osteoblasts with subsequent bone formation on their surface. Osteoconductive osteogenesis is considered to be “creeping replacement,” i.e., primary resorption of the implant with secondary subsequent ingrowth of supporting tissues from the maternal bed. In these cases, the implant plays the role of a scaffold for the germination of blood vessels. Then the ingrowth of cells from the maternal bed occurs. This mechanism combines the processes of resorption and the formation of new supporting tissue, starting from the borders of the defect. Osteoinductive materials contain biologically active substances that induce recipient bed cells to differentiate into osteoblasts [21]. Osteogenic materials (autografts and materials enriched with cultured autogenous bone cells) contain living host cells capable of differentiating into osteoblasts.
Any bone grafts must have the following properties: a) be completely biocompatible and bioinert; b) be porous; c) serve as a matrix on the surface of which recipient cells are fixed (osteoconductivity); d) gradually be resorbed and replaced by newly formed bone (creeping replacement); e) have a density and physical properties similar to the fabric where it is placed, as well as the ability to resist mechanical stress; f) be easily accessible, well preserved and sterilized; g) in preparation for transplantation, it is easy to process to obtain the desired shape; h) not to be rejected [22].
Currently, both synthetic and natural materials are used for plastics. Main types of bone implants:
1. Autograft - the donor is the patient himself.
These can be bone flaps, crushed or preserved autologous bone or cartilage. Since one's own bone or cartilage tissue is implanted, very good compatibility is ensured with the area in which the tissue is implanted, as well as with all other adjacent tissues. The essence of osteoplastic methods used in rhinology is to create various modifications of the osteoperiosteal plastic flap, which is “broken out” from the wall of the frontal or maxillary sinus before surgery and placed in its original place at the end of the operation [23-25]. Autocartilage of the nasal septum is also used to close defects in the anterior wall of the frontal sinus [26] and the upper wall of the maxillary sinus [27]. This method also has disadvantages. The collection of autologous bone or cartilage may be accompanied by complications: damage to blood vessels and nerves, the formation of hematomas, and the development of an infectious and inflammatory process. In addition, autografts are often resorbed faster than their integration and restoration of the bone defect occurs [28].
2. Allograft - the donor is another person.
We are talking about a bone graft taken from a donor. Allografts include fetal anlage or bone, fresh allogeneic bone, ground allogeneic bone, preserved bone, and demineralized bone matrix. The recipient's body is able to transform this type of bone tissue into its own tissue, and therefore, after implantation, the foreign bone tissue takes root in the body, turning into its own. Bone allografts are characterized by slow osseointegration; their use carries the risk of developing histoincompatibility reactions and chronic granulomatous inflammation [29].
Among biological materials, in recent decades, demineralized bone grafts, called “bone matrix” by some authors, have become widespread in otorhinolaryngology to cover various defects of bone structures. Prof. A.G. Volkov was one of the first in his specialty to use demineralized bone graft - DBT, which is a specially processed cadaveric bone, to restore extensive bone defects that arise after radical surgical treatment for tumors of the frontal sinuses. Demineralized bone matrix was used in plastic surgery of the external nose and nasal septum [22, 30], to restore the lower wall of the orbit destroyed during a fracture [31], and fractures of the walls of the frontal sinuses [32]. A similar bone plastic material with the commercial name “Perfoost” is a demineralized lyophilized perforated plate prepared from long and flat bones of allogeneic origin. The Perfoost allo-implant is successfully used in reconstructive plastic surgeries on the nasal septum that require compensation for defects in both the cartilaginous and bony parts of the nasal septum [21].
A number of authors [22] drew attention to the possibility of using fetal bone (brefomatrix). Due to its pronounced osteoinductive properties, embryonic matrix is successfully used in patients with various defects of the external nose and nasal septum.
3. Xenograft is an animal source. This is a bone or cartilage graft taken from the animal's body. When the graft is in the body, the process of its replacement with human tissue occurs, and it serves as a “framework” for the formation of a person’s own bone tissue. The disadvantage of xenografts is that they are resorbed and replaced by new bone tissue extremely slowly. In rhinology, preserved porcine costal cartilages were used for rhinoplasty, for obliteration of the frontal sinuses and plastic surgery of the fronto-orbital region after extranasal removal of osteoma of the ethmoidal labyrinth [33].
4. Synthetic source.
This implant is an inert, synthetic, artificial substance that is manufactured in laboratories. The use of artificial materials avoids preliminary implantation near the defect and does not limit the surgeon in the amount of material.
According to the literature, synthetic implantable materials include explants (metals, polymers, porous carbon compounds, ceramics). Depending on the manufacturing method and the type of material, bone substitutes are classified as “absorbable” or biodegradable and “non-absorbable”. In other words, our body may or may not replace synthetic material with its own bone tissue, depending on the type of material. If these implants have pores with a diameter greater than 100 µm, bone ingrowth may occur, which ensures its attachment to the material (biological anchorage).
The main disadvantage of synthetic materials, in contrast to auto-, allo- and some xenomaterials, is their lack of osteoinductive properties. The osteoinductive properties of bone replacement materials include their ability to stimulate bone tissue regeneration. For this purpose, composite materials were created. Composite materials are a combination of an osteoconductive matrix with bioactive agents that provide osteoinductive and/or osteogenic properties, which makes these materials equal in bioactive properties to auto-, allo-, and xenografts. This biological activity may be due to the inclusion of sulfated glycosaminoglycans, amino acids, growth factors and morphogens in the bone-replacing material [34].
A number of calcium phosphate materials, such as hydroxyapatite, tricalcium phosphate, some compositions of silicate glass and glass ceramics, are bioactive materials similar in composition to human bone tissue. The latter contribute to the formation of bone on their surface and the formation of strong chemical bonds with the latter (bioactive fixation). These bioactive materials are an osteoconductive matrix that causes adhesion of morphogenetic proteins, osteoblast precursor cells, their proliferation and differentiation into osteoblasts. Synthetic materials based on artificial hydroxyapatite are superior to hydroxyapatite of animal origin in a number of characteristics. They eliminate the possibility of transmitting infectious diseases and allow you to regulate the rate of resorption due to the peculiarities of synthesis and various substitutions of phosphate and hydroxyl groups in the structure of apatite. This characterizes synthetic hydroxyapatite as a promising osteoplastic material for use in all areas of osteoplastic surgery.
In the literature under study [25], there are works on the use of hydroxyapatite to close a defect in the upper wall of the maxillary sinus [35], postoperative defects in the walls of the paranasal sinuses after removal of osteomas. One of the disadvantages of calcium phosphate ceramics is the low mechanical strength of this type of implant.
Corundum ceramics, which is bioinert and biocompatible, and has a high degree of strength, turned out to be suitable for plastic surgery of the walls of the paranasal sinuses in terms of its physicochemical properties [36]. But, unfortunately, full modeling of corundum ceramic plates based on the shape of a complex defect in the walls of the frontal sinuses is impossible [37].
Titanium mesh implants are very widely used for plastic surgery of postoperative and post-traumatic bone defects of the paranasal sinuses and skull [38–41]. In the literature studied, there was work where porous titanium nickelide was used to close perforations of the nasal septum and postextraction fistulas [42]. Structures made of these alloys implanted into the body are deformed in accordance with the laws of elastic behavior of body tissues and ensure long-term harmonious functioning. In addition, porous titanium nickelide, which has physical and mechanical properties close to the parameters of bone tissue (pore sizes, permeability, general patterns of elastic behavior), provides favorable conditions for the ingrowth of tissue structures into the pores and its fusion with the recipient bone [43, 44] . However, even titanium implants can provoke rejection reactions. Therefore, in order to isolate titanium from adjacent living tissues of the body, a coating of biositall, a bioactive material, is applied to the titanium mesh to improve osseointegration and biocompatibility [16, 45, 46].
Of great clinical interest are data on tissue reaction and the course of the wound process during implantation of polymer materials [47, 48]. Thus, for the purpose of plasticizing a bone defect in osteomas of the paranasal sinuses, polyphosphazene endoprostheses [49] and protacryl [26] were successfully used; to close a post-traumatic defect in the upper wall of the maxillary sinus, silicone [50] or Teflon [51] were used. Plastic material made of polyester - “Knitted material for the restoration of bone and cartilage structures” was used to correct the contours of the nasal septum and the walls of the paranasal sinuses [52].
Currently, combined synthetic materials are of greatest clinical interest. Combined forms consist of a polymer matrix and nano-hydroxyapatite as a filler. The emergence of composites of synthetic hydroxyapatite in the form of powders, granules and gels in combination with polysaccharides, chitosan, alginate, hyaluronic acid, collagen protein, peptides, drugs and other drugs has expanded the possibilities of bone tissue restoration [53-55].
In this regard, the development and introduction into the clinic of new materials for plastic surgery of bone walls is relevant.
Characteristics
During the production of Bio-Oss, organic components are extracted from raw materials. Only calcium phosphate is used, which is a mineral base in which there are many microcapillaries and microtunnels.
According to the physicochemical characteristics, Bio Oss is similar to human bone tissue. Hence the positive reaction of the human body to this material, which integrates well with the patient’s primary bone.
The external topography of the implanted materials has a rough surface, which promotes the adhesion of the implanted material, the proliferation of young cells and the rapid synthesis of connective tissue.
The large area of the internal surfaces of the implant promotes intensive ingrowth of blood vessels into it, as well as active and rapid integration and healing of open wounds.
Expert opinion
Igor Yurievich Malinovsky
Maxillofacial surgeon, implantologist
Experience: more than 11 years
Osteoplastic surgery often precedes dental implantation. Especially in cases where the tooth was removed more than a year ago. Without load, the bone sags, atrophies, and its volume becomes insufficient to install an implant. This is why it is so important to restore teeth immediately after their removal. If there are a large number of missing teeth, the only way to do without osteoplasty may be basal implantation with deeper installation of implants into hard layers of bone tissue.
Autogenous osteoplastic materials in dentistry
According to the literature, the autoplastic method most often used in dental surgery is the transplantation of bone obtained from another part of the patient’s body. The first autogenous transplant was tested by the surgeon Walter in 1820.
Over the next two centuries, patient-derived material was traditionally considered the " gold standard"
» osteoplasty. This was not least due to the imperfection of technologies for processing foreign osteoplastic materials and the low development of chemical production, limiting access to more advanced options.
Proponents of autogenous grafts point to high osteogenicity (due to the presence of cells), osteoconduction (due to the content of minerals and collagen) and osteoinductive properties (due to non-collagenous bone matrix proteins).
In terms of their structure, autografts can be cortical, spongy and spongy-cortical. It is generally accepted that when using cancellous bone materials, faster and more complete graft revascularization occurs.
This is possible due to the content of pluripotent cells
, which are able to differentiate and proliferate, participating in osteogenesis. In cortical grafts, these processes occur slowly.
A number of researchers believe that spongy-cortical fragments, due to their strong cortical part, have sufficient mechanical properties, and the spongy component helps to increase osteogenic potential.
Most often, the extraoral sites for collecting osteoplastic material are the lower jaw, less often the pelvic bone, the lateral edge of the scapula, or the rib. According to foreign experts, tissue from the pelvic bone and jaw has a high regenerative potential and is less susceptible to resorption.
In any case, additional intervention is necessary only to obtain autogenous osteoplastic material. This means the involvement of anesthesiologists and surgeons, additional risks and costs.
If an intraoral graft is required for osteoplasty, the optimal donor site is the body or ramus of the mandible, the retromolar region, the mental symphysis and the hump of the maxilla.
The biomaterial is collected under local anesthesia, which simplifies the entire treatment process, but additional trauma and risks remain.
It is worth mentioning that one of the main reasons for refusing this type of osteoplasty is patients’ fear of surgery and the natural desire to complete the treatment with minimal blood (literally).
Despite the obvious advantages of autografts (biocompatibility, infectious safety, regenerative potential), they have a significant drawback. The problem lies in graft resorption over time, mainly when using extraoral grafts
.
It is necessary to remember about age aspects and the tolerance of additional surgical intervention in certain categories of patients.
The method is used with caution in the elderly and children, including due to insufficient bone and the risk of damage to growth plates in children.
The need to harvest bone is always associated with an additional risk of infection of the donor site, blood loss, increased duration of the postoperative period, increased need for painkillers, increased medical costs, etc.
The need to overcome these disadvantages of autotransplantation has led to the rapid development of an alternative method, allotransplantation. For the first time in the world, an innovative method of replacing bone defects, in which another person acts as a donor, was used in 1880 under the leadership of William McEwan.
Splitting of the alveolar process -
Used in horizontal bone resorption to increase the thickness of the alveolar process. Can be performed on both the lower and upper jaws. It must be said that this is the most effective method of expanding the alveolar process today, which also has a low cost (it does not require expensive bone materials and membranes). There are several varieties of such splitting, but we will especially focus on the “Split-Control” technique, which allows for simultaneous expansion and installation of implants.
The content of the “Split-Control” technique (Fig. 5-10) - after detachment of the mucoperiosteal flaps (gum) in the center of the alveolar ridge, a cut is made with a milling cutter or other special tools to the height of the future implant (Fig. 6). Next, a pilot drill is used to mark a hole for the implant(s) and spreaders are screwed into the prepared holes (Fig. 7). By using different sizes of spreaders from smaller to larger, you can increase the width of the ridge and immediately install the implant.
There is always a gap left on the sides of the implant, which is filled with bone material, which, if necessary, can be applied in excess to the outside of the alveolar process, covering it all with a special resorbable membrane (Fig. 9). After which the wound is sutured, and we wait for osseointegration of the implant within 3-4 months.
Bone grafting of the lower jaw (splitting method) –
Advantages of the technique –
- Firstly , thanks to the splitting of the ridge, we get a bone defect that has bone walls on all sides (except on top).
Thanks to this, rapid and high-quality osteogenesis (new bone formation) occurs, because the spongy bone deep in the alveolar process is rich in blood vessels, osteoblasts, mesenchymal cells, growth factors... Speaking of why it is much worse to increase the width of the bone not due to splitting (from within the alveolar process), and do this by externally attaching bone blocks or bone chips outside cortical plastic surgery of the alveolar process (24stoma.ru). The fact is that the outer cortical layer of bone is very dense and there are practically no blood vessels in it. Accordingly, the implanted bone material will take a very long time to grow blood vessels, bone formation will be slower, and there will be a greater risk of failure and complications of such bone grafting.
- Secondly , there is no need for expensive bone materials and membranes, again due to the fact that this is a three-wall defect inside the alveolar process, and not outside it. There are enough inexpensive materials, for example, the bone material "Osteodent-K" and the membrane "Osteodent-Barrier". But if you are principled, then you can also use expensive materials like “Bio-Oss”.
- Thirdly , installation of implants with this technique is possible in most cases immediately. If the implants are installed later, then only 3-4 months will have to pass between operations, which is significantly less compared to other bone grafting methods.
Splitting of the alveolar process: animation and video of the operation
Important: There are several types of splitting techniques. With “Split-Control”, the cutter makes only a cut along the crest of the alveolar process + a pair of vertical cuts to the thickness of the cortical plate. But there is a variation of this method, where an additional horizontal cut is made at the level of the tops of future implants, which leads to complete detachment of the bone block (vestibular cortical plate).
Then this block is fixed with screws, which often break it. With this modification of the technique, implants are not installed immediately, but after 3-4 months. In addition, it is quite traumatic and there is a greater risk of complications. This type of technique should only be used for the thinnest alveolar process (2 mm), but some doctors use it even in cases where this is not necessary.
Bone augmentation of the lower jaw
The operation also has its own specifics, since in this projection there is a large accumulation of nerves, the mandibular canal, the temporomandibular joint, etc. It is important to place the bone carefully, without touching or crushing the nerve endings.
The lower jaw is characterized by the transplantation of a donor composition, which is taken from the area of the wisdom teeth or the chin. The donor block is fixed with metal screws, and the gaps are filled with bone chips. After a few months, once the block has taken root, the screws are removed and you can proceed to the implantation procedure.
The most common question is: is it possible to do without replenishing bone volume? Yes, in some cases it is possible. For example, with express implantation, when a root-shaped implant is implanted immediately after the extraction of its tooth. In almost all other cases, even if a month has passed since the tooth was removed, it is impossible to do without bone tissue augmentation. But this operation guarantees a stable position of the implant - reliability, durability and an ideal result of implantation and prosthetics.
Instead of an epilogue. What are the best biomaterials?
Geistlich Biomaterials, definitely)))). Because RegenerationDay.
Not only patients, but also osteoregenerators would like to hear the answer to this question, and perhaps not at all from me, but from Vladimir Vladimirovich Putin, a more authoritative person. For in all medical forums, in all professional communities, in all discussion forums, there are endless debates about what is better and why.
In my opinion, to answer this question, it needs to be, at a minimum, reformulated. Something like this:
Benefits of demineralized lyophilized bone with proven osteoinductive activity
Among all the materials on the market, one can highlight a product called AlloGro from the largest tissue bank in the United States. This preparation is a demineralized lyophilized bone implant whose osteoinductive activity is determined by testing. The need for this test lies in the fact that the inductive properties of donor tissue are highly pronounced, and conducting a biotest eliminates about 10% of donors for the production of material for implantation. Today, in order to save money, to test for osteoinductive activity, laboratories use cell cultures of the SAOS-2 (osteogenic human sarcoma) type, into which thymidine and donor CMP are placed. As a result, the activity of cell division and the rate of thymidine excretion are determined. These data allow the osteoinductive efficiency to be calculated.
As a result of these clinical studies, the company was able to label the product as “Proven Osteogenic Activity.” One of the risks with allogeneic transplants is transmission of a viral infection such as hepatitis or AIDS. But to date, there have been no recorded cases of infection with any virus, even those infections whose development zone is the dura mater. Today, DLK is the most economical and effective osteogenic material.
Which material is better?
Recently, operations to transplant one's own bone are used less frequently, since taking the material is another operation, a load on the body and general stress. However, dentists do not exclude this method, but are gradually moving to BMR technologies (based on Bone Morphogenetic Protein), which do not require the collection of a donor composition. We are talking about a group of morphogenetic protein tissue growth stimulators that activate processes, and after some time a sufficient volume of bone is formed. The composition is based on molecules that attract natural cells to areas where it is necessary to compensate for bone deficiency. There are no synthetic components or donor bone blocks - exclusively natural mechanisms of tissue regeneration.
Types, sources of origin and composition
In general terms, all existing barrier membranes can be divided into two groups: resorbable and non-resorbable. There are also membranes with a very long period of resorption and, it seems, they are trying to separate them into a separate class, but in my opinion, they should be classified as resorbable, because in the end they still dissolve and disappear. Non-resorbable membranes are made from various bioinert materials (Teflon, PTFE, titanium alloys, etc.), they are used much less frequently, we will talk about them when we consider osteoplasty using the NCR method.
Here and further, we will talk about the most common resorbable barrier membranes in surgical practice.
The main component of barrier membranes existing on the market is collagen, an organic substance of protein nature, the main structural element of connective tissue. The source of collagen for barrier membranes is 98% best friends and, at the same time, human food - pigs. Occasionally, allocollagen (of human origin) or something else (biopolymers, polysaccharide derivatives, etc.) is used.
The main reason for using collagen to produce barrier membranes is its predictable breakdown naturally by collagenase enzymes and the formation of amino acids common to the body. Without unnecessary breakdown products and other LSD.
Anyway. We, the end consumers of barrier membranes, are concerned not so much with production secrets, but with a number of criteria that are important for practice. They are generally similar to what we expect from osteografts and biomaterials in general, and include:
Form factor.
sizes, packaging, etc. The same barrier membrane can be of different sizes. Thus, the Geistlich Bio-Gide we use is available in sizes 16x22, 25x25 and 30x40 mm
And we choose the right size, depending on the scale of the surgical intervention.
Physical and biological properties.
By analogy with osteografts, barrier membranes must have a number of physical and biological properties. Of course, information about the properties is important, first of all, for the doctor, and not for the patient. However, you, friends, also need an idea of the properties to understand how we, doctors, navigate when choosing a barrier membrane to solve a particular clinical problem.
hydrophilicity - well, this goes without saying, because liquid is the main transport medium of the body.
strength – the ability of a barrier membrane to maintain integrity under load and fixation. It should not turn into rags, if we decide to pin it or screw it in, the underlying graft should not erupt, and the stretched membrane should not creep.
elasticity - the barrier membrane must take the shape of the area to which we adapt it. Without unnecessary creases and filing.
adhesion – an ideal barrier membrane literally sticks to the underlying graft and, most often, does not require any special fixation.
We can talk about the properties of barrier membranes for a very long time. And we will do this one day, in an experiment called “M.P.” You, friends, need two things about properties:
– physical properties determine how the barrier membrane behaves during surgery. Does it make the doctor’s work easier and cheaper, or, conversely, complicates it and requires the use of something additional. Pins and screws, for example.
– biological properties determine what happens to the barrier membrane after surgery. They are difficult to measure and practically impossible to study objectively. Therefore, by appealing to biological properties, you can “sell” anything you want. That is why such criteria as “permeability” and “resorption time” are still the subject of fierce disputes, discussions, fights and other quarrels in the professional dental community. And that is why I urge you to believe them as little as possible.
And we just have to consider one more category of biomaterials: