In what cases may the bone fail to take root?
The bone may not take root in cases where it becomes infected, including when the patient violated the schedule for taking antibiotics or did not follow the doctor’s orders.
Much attention is paid to food intake: the patient can simply, out of forgetfulness, bite into something hard, and his stitches will come apart, and the material and bone graft will become infected through the open wound.
The above accounts for 90 percent of cases
when the bone may not take root.
Are there any contraindications to bone grafting?
Of course, there are contraindications to bone grafting. These include
:
- various chronic diseases, incl. diabetes mellitus with high sugar levels,
- the period when the patient takes a number of drugs, including chemotherapy,
- in the period after chemotherapy, when the bone cannot be “touched” at all.
Features of hygiene after bone grafting
After bone grafting it is recommended
:
- use of special surgical toothbrushes,
- the use of toothpaste should be limited, and even better, use special toothpastes for post-surgical interventions,
The main thing when carrying out hygiene is NOT TO INJURY
area of bone grafting! You should try to eliminate contact with this area or reduce it to a minimum.
When can you do without bone grafting?
You can always do without bone grafting when you can install an implant of the required diameter and required length into the remaining bone.
And, in fact, you shouldn’t do bone grafting just to assert yourself. Some doctors suffer from this, trying to prove to themselves or someone else how they can do bone grafting.
But, as they say, the best bone grafting is the one we don’t do: if the patient can be rehabilitated without bone grafting, then it’s better to do just that. Since volume can be added with soft tissues, connective tissue can be transplanted - a graft, or drugs can be added to replace the volume of soft tissues - and achieve an excellent result!
Donor materials
The following can be used as donor materials:
- Protein molecules that are similar in structure to the original bone. They are responsible for starting the process of cell regeneration.
- Membranes made of collagen and impregnated with a regenerating composition.
- Hydroxyapatite compounds, membrane barriers and bone granules.
- Biologically active compounds together with a variety of distracting drugs.
The best solution seems to be the combination of several materials when performing guided bone regeneration. Not only bone tissue is suitable for this, but also blood cells, synthetic fibers, and so on. If you add the patient's blood to crushed bone granules, regeneration will be more active and survival rate will improve.
Stages of guided bone regeneration surgery
Guided regeneration around implants is performed in several stages:
- Using a scalpel, the doctor removes the periosteal flap. During tissue incision, the point is taken into account that in the future the membrane installed in the sinus should not touch the root system. The distance should be about 4 mm, otherwise the proliferation of bacteria and the development of an inflammatory process in the oral cavity cannot be avoided.
- The optimal size of the implanted plate for a particular case is selected, with an emphasis on the specifics of soft tissues and parameters of bone restoration.
- Decortication of the surface of the hole is carried out. For this purpose, spherical burs and fissures of compact sizes are used. In some cases, the doctor uses thin drills. Provides access to the drugs necessary for the rapid restoration of the affected area and to activate blood circulation in the jaw.
- The membrane is installed. Titanium feints are used, the attachment location is chosen in an inconspicuous area. After installing the first side, regenerating drugs are administered, only after that the doctor begins to fix the second side. It is important to achieve maximum fit, otherwise soft tissue will grow into the formed folds, which will negatively affect the result of the dental operation.
- The flaps are sutured over the membrane. It is important that the surgeon uses the thinnest threads. It is also necessary to match the boundaries of the incisions as accurately as possible - in this case, healing is accelerated and the risk of inflammation is eliminated when food debris enters the sinuses.
- At the final stage, the doctor disinfects the suture. The implant is installed after final bone regeneration.
If you are interested in restoring your teeth using soft tissue grafting, start with a consultation. Visit the official website of the medical center - make an appointment with a doctor online. During the initial examination, the doctor will diagnose existing diseases, if any, and prescribe treatment.
What implants are used after bone grafting?
Are there “special implants” that are recommended in cases of bone grafting? Both with bone grafting and without bone grafting, it is necessary to use implants only from good, proven manufacturers, those that have a good clinical base. For example – Straumann, Nobel, Ankylos, Xive, Astra Tech.
There are a number of other implant systems that give good results. But at the German Implant Center we use only the best implant systems, only premium ones.
Alternative Methods
Removable dentures Recommended if there are absolute contraindications to implantation or if there is a limited budget
ReSmile Modern technology for rapid restoration of teeth with complete edentia with the installation of a permanent prosthesis
Mini-implants Removable prosthetics with mini-implants MDI
Article Expert
Nesterenko Alexey Pavlovich Surgeon-implantologist, doctor of the highest category
Work experience: more than 11 years
How is implantation performed during bone grafting?
Implantation during bone grafting can be carried out either simultaneously with bone grafting, or delayed - when the implants are installed in the new “grown” bone.
As an experienced implant surgeon, in my practice, in 80-90 percent of cases I perform bone grafting at the same time
with implantation.
I will explain why I perform plastic surgery with implantation at the same time, and what is the advantage of this approach. Bone grafting itself requires a long healing period, from 4 to 9 months. And if we maintain this period and then do implantation, then we have to wait another 4 months. That is, the time frame in this case increases significantly.
And if I do implantation along with bone grafting, then the implant takes root along with the bone. A good implant has an excellent osteogenerating surface, and when fused, an excellent result
.
This reduces the patient’s rehabilitation time. And most importantly, the patient DOES NOT NEED
second surgery. We understand that a large number of surgical interventions do not improve trophism, mucous membranes, or bone tissue.
Everything we do at the German Implant Center, from tooth extraction to implantation, is carried out as atraumatically as possible for the patient.
How many implants are placed during a total restoration?
We specialize very broadly in total implant rehabilitation. In the upper jaw, 6-8 implants are recommended according to our protocol; in the lower jaw, 6 implants are sufficient for total rehabilitation.
Often, implantation occurs simultaneously with the installation of temporary teeth, that is, the patient leaves the clinic “with teeth”, and not on the second or third day, but on the same day when implantation is done:
Preliminary implantation planning is carried out using CBCT, the implants are placed in the required positions.
After this, a surgical template is made, according to which the implants are installed. And based on the same computed tomography (CBCT) and images, a temporary structure is made that will be attached to the implants installed for the patient.
And it turns out the so-called “full case” is when the patient comes, if necessary, if circumstances require it, teeth are removed (or they have already been removed/lost earlier), implants are placed on the patient and an orthopedic structure is fixed - his new teeth.
Preparing for surgery
Like any other operation, sinus lift requires patient preparation. The surgeon will never decide to operate until he is sure that the patient’s maxillary sinuses are normal. To do this, a detailed examination is carried out with mandatory x-rays. If there is the slightest deviation from the norm, surgery cannot be performed.
Also, in preparation for a sinus lift, a complete examination of the patient’s body condition is carried out.
Perhaps it wouldn’t hurt to give some good advice here. If the clinic where you are planning to go for a sinus lift does not have a 3D computed tomograph, then it is better to look for a more reputable clinic that has this expensive medical device. The fact is that only it allows you to get a complete picture of the state of a person’s internal organs.
Studio Dent purchased a computer tomograph for 6 million rubles, and this was done not for the sake of advertising or profit, but for the sake of obtaining impeccably accurate examination results.
Also, in preparation for surgery, the patient may be prescribed a course of medication. Most often this is taking antibiotics to prevent bacterial infections. Steroids may also be prescribed to promote rapid wound healing and reduce the likelihood of inflammation.
On which jaw does tooth bone resorption occur faster?
How quickly does a deficiency of bone and bone tissue occur in the absence of a tooth?
In fact, tooth bone tissue decreases faster in the upper jaw, since the upper jaw is softer and more porous. In the lower jaw, the bone also disappears quite quickly, since the vestibular plate near the teeth is quite thin. Six months after tooth loss, quite severe atrophy of bone tissue occurs, and the atrophy progresses. And therefore, in order to avoid atrophy, it is advisable to do implantation simultaneously immediately after tooth extraction.
This format is the regular, daily work of the specialists of the German Implantology Center. For example, a patient comes with a crack in the root of a tooth - the tooth must be removed. We can go with two options:
Option 1.
We can remove the tooth and 3 months later implant the tooth into the patient.
But during these three months, shrinkage of the bone tissue still occurs, since - I said earlier - the vestibular bone plate is very thin. And in this case, the patient undergoes 2 surgical interventions
: the first is tooth extraction, the second surgical intervention is the installation of a dental implant.
Option 2.
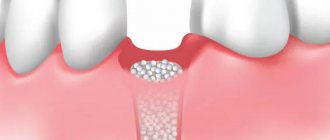
In our practice, we recommend and practice the second option. This is a one-step implantation, when the patient has a tooth removed, an implant is installed, and in order to avoid collapse of the bone tissue in the places where the roots of the tooth used to be, these places are filled with a bone graft. Due to graft filling, we do not have tissue “collapse”; the contour of both the gums and the jaw bone tissue is preserved. Which, in turn, is very difficult to achieve with delayed, delayed implantation.
Who can undergo bone grafting?
Who are potential patients for bone grafting, and what are the age restrictions for it?
This is a bit of a tricky question :). The oldest patient I have performed bone grafting on is a 75-year-old patient, a wonderful, purposeful woman. She had bilateral terminal defects on her lower jaw. She really wanted implantation and refused a removable structure.
I performed bone grafting on this woman at the same time as implantation. And literally 6 months later she was fitted with prosthetics. And everything went great.
In the case of the patient’s age, the main thing is that he has no contraindications. Perhaps there are age restrictions, but they are not so pronounced, because, although trophism deteriorates with age, regenerative abilities decrease, but the main thing is the presence of contraindications. You need to look at the tests, and if the patient is healthy at 75 years old, then why not?
How much does a sinus lift cost?
At the Studio Dent clinic, the pricing system is based on obtaining a minimum profit sufficient to maintain the clinic and pay for the work of medical personnel. At the same time, the cost of the operation depends on five factors.
- Type of surgery (closed sinus lift, balloon sinus lift, open sinus lift).
- Type of anesthesia (general anesthesia, local anesthesia, combined anesthesia).
- A type of synthetic bone material.
- Type of diagnosis.
- Number of required tests.
In order not to mislead our patients, our price list is designed as conveniently as possible; it does not use complicated terms that people do not understand. Prices are indicated as a package for each type of operation, and not for individual procedures included in it.
Each sinus lift package includes the following paid procedures:
- preparation for surgery;
- anesthesia;
- the operation itself.
- additional bone tissue (if required during the operation);
- suturing postoperative wounds and their subsequent removal;
- postoperative observation by the attending doctor;
- a set of medications that should be taken after sinus lift;
- X-ray panoramic image.
Please note that an open sinus lift costs more than a closed sinus lift. This is explained by the fact that this type of operation is much more complex and requires additional materials.
How to do without bone grafting
Is it possible to do without bone grafting and sinus lift?
Yes, in some cases you can do without bone grafting. But you need to understand that if the patient does not have bone tissue, and we install an implant, the crown will hang over the gum, and something from food will constantly get clogged there. That is, it is aesthetically unsightly, and all the food will be stuffed there, the patient will always have a “pocket of food supplies” from yesterday and the day before yesterday.
Option with a smaller diameter implant
You can place an implant of a smaller diameter, and at the same time we can carry out soft tissue regeneration - replant the mucous membrane (this can be connective tissue from the palate, from the tubercle of the upper jaw). And thus we achieve replenishment of the volume of soft tissues. Due to this, aesthetics are visually improved and hygiene problems are eliminated.
Whenever it is possible to avoid various surgical procedures, but not at the expense of quality, then they should be avoided.
That is, surgery for the sake of surgery - it is not needed
.
Possible postoperative complications
After a sinus lift, the following problems may arise:
- acute chronic sinusitis;
- swelling of the palate;
- sinusitis;
- increased body temperature;
- rupture of the mucous membrane inside the maxillary sinus or its perforation;
- chronic runny nose;
- bleeding from the nose and at the operation site.
All these troubles can occur due to insufficient qualifications of the doctor and the use of low-quality materials and instruments.
Work examples
All works
Implantation for 2 jaws with artificial gum
Complete restoration of the upper jaw on implants
Complete restoration of the upper jaw using a zygomatic implant
Stage III periodontal disease: complex dental implantation Restoration of both jaws in 4 days
Sinus lifting with simultaneous implantation
Implantation of both jaws with ROOTT implants for stage II periodontal disease
Restoration of two jaws with one-stage implantation using sinus lift
Sinus lift with simultaneous implantation
All works
Sign up for a consultation
three ROOTT specialists + diagnostics as a gift