- Causes and risk factors
- Localization
- Metastases
- Symptoms of Oral Cancer
- Stages of the disease
- Treatment
- Prognosis and survival
- Prevention
Malignant tumors of the oral cavity account for about 6% of all cancers in general. Based on the histological structure (type of tumor-forming cells), the following types are distinguished:
- Tumor of epithelial cells - cancer
- Tumor of connective tissue cells - sarcoma
- Melanoma
Each type includes several varieties.
Several groups of precancerous diseases are also distinguished separately. Precancerous diseases of the oral cavity are divided into:
- Obligate - with a high incidence of malignancy. These include Bowen's disease, warty precancer, limited hyperkeratosis, Manganotti cheilitis.
- Optional - with a lower incidence of malignancy. This group includes the verrucous form of leukoplakia, papillomatosis, erosive-ulcerative and hyperkeratotic forms of systemic lupus erythematosus and lichen planus, post-radiation stomatitis and post-radiation cheilitis, keratoacanthoma.
Among malignant tumors of the oral cavity, cancer is the most common.
Oral cancer, in turn, is divided as follows.
- Intraepithelial carcinoma (Carcinoma in situ, cancer in situ) is characterized by the absence of invasion into the basement membrane, despite the malignancy of the neoplasm.
- Squamous cell carcinoma is the most common.
Symptoms of advanced oral cancer
You may have any of the following symptoms:
- persistent pain in the lips, mouth, or both;
- a lump on the lips, neck, or mouth that does not go away;
- white or red spots on the gums, tongue, or cheeks;
- persistent bleeding, pain, or numbness in the mouth;
- persistent sore throat;
- feeling as if something is stuck in the throat;
- problems chewing or swallowing;
- pain while chewing food or swallowing;
- swelling, which causes dentures to fit poorly or cause discomfort;
- voice change;
- ear pain;
- inability to open mouth.
to come back to the beginning
Diagnosis of advanced oral cancer
To check if you have oral cancer, you will need to have a biopsy (a procedure that takes small samples of tissue). During a biopsy, your healthcare provider will remove a small piece of tissue from the area where the cancer may be located. This tissue is examined for the presence of abnormal or cancerous cells. It will take at least 5 business days to receive biopsy results. The healthcare professional will then explain the diagnosis to you.
Your healthcare provider may also order other tests, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to help you Find out if the cancer has spread to other areas.
to come back to the beginning
Causes and risk factors
The causes of the development of malignant neoplasms of the oral cavity can be divided into local and general risk factors.
Common factors include age, a history of various hazards (exposure to radiation, etc.), and hereditary predisposition.
Local factors are local factors affecting the oral cavity. These include chewing nasvay (tobacco- and drug-containing mixtures), smoking, the habit of drinking scalding hot drinks, chronic traumatization of the mucous membrane (tooth fragments, deformed dentures), as well as the presence of precancerous diseases. A separate risk factor for detecting the disease in later stages is the lack of annual dental examinations.
It is the neglect of preventive visits to the doctor that prevents the diagnosis of cancer at early, treatable stages, detection and treatment.
Information about surgery to treat advanced oral cancer
Surgery is the most common treatment for advanced oral cancer. Its goal is to remove all cancerous tissue. Depending on the surgery, you may need tissue, muscle, or bone reconstruction. In this case, a plastic surgeon will work with a surgeon who specializes in the head and neck.
A surgeon who specializes in the head and neck may refer you to an oral and maxillofacial surgeon. If necessary, they will examine your teeth and make a denture. A prosthesis is a device that replaces a removed body part.
The extent of the operation depends on how the head and neck surgeon removes the cancerous tumor.
- Some tumors are removed through an incision (surgical cut) in the jaw. An incision is made between the 2 lower front teeth. Once the incision is made and the tumor is removed, the jaw is reattached using a metal plate and screws.
- If the cancer is close to the jaw or only affects a small part of it, only that part of the bone is removed.
- If the cancer affects a large part of the bone, that part of the jaw is removed completely.
- Sometimes tissue, muscle, bone, arteries and veins may be taken from another part of the body to replace those that were removed. This is called a free flap.
- You may also need to have lymph nodes in your neck removed. The tumor and lymph nodes will be sent to the Pathology Department for examination. It will take at least 1 week to see results.
to come back to the beginning
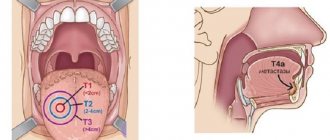
Stages of the disease
There are 4 stages of development of palate cancer.
Stage 1. A tumor within the palate, soft or hard. The lymph nodes are not damaged, there are no metastases. There are no clinical manifestations of the disease.
Stage 2. The cancer remains within the palate, the tumor grows, reaching up to 4 centimeters in diameter. It can be seen during an examination at the dentist or felt by the sick person himself.
Stage 3. The tumor begins to grow into neighboring tissues. The lymph nodes are damaged, but there are no metastases yet. The symptoms are pronounced.
Stage 4. The tumor grows even larger, and neighboring organs are damaged by it. Distant foci of metastases appear. The patient's condition worsens significantly. Cancer is progressing rapidly.
Tracheostomy
Sometimes surgery to treat advanced oral cancer can cause swelling in the throat. In this case, your surgeon may perform a tracheostomy to make sure you can breathe normally. A tracheostomy is an operation to create a surgical opening in the windpipe to make breathing easier and protect your airway. Before your surgery, your healthcare provider will discuss with you whether you will need a tracheostomy.
During a tracheostomy, your surgeon will make a hole in your neck and insert a tracheostomy tube into your trachea (windpipe). This will allow you to breathe easier. If you are having a tracheostomy, your nurse will give you the resource Care after a tracheostomy.
You will also have a tracheostomy if your surgery involves certain types of reconstruction or free flaps.
A nurse will care for your tracheostomy while you are in the hospital. Any mucus that forms will be removed using a suction tube. Keeping your airways clear will make breathing easier and reduce the risk of pneumonia.
The tracheostomy tube will be removed when the swelling in your airway has subsided and you can breathe normally. If you still have a tracheostomy after discharge, your nurse will teach you how to care for it.
to come back to the beginning
Prevention measures
Not all oral and oropharyngeal cancers can be prevented, but the risk of developing these cancers can be significantly reduced by avoiding certain risk factors.
Limit smoking and alcohol
Tobacco and alcohol are among the most important risk factors for the development of RPD. Not starting to smoke is the best way to limit your risk. But quitting tobacco also reduces the risk of developing cancer, even after years of use. The same applies to alcohol.
Preventing HPV infection
In recent years, vaccines have become available that reduce the risk of contracting certain types of HPV. These vaccines were originally used to reduce the risk of cervical cancer, but have been shown to reduce the risk of other HPV-related cancers such as penile, anal, vulvar, and vaginal cancers. HPV vaccination also appears to reduce the risk of RCC, although this has not yet been proven.
Limiting exposure to UV radiation
Ultraviolet radiation is a risk factor for the development of RPR. If possible, limit the time you spend outside during the middle of the day, when the sun's ultraviolet rays are strongest. If you are out in the sun, wear a wide-brimmed hat and use sunscreen and lip balm with a sun protection factor (SPF) of at least 30.
Maintaining a Healthy Diet
Poor diet has been linked to RCC, although it is not entirely clear which substances in healthy foods may be responsible for reducing the risk of these cancers.
After operation
Communication after tracheostomy
If you have had a tracheostomy, you may not be able to speak when you first wake up after surgery, but you will be able to communicate in writing. The nurse will give you a pencil and paper. You can also answer yes or no questions by nodding or shaking your head. You may also be given a tablet to facilitate communication. The tablet comes with an app to help you communicate your needs. Your nurse will teach you how to use the tablet.
Compression boots
You will be wearing compression boots while you are in bed. These boots put gentle pressure on your calves, which prevents blood clots. They will be removed when you are able to get out of bed and walk. If you have surgery without a free flap, you will be able to get out of bed and walk the day after surgery. If a free flap was used during surgery, this will occur somewhat later, depending on the location of the free flap. Every day your physical activity will increase.
Nutritional tube
If you find it too difficult to eat and drink, you may have a feeding tube placed after surgery. Depending on the surgery, you may be unable to eat for a week after surgery. Your healthcare provider will provide you with more information.
Anesthesia
You will experience pain after surgery. Be sure to ask your nurse for painkillers. You may initially receive it through an intravenous (IV) drip. Later, you may take medications by mouth (by mouth) or through a feeding tube if you have one. As you heal, you will need less pain medication.
Drainage tubes
If lymph nodes in the neck are removed, drainage tubes will be placed in the neck. You may also have them installed in the area of the free flap, if one was used. Drainage tubes are usually removed when the amount of discharge decreases. Most likely, all of these tubes will be removed before you are discharged from the hospital. If you are discharged from the hospital with tubes in place, your nurse will teach you how to care for them. For more information, read the pre-surgery guide About Neck Dissection Surgery.
Oral hygiene
Your nurse will teach you how to use the oral irrigation and care kit. This kit will help keep your mouth clean and speed up healing. After you leave the hospital, you will need to rinse your mouth with an irrigation kit. It is especially important to rinse your mouth after eating. After you eat, there should be no food particles left in your mouth. For more information, see Oral Irrigation
How to prevent spasms of the masticatory muscles
Spasm of the masticatory muscles is the inability to open the mouth. During recovery after surgery, it is very important to prevent spasm of the masticatory muscles. Your nurse will teach you exercises to help prevent this side effect, which are described in How to Prevent Masseter Muscle Spasms.
to come back to the beginning
Discharge after surgery
Your surgeon will tell you when you can return to work and normal activities. It depends on the surgery you underwent and the speed of recovery.
In most cases, patients can cope with daily activities at home without additional help, but the nurse will discuss this with you before leaving the hospital. If you need help, your nurse or case manager can help arrange visits from a visiting nurse or home health professional.
Call your healthcare provider if you have any of these signs or symptoms of infection:
- temperature 101°F (38.3°C) or higher;
- increased redness around the incisions;
- increased discharge from the incisions;
- discharge that has an unpleasant odor;
- increased pain that does not go away after taking a prescribed pain reliever or acetaminophen (Tylenol®).
to come back to the beginning
Forecast
The prognosis for RPR depends on the stage and location of the tumor. In most cases, the stage of the tumor is related to the time of diagnosis. The earlier the diagnosis is made, the lower the stage of the tumor, and, therefore, the better the survival rate.
Other factors must also be taken into account, such as the location of the tumor, the patient's general health, age, tobacco use, and the presence of human papillomavirus (HPV).
Based on 2022 EU data, the overall estimated 5-year survival rate for RCC is approximately 66%.
Lip carcinomas generally have the best 5-year survival rate (88%), while floor of the mouth cancers have the worst (54%).
Tumor staging has been shown to be the best prognostic factor for lip carcinoma, whereas transcriptionally active HPV status is considered an important prognostic factor for RCC.
Those with HPV-positive tumors tend to respond better to chemotherapy or radiation therapy compared to those with HPV-negative tumors.
According to the US National Cancer Institute, the five-year survival rates for RCC are as follows:
- 83%, for localized cancer (that has not spread);
- 64%, for cancer that has spread to nearby lymph nodes;
- 38%, for cancer that has spread to other parts of the body.
Follow-up
You will need to see your head and neck surgeon 7-10 days after discharge. If a plastic surgeon was involved in the operation, you will also need to see this specialist. Call each doctor's office to make an appointment. Depending on the rate of healing, you may have some stitches removed at your first follow-up appointment. You will also have a complete examination of your head and neck.
If your lab results are ready, your head and neck surgeon will review the results with you during your first follow-up appointment. He will also give you details about the cancerous tumor that was removed during surgery.
Your healthcare provider will discuss the need for additional treatment with you. In most cases, patients with advanced oral cancer need to undergo radiation therapy, chemotherapy, or both after surgery to ensure that all cancer cells are removed. If you would like to have these procedures done at Memorial Sloan Kettering (MSK), an appointment will be made for you. If you would like to take them elsewhere, we can help you choose a healthcare professional. Your medical record will be sent to the health care provider who will treat you.
It is very important not to miss any follow-up appointments. These techniques can help detect relapse (recurrence of cancer) or new cancers at an early stage. As time goes on, visits will be scheduled less frequently.
to come back to the beginning
Classification of oncological pathology of the palate
In half of all cases, malignant tumor of the hard palate is squamous cell carcinoma.
Nonsquamous cells, including minor salivary gland cancer, sarcoma, and melanoma, account for the other half of hard palate neoplasms. In 80% of cases, a tumor of the soft palate is squamous cell carcinoma. The remaining 20% are benign neoplasms.
The histological distribution of malignant neoplasms of the hard palate is as follows:
- squamous cell carcinoma - 53%;
- adenoid cystic carcinoma - 15%;
- mucoepidermoid carcinoma - 10%;
- adenocarcinoma - 4%;
- anaplastic carcinoma - 4%;
- other - 14%.
The histological types and frequency of neoplasms of the minor salivary glands of the palate are as follows:
- Benign - 26%
- Malignant - 74% overall Adenoid cystic carcinoma - 30%
- Mucoepidermoid carcinoma - 16%
- Adenocarcinoma - 18%
- Malignant mixed tumor - 8%
- Other - 2%
Recovery
Being diagnosed and treated for cancer can leave you feeling stressed and overwhelmed. Each person deals with this differently. Many people say that it is helpful to focus on small improvements that you will see with each new day and each new week, for example:
- swelling will gradually subside;
- the face will begin to look more natural, and the scars will become less noticeable;
- It will become easier for you to speak and you will be able to eat many of your favorite foods; A dietitian can help you choose the best way to prepare your favorite foods until your ability to chew and swallow is restored;
- you'll have more energy to do the things you love.
Support Resources
Numerous resources are available to help you and your loved ones through the recovery process. Some of them are offered by MSK, while others can be found locally. Ask your health care provider or social worker about available resources.
You may find it helpful to talk to a head and neck cancer survivor or someone who has cared for someone who has undergone similar treatment. Through our Patient and Caregiver Support Program, you can connect with former patients and caregivers. To learn more about this program, call 212-639-5007.
MSK's Resources for Life After Cancer (RLAC) Program provides support and education for patients who have completed treatment. For more information about this group and the programs offered, call 646-888-8106 or visit our Cancer Survivor Program page at
Emotional Health
It is normal if you feel depressed during or after treatment. Programs are available to help you cope with these feelings. It is important to recognize the signs of depression, such as:
- feelings of helplessness and sadness;
- inability to concentrate or do usual activities;
- mood swings;
- changes in sleep patterns (increasing or decreasing usual sleep duration);
- increase or loss of appetite.
Call your healthcare provider if you have these symptoms and they do not go away for more than 2 weeks. To speak with a counselor, call the MSK Counseling Center at 646-888-0200. For more information, see Coping with Depression During Cancer Treatment.
Smoking and drinking alcohol
Using tobacco or alcohol increases your risk of developing oral cancer. Quitting these bad habits will help reduce the risk of recurrence or formation of a new tumor. If you want to quit smoking, we can refer you to a Tobacco Treatment Program at our center or in your community. For more information, contact MSK's Tobacco Treatment Program at 212-610-0507 or visit: . Tips on how to quit smoking are given in our material Recommendations for the treatment of tobacco addiction for patients and their family members.
If you want to stop drinking alcohol, there are programs that can help you.
For more information, call MSK's Counseling Center at 646-888-0200. to come back to the beginning