From this article you will learn:
- what is tooth root cement,
- its structure and functions,
- histological preparations.
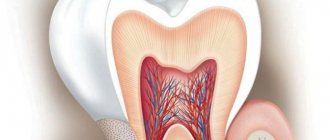
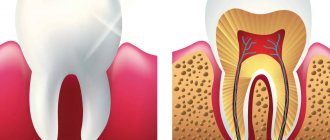
Dental cement (cementum) is a highly mineralized tissue, reminiscent in its structure of coarse-fiber bone, which covers the root of the tooth (up to its neck) with a thin layer. But unlike bone tissue, root cement is not subject to constant restructuring, it does not have vessels, and its trophism is carried out through the usual diffusion of nutrients dissolved in the main amorphous substance in the periodontal structure.
The main function of cement is to form the ligamentous apparatus of the tooth (periodontal attachment), which holds the tooth in the alveolus, and also contributes to the redistribution of chewing pressure from the tooth to the alveolar bone. Let us recall that periodontal fibers begin to grow simultaneously - both from the side of the root cement and from the side of the compact lamina of the alveoli. Next, with the help of immature collagen (procollagen) in the center of the periodontal fissure, the ends of these fibers are tied together, bundles of fibers are formed.
Tooth root cement: diagram and photo
The cementum layer is present only on human teeth, as well as on the teeth of other mammals. In the area of the tooth neck, the thickness of the cement is less - from 20 to 50 microns, while in the area of the root apex - from 100 to 150 microns. I think you are familiar with the fact that “secondary dentin” is produced by odontoblasts throughout life, and in the same way, constant formation of cement on the root surface occurs throughout life. And therefore, if you live to retirement age, the cement of your teeth will most likely have time to at least triple its thickness (Fig. 3).
Structure of tooth dentin –
Dentin consists of calcified intercellular substance, which is penetrated by the so-called “dentinal tubules” (dentinal tubules), which ensure trophism and mineralization of dentin. Dentinal tubules run radially, in the coronal part of the tooth - in the direction from the wall of the pulp chamber to the enamel-dentin border, and in the root part of the tooth - from the wall of the root canal to the surface of the tooth root. However, if in the root part of the tooth, as well as in the area of the occlusal surface of the tooth crown, the dentinal tubules have an almost straight shape, then in the lateral parts of the crown they will already be S-shaped.
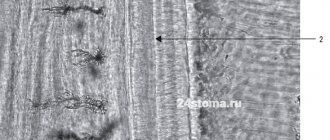
Dentinal tubules (electron microscopy) –
The diameter of the tubules ranges from 0.5 to 4 microns, and they will be wider in the internal parts of the dentin and gradually narrow outward (like a flattened cone). Inside the tubules there are processes of odontoblasts, unmyelinated nerve fibers, and tissue fluid also circulates. The odontoblasts themselves are located outside the dentin - their bodies are located in the superficial layer of the pulp, and their processes, passing along the entire length of the dentinal tubules, end in the area of the enamel-dentin border (Fig. 8).
The lateral canals extend from the dentinal tubules in a perpendicular direction. There are especially many of them in the predentin and inner layers of peripulpal dentin (100–200 µm from the border with the pulp). There are quite a few of them in the middle sections of dentin and again become numerous at the periphery - in the area of mantle dentin. In the lateral canals there are lateral branches of the processes of odontoblasts, which anastomose with each other. Let us recall that it is odontoblasts that participate in the formation of the organic dentin matrix and its further mineralization.
Odontoblasts, predentin and dentinal tubules (histology) –
Please note that on the histological specimen (Fig. 6) predentin looks like a light stripe, turning into a zone with spherical formations of a darker color (globules). The predentin layer has minimal mineralization and consists mainly of an organic matrix - intertwined collagen fibrils (Fig. 7). Spherical formations at the border of predentin and peripulpar dentin are nothing more than “calcospherites”, which are foci of mineralization. Low-mineralized dentin located around such globules is called “interglobular.”
Subsequently, the globules merge, forming homogeneous, highly mineralized dentin. It is also worth noting that when the dentinal tubules approach the enamel-dentin border or the cementum layer, their ends form large terminal branches (similar to tree branches). A number of terminal segments of dentinal tubules penetrate even through the enamel-dentin boundary, forming the so-called “enamel spindles”. According to most authors, these formations are involved in the mineralization of deep layers of enamel.
Architectonics of dentinal tubules –
The density of the tubules differs in different layers of dentin. Some of them are most densely located in the peripulpal dentin, where there are from 50,000 to 75,000 of them per 1 mm2 of dentin. For 1 mm2 of the mantle layer of dentin there will be only from 15,000 to 30,000. But let us draw your attention to the fact that in this case it decreases not the number of tubules as such, but precisely the density of their location in the surface layers of dentin (due to their radial direction and with a simultaneous increase in the area of the outer layers).
Reasons for additional formation of cement –
In case of periodontitis and chronic periodontitis, when the enamel on the occlusal surfaces is worn away, when the load on the tooth increases, as well as in the absence of an antagonist tooth, intensive deposition of cement occurs in the area of the apical third of the root (hypercementosis is formed, Fig. 3).
Trauma to the tooth root, as well as orthodontic treatment, can also lead to this. In addition, there is also such a formation as “cementicle”. This is nothing more than a round-shaped formation consisting of cement, located in the periodontium. They arise as a result of mineralization of microvessels in the area of islets of Malasse epithelial cells.
Structure of dentinal tubules –
Dentinal tubules pass in the so-called dentinal tubules. The wall of each dentinal tubule is formed by the so-called “peritubular dentin,” which is characterized by a very high degree of mineralization and the absence of collagen fibers. Between the dentinal tubules there is the so-called “intertubular dentin”, which is characterized by a lower degree of mineralization and a large number of collagen fibers (fibrils). Dentinal tubules are hollow inside, which is why they are often called dentinal tubules.
Each tube is internally coated with a thin layer of organic matter - this layer contains a high concentration of glycosaminoglycans and is commonly called the Neumann membrane. In the center of the dentinal tubules there are processes of odontoblasts (Toms fibers). The space between the odontoblast process and the wall of the dentinal tubule is filled with dentinal fluid, which is similar in composition to blood plasma. In addition to the processes of odontoblasts and tissue fluid, they also contain non-myelinated nerve fibers (however, they can only be found in peripulpar dentin).
Scheme of the structure of dentin –
Peritubular and intertubular dentin –
During the process of dentinogenesis, intertubular dentin, located between the dentinal tubules, is formed earlier than peritubular dentin (24stoma.ru). The deposition of peritubular dentin occurs from within the already formed dentinal tubules (the processes of odontoblasts take an active part in this). The thickness of peritubular dentin from the pulp end of the tube is from 40 to 50 nm, and from the enamel-dentin border from 500 to 700 nm.
As we said above, peritubular dentin has a significantly higher mineralization. For example, the content of hydroxyapatite in it will be 40% higher than in intertubular one, but there are practically no organic components in it. This leads to the fact that when moderate caries occurs, peritubular dentin will be destroyed much faster than intertubular dentin. And as a consequence, the ongoing processes of demineralization will lead to the expansion of dentinal tubules and an increase in dentin permeability, including for pathogenic bacteria.
In turn, intertubular dentin contains many organic components, for example, calcified collagen fibrils with a diameter of about 75 nm (hydroxyapatite crystals are located along the axis of the fibrils). Collagen fibrils form a so-called “framework”, which serves as a basis for the deposition of mineral salts. Below you can see what the collagen framework of dentin looks like in electron microscopy images taken after its forced demineralization.
Innervation of the pulp -
The common sensory or afferent nerve for the maxillary and mandibular teeth are the II and III branches of the trigeminal nerve (i.e., the maxillary nerve and the mandibular nerve). In turn, nerves depart from them, which form plexuses - the superior dental plexus in the upper jaw and the inferior dental plexus in the lower jaw. In turn, bundles of myelinated nerve fibers branch off from these plexuses, which penetrate into the tooth cavity along with blood vessels - through the apical openings at the apexes of the roots. And, accordingly, forming a neurovascular bundle (tooth pulp) there.
The nerve fibers form a subodontoblastic nerve plexus, which is located under the layer of odontoblasts (also called Rashkov's plexus). Unmyelinated nerve fibers depart from this plexus, which are directed to the peripheral areas of the pulp, where they seem to entwine the odontoblasts, forming the so-called “nadodontoblastic plexus” between the odontoblasts and predentin. Some of the nerve fibers end in this plexus, but the rest of them penetrate into the dentinal tubules.
Organic dentin matrix –
The organic matrix of dentin is located between the dentin tubules (in intertubular dentin). It consists of collagen fibrils and an amorphous substance located between them. It is interesting that the direction of collagen fibrils and their structure will differ in the mantle and peripulpar layers of dentin. This is due to the fact that during primary dentinogenesis, the organic matrix of mantle dentin is first produced, and only then the matrix of peripulpar dentin.
In mantle dentin, fibers running in a radial direction, parallel to the course of the tubules (“Korff fibers”) will predominate. But the peculiarity of Korff fibers is not only their directionality, but also the fact that they will consist of fairly thick fibrils united into conical-tapering bundles. Moreover, it is worth clarifying that the radial-parallel direction of Korff fibers is more typical for that part of the mantle dentin that is closest to the occlusal surface of the tooth crown. And on the lateral surfaces of the crown and in the root area, the Korff fibers acquire an increasingly oblique direction.
As we said above, the matrix of peripulpal dentin is formed later than that of mantle dentin. Odontoblasts during this period synthesize much thinner fibrils, which intertwine with each other (see figure below). These fibers will be located tangentially, i.e. they extend from the dentinal tubules at almost a right angle (they are called “Ebner’s fibers”). But collagen fibers are not the only component of the organic dentin matrix, and we must not forget about the amorphous substance surrounding them.
Collagen fibrils in peripulpar dentin –
Amorphous substance –
Collagen fibers are surrounded on all sides by a basic amorphous substance, which consists mainly of glycosaminoglycans (chondroitin sulfates). In addition to them, the organic matrix includes a large amount of non-collagen proteins (their share is about 20% of the organic dentin matrix). The amorphous substance also contains proteoglycans, which are formed as a result of the combination of chondroitin sulfates and non-collagenous proteins.
Non-collagenous proteins play an important role in the processes of dentin mineralization. Below we have listed their main varieties -
- calcium binding proteins
- bone morphogenetic proteins (BMPs),
- glycoproteins (fibronectin, osteonectin),
- calcium ATPase and alkaline phosphatase,
- collagenases and collagen-digesting enzymes necessary for the restructuring of the organic matrix.
In the organic basis of dentin, lipids (glycolipids and phospholipids) have also been identified, probably participating in the mineralization of the matrix.
Nerve fibers -
Unmyelinated nerve fibers penetrate into dentin from the peripheral parts of the pulp, and they can only be detected in predentin (they penetrate into it to a depth of several micrometers, and only rare fibers - to a depth of 100 to 200 microns). In addition, nerve fibers are not found in all, but only in some dentinal tubules. In the more peripheral layers of dentin, there are no nerve endings at all, and in this case the main role in the formation of pain impulses is played by dentinal fluid (changes in hydrodynamic conditions).
Cementocytes
The 2nd picture shows two cementocytes (C) with their intermittent branching processes (O) emerging from a calcified cement block. Cementocytes are stellate cells located in the corresponding lacunae (La) inside the cellular cement.
The cell processes are very short and lie in small tubules. Sometimes they come into contact with the processes of neighboring cementocytes. The cell body includes a massive nucleus, several mitochondria, the Golgi complex, and well-developed cisterns of the granular endoplasmic reticulum. The supply of nutrients to cementocytes occurs due to diffusion from the periodontal ligament.
Collagen fibers in the cementum are collected in thin plates (P), located concentrically around the dentin.
Features of the inorganic matrix –
Dentin consists primarily of calcium phosphate (in the form of hydroxyapatite crystals), as well as small amounts of calcium fluoride and carbonate.
Hydroxyapatite crystals in dentin are much smaller and thinner when compared with tooth enamel, and have the following dimensions - length 20 nm, width 18-20 nm, thickness 3.5 nm. Those. The crystals are quite small and needle-shaped. Electron microscopy made it possible to establish that these crystals are located not only outside the collagen fibers, but also inside them (located even between the collagen fibrils). Dentin is characterized by a special form of deposition of crystals of mineral salts. If, for example, in the main substance of bone tissue the deposition of mineral salts occurs evenly (in the form of tiny crystals), then in dentin the mineralization process occurs in several stages. At the first stage, the formation of spherical crystalline structures occurs (in the form of “globules” - calcospherites), between which areas with non-calcified or slightly calcified basic substance - interglobular dentin - are still preserved.
Globular and interglobular dentin (histology) –
Globular and interglobular dentin are best visible at the border of peripulpar dentin and predentin (in the coronal part of the tooth), because It is in this zone that mineralization of secondary-formed dentin actively occurs. In addition, it is in this zone that the largest calcospherites can be found. Gradually, the globules increase in size and merge, forming homogeneous, highly mineralized dentin.
What are Owen's lines and Abner's lines?
Primary (physiological) dentin is formed during the period of tooth formation and eruption. It is produced by odontoblasts at a rate of approximately 4-8 µm/day, and the activity of odontoblasts has periods of activity and rest. This periodic change in odontoblast activity leads to the presence of so-called growth and contour lines in dentin.
Owen's contour lines reflect the daily rhythm of dentin deposition by odontoblasts. They are located at right angles to the dentinal tubules and correspond to “rest periods” in the activity of odontoblasts. During these periods, much less intense mineralization of dentin will occur - with the formation of very small interglobular spaces. The number of Owen lines can increase in pathological conditions of the body that affect the processes of mineralization of hard dental tissues.
Ebner's growth lines correspond to a slower 5-day cycle of formation of the organic dentin matrix by odontoblasts, i.e. periods of less mineralization of the dentin base substance.
Dead pathways in dentin –
Also, so-called dead paths (on thin sections of teeth) can be found in dentin, which arise when some of the odontoblasts die. Some authors say that only the exposure of 1 mm of the child’s area leads to the death of up to 30,000 odontoblasts. At the same time, the processes containing in the dentinal tubules undergo decay; accordingly, the cavities of the dentinal tubules will be filled with decay products and gaseous substances.
Due to the presence of gases, such dentinal tubules (dead paths) appear black on polished sections of teeth. By the way, the term “dead paths” was coined by E. Fish. It is also worth noting that the sensitivity of dentin in such areas is reduced, and from the side of the dental pulp in these areas there will be increased production of tertiary dentin.
Secondary and tertiary dentin –
Secondary dentin is deposited (from the pulp chamber side) throughout the life of the individual, which leads to a gradual reduction in the volume of the pulp chamber. Secondary dentin, like primary dentin, is produced by odontoblasts. Secondary dentin differs from primary dentin (formed during the formation and eruption of teeth) by a less regular structure, which is expressed in a change in the direction and number of dentinal tubules and collagen fibers, as well as a lower degree of mineralization. The size of the dentinal tubules itself also decreases.
Deposits of secondary dentin occur more actively in the area of the roof of the pulp chamber, as well as in its side walls. In addition, secondary dentin is actively deposited in the area of the bottom of the pulp chamber (in multi-rooted teeth). In connection with all this, the shape of the pulp chamber gradually changes - the pulp horns become flattened, its volume decreases. An interesting fact is that in men the intensity of secondary dentin deposition is higher. In addition, it is noted that with age, the intensity of secondary dentin deposition decreases.
Another type of dentin is the so-called “tertiary dentin” (dentinum tertiarium), which is also called reparative or irregular. Unlike secondary dentin, which is produced fairly evenly from the inner surface of the pulp chamber, the formation of tertiary dentin occurs locally. Local dentin formation is caused by the influence of strong irritating factors on the tooth, for example, this occurs when the enamel is destroyed or increased abrasion, or dentin is exposed.
With slowly developing caries, the production of tertiary dentin allows, for some time, to prevent the penetration of pathogenic bacteria and their toxins into the pulp. Thus, tertiary dentin performs a protective function. It is also worth noting that tertiary dentin is also characterized by the incorrect direction of the dentinal tubules, or they may be completely absent.
Tooth dentin: histology
Below you can see the histology of tooth tissue in stunning resolution, as well as an excellent lecture on dentin morphology in English (if you wish, you can turn on subtitles and select translation from English into Russian in the settings).
Functions
Dentin performs such tasks as protective, trophic, sensory. The first function is to create a protective layer of the pulp and prevent pathogens from penetrating into the deeper layers. With the development of infectious processes, the pulp begins to secrete a special replacement dentin, creating an additional shell.
The second function is trophic, that is, dentin provides the necessary permeability. The layer of material is penetrated by tubules that conduct dental cerebrospinal fluid between the enamel and the layers located below. In addition, such tubules provide nutrition and innervation to tissues.
Dentin is extremely susceptible to any influence, including pain. With the development of inflammatory and other processes, pain appears, which signals a developing problem. This sensitivity protects the tooth from serious damage.
Age-related changes in dentin –
We have already said above that with age, the deposition of secondary and tertiary dentin occurs, which also leads to a decrease in the size of the pulp. But in the teeth of older people you can often notice areas of dentin in which mineral salts are deposited not only in the main substance, but also inside the dentinal tubules themselves (this occurs against the background of degeneration processes of odontoblast processes). As a result, complete obliteration of the tubule lumen occurs, i.e. their physiological sclerosis.
Obliteration of the lumen of the tubules leads to a decrease in tooth sensitivity. In addition, the refractive indices of light in the tubules and in the main substance are aligned in this case, and therefore such areas of dentin appear transparent. Accordingly, such dentin is often called “transparent” or “sclerotic.” The formation of transparent dentin most often occurs first in the apical part of the root, and then slowly spreads towards the coronal part of the tooth. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Therapeutic dentistry” (Politun, Smolyar), 5. “Histology of the oral cavity” (Glinkina V.V.).
Fact one: color component
One of the most common misconceptions is that the color of a tooth is the color of its enamel. In fact, the color characteristic directly depends on the dentin, which determines the shade of the smile. Although the enamel is the strongest part of the tooth, it is still transparent, and the color of soft dentin is visible through it. The palette ranges from white to gray and yellowish.
Don't be upset if your smile is not snow-white. Today you can whiten your teeth in many ways - from going to the dentist and using pastes with a dispersed phase to using specialized preparations and devices. But the main thing is the health of the teeth, their strength and beauty. Those with yellow teeth, as it turns out, are incredibly lucky, because their bodies are saturated with minerals, which means no bacteria are scary. As you know, yellow teeth are not necessarily a lack of proper care; often the color is transmitted genetically.
Interesting! In the old days in Rus', teeth were whitened with birch charcoal, but doing this with gunpowder or salt was strictly prohibited.