Palate cancer is a malignant neoplasm that forms from the mucous membrane of the hard and soft palate. This is a fairly rare disease. It is more common between the ages of 40 and 60 years. Men get sick 4 times more often than women.
Diagnosis of cancer of the soft and hard palate at the Yusupov Hospital is carried out using modern research methods. The oncology clinic is equipped with modern equipment from leading American and European manufacturers, which allows you to quickly establish an accurate diagnosis. To treat malignant tumors of the palate, surgical interventions, chemotherapy drugs and innovative methods of radiation therapy are used.
The most malignant tumor of the palate occurs due to metastases of cancer of the nasopharynx and nose. The neoplasm affects the periosteum of the hard palate, lower and upper jaws, muscles and tissue of the oral cavity, and tongue. Atypical cells spread to the submandibular, mental and cervical lymph nodes.
Classification of oncological pathology of the palate
In half of all cases, malignant tumor of the hard palate is squamous cell carcinoma.
Nonsquamous cells, including minor salivary gland cancer, sarcoma, and melanoma, account for the other half of hard palate neoplasms. In 80% of cases, a tumor of the soft palate is squamous cell carcinoma. The remaining 20% are benign neoplasms.
The histological distribution of malignant neoplasms of the hard palate is as follows:
- squamous cell carcinoma - 53%;
- adenoid cystic carcinoma - 15%;
- mucoepidermoid carcinoma - 10%;
- adenocarcinoma - 4%;
- anaplastic carcinoma - 4%;
- other - 14%.
The histological types and frequency of neoplasms of the minor salivary glands of the palate are as follows:
- Benign - 26%
- Malignant - 74% overall Adenoid cystic carcinoma - 30%
- Mucoepidermoid carcinoma - 16%
- Adenocarcinoma - 18%
- Malignant mixed tumor - 8%
- Other - 2%
Causes of palate cancer
The causes of this disease have not been established, but it is known that certain factors may increase the risk of developing malignant tumors of the palate.
Smoking and chewing tobacco
Active smoking, especially unfiltered cigarettes and cigars, at least doubles the risk of developing malignant neoplasia of the oral cavity. Their development is also facilitated by the use of chewing tobacco mixtures - betel nut, gutka, snus, etc.
Alcohol
Strong alcohol is a recognized risk factor for palate cancer. This is mainly associated with the direct damaging effect of ethyl alcohol on the oral mucosa.
Human papillomavirus
HPV infection has been significantly associated with an increased risk of developing oral squamous cell carcinoma in recent studies.
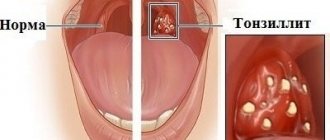
Chronic inflammatory diseases of the oral cavity
Sluggish inflammatory processes, such as chronic gingivitis or periostitis, increase the likelihood of the formation of palate tumors.
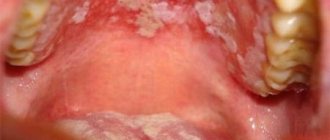
Precancerous diseases
In the presence of pathologies of the mucous membrane such as leukoplakia or erythroplakia, the likelihood of developing cancer becomes extremely high - up to 90%.
Gels and ointments for treating inflamed mucous membranes
External agents, which include gels and ointments, are also prescribed to relieve pain and acute signs of inflammation. Below, as an example, are the most effective and popular drugs from this pharmacological group:
- “Nystatin” ointment - it is prescribed for candidiasis. The active ingredients in the composition destroy fungal cells and create a reliable barrier that prevents the further spread of infection,
- "Levomekol" ointment - has an antibacterial effect and promotes tissue regeneration processes. The active components of the product help reduce inflammation and actively fight the population of harmful microorganisms,
- “Solcoseryl” – this product contains an extract of calf’s blood (dialysate), which has a powerful therapeutic effect. The gel restores oxygen metabolism, triggers tissue regeneration processes at the cellular level and promotes collagen production, thereby accelerating damage processes,
- "Cholisal" is an anesthetic gel with a slight cooling effect. Helps relieve swelling and inflammation, destroys pathogenic microflora.
Gels and ointments are prescribed to relieve pain and acute signs of inflammation.
The choice of a suitable remedy remains at the discretion of the attending physician and directly depends on the cause of the development of the inflammatory process in the palate. Before use, you should carefully read the instructions and then follow all the instructions of the treating specialist.
Symptoms of the disease
Squamous cell carcinoma appears as ulcerative superficial lesions. However, there are often no signs of palate cancer in the initial stages. The first manifestations appear, as a rule, already in the advanced stages of the disease.
Palate cancer - symptoms and first signs:
- bleeding;
- difficulty swallowing;
- speech disorders;
- bad breath;
- wounds in the mouth that do not heal for a long time;
- loosening of the teeth of the upper jaw;
- pain when swallowing;
- weight loss;
- ear pain;
- swelling of the neck;
- white spots in the mouth that do not disappear for a long time.
A swelling on the roof of the mouth, bleeding, foul odor, or loose teeth may be symptoms in patients with hard palate cancer. Patients with advanced soft palate cancer may have difficulty swallowing, altered speech, trismus, or neck swelling.
Because the area is easily visualized, tumors are often discovered in the early stages by chance by the patient or physician.
What is the palate and where is it located in the oral cavity?
As mentioned above, this is a horizontally located partition that separates the oral cavity from the nasal cavity. Approximately 2/3 of its surface suggests the presence of a bone base. These are solid processes in the form of plates that have a concave shape and are located in a horizontal position on the upper jaw. They are covered by a thin mucous membrane, which turns into the velum palatine. This is already a muscular formation with a fibrous membrane, also covered with mucous membrane.
The upper palate is the wall located in the mouth from above in the horizontal plane
It is the soft part that represents the barrier between the mouth and pharynx, and on its far edge there is the uvula. The palate is directly involved in the process of chewing food and swallowing, helps in the reproduction of sounds, which makes it an important component of the articulatory apparatus.
Stages of development of palate cancer
The stages of malignant neoplasms of the palate are determined based on the international TNM system. With its help, the characteristics of the tumor are described according to three main criteria.
Primary tumor stage (T)
- TX—primary tumor not evaluable
- T0 - no evidence of a primary tumor (T - carcinoma in situ.)
- T1—tumor 2 cm or less in greatest dimension
- T2 - tumor larger than 2 cm but not larger than 4 cm in greatest dimension
- T3 - tumor larger than 4 cm in greatest dimension
- T4 - Tumor invades adjacent structures (eg, cortical bone, soft tissue of the neck, maxillary sinuses)
Regional lymph node involvement (N)
- NX—regional lymph nodes not evaluable
- N0 - Absence of regional metastasis in the lymph node
- N1 - Metastasis in one ipsilateral lymph node, 3 cm or less in greatest dimension
- N2 - metastasis in one ipsilateral lymph node, more than 3 cm, but not more than 6 cm in greatest dimension; in several ipsilateral lymph nodes, not more than 6 cm in greatest dimension; or in bilateral or contralateral lymph nodes, not more than 6 cm in greatest dimension
- N3 - Metastasis in a lymph node greater than 6 cm in greatest dimension
Distant metastasis (M)
- MX - The presence of distant metastases cannot be assessed
- M0 - no distant metastases
- M1 - distant metastases
Based on the TNM characteristics, the so-called clinical stage is determined.
| Stage | Characteristics |
| 0 | Tis N0 M0 |
| I | T1 N0 M0 |
| II | T2 N0 M0 |
| III | T3 N0 M0 |
| (T1, T2, T3) N1 M0 | |
| IVA | T4a ( N0 or N1) M0 |
| (T1, T2, T3 or T4a) N2 M0 | |
| IVB | Any T N3 M0 |
| T4b Any N M0 | |
| IVC | Any T Any N M1 |
What does traditional medicine offer?
Some remedies prepared from herbal ingredients based on folk recipes also help relieve inflammation and reduce pain in the palate. Tannins and astringents in their composition have a disinfectant and analgesic effect. The most popular and proven recipes are described below, but it is better to first discuss their use with your doctor.
Calendula tincture
Used for pharyngitis, laryngitis, tonsillitis and fungal infections in the oral cavity. To prepare the tincture, you can dissolve a teaspoon of the product in 200 ml of warm water. Or pour raw calendula flowers with a tablespoon of boiling water, strain and use for rinsing while warm.
Calendula tincture will relieve pain
Chamomile decoction
Soothes, relieves acute inflammation, helps with colds and fungal infections. A tablespoon of dried flowers is brewed in 200 ml of boiling water, allowed to cool, filtered and used for rinsing 3-4 times a day.
Chamomile decoction helps well in treatment
Sage based rinse solution
Recommended for laryngitis, as well as for scratches on the palate, pharynx or larynx. The solution perfectly relieves inflammation and relieves pain. Sage leaves and flowers (1-2 tablespoons) are brewed in 200 ml of boiled water. The product is infused until it cools completely, then filtered and then used for rinsing up to 6-7 times a day.
Oak bark decoction
Effectively relieves bleeding and inflammation, eliminates swelling. To prepare the solution, 2 tablespoons of crushed oak bark are diluted in 200 ml of water and heated in a water bath for 15-20 minutes. Remove, leave to brew for an hour, filter and then use for rinsing 4-5 times a day.
Gargling with a decoction of oak bark will help in treatment
Honey with tea or milk
Honey has an enveloping and soothing effect and effectively fights the proliferation of fungi and the spread of infection. To enhance the healing effects, it is recommended to eat honey with a warm drink or dilute it in tea.
You can relieve pain in the palate and reduce inflammation with the help of a medicinal mixture, for the preparation of which butter and honey should be mixed in equal proportions. The composition must cool completely, after which it can be taken 0.5-1 teaspoon 5-7 times a day.
Tea with honey is used to treat throat
Diagnosis of palate oncology
In most cases, detection of oncological pathologies of the palate occurs during a routine examination by a dentist. The diagnosis is then confirmed by biopsy findings.
However, to assess the extent of the tumor in the structures of the upper jaw, pharynx, etc. Additional diagnostic tools are required:
- MRI (magnetic resonance imaging) - to detect tumor growth in the sinuses of the upper jaw or the nasal cavity.
- PET (positron emission tomography) - to detect metastasis in regional lymph nodes and separated metastasis.
Probability of disease recurrence
After intensive therapy, the patient is discharged home. He must be observed by an oncologist on an outpatient basis for a year. It is recommended to visit a doctor for a preventive examination every three months. This will allow you to recognize the symptoms of relapse in time and carry out treatment again.
In case of relapse, a cancerous tumor arises either in the same place or in other organs. Distant metastases are difficult to diagnose if the cancer cells are dormant in the organ they entered through the blood or lymphatic system. The period of remission in this case can be long.
Treatment of the disease
Radiation therapy
Radiation therapy to treat palate cancer can be used in several ways.
- As the primary treatment for small, early-stage tumors.
- As an adjunct to surgery or ongoing chemotherapy. In this case, it is possible to use adjuvant radiation therapy as after surgery to destroy tumor remnants. So is the use of radiation before surgery to shrink the tumor and make it easier to remove—neoadjuvant radiation therapy.
- Radiation therapy can also be used to relieve symptoms of advanced, inoperable cancer, such as pain, bleeding, problems swallowing, and problems caused by bone metastases.
Modern radiotherapy for palate cancer in Belgium
Radiation in cancer centers in Belgium is carried out using techniques that help doctors focus the radiation more precisely.
There are two main such methods.
- Three-dimensional conformal radiation therapy (3D-CRT);
- Intensity modulated radiation therapy (IMRT).
These methods rely on the results of imaging tests, such as MRI, and special computer programs to pinpoint the location of the tumor. The beams are then shaped and directed at the tumor from multiple directions, reducing damage to healthy nearby tissue.
Another modern way of delivering radiation is to place radioactive materials directly into the tumor. This is called brachytherapy.
To do this, a small grain of radioactive material is placed into the tumor. In this case, the radiation spreads only over a very short distance and is limited to the tumor.
Surgery
The type of operation is selected depending on the location and extent of the tumor.
For small to medium-sized tumors up to T3, an oral approach is often used without trauma to the mandible. For most tumors that do not have regional spread, surgery to remove the hard or soft palate is used - palatectomy.
For tumors that have grown into the paranasal sinuses or nasal cavity, a unilateral or bilateral maxillectomy (removal of the upper jaw) may be required.
Chemotherapy
Treatment of palate cancer with chemotherapy is considered as an additional method in combination with radiation therapy and surgery.
The chemotherapy drugs most often used for cancer of the oral cavity and oropharynx are:
- Cisplatin;
- Carboplatin;
- 5-fluorouracil (5-FU);
- Paclitaxel (Taxol);
- Docetaxel (Taxotere).
Targeted and immunotherapy
As a rule, targeted and immunological drugs for this disease are used for metastatic inoperable forms, or for relapses.
Cetuximab (Erbitux®) is a monoclonal antibody that targets the epidermal growth factor receptor (EGFR), which helps cells grow and divide. Palate cancer cells often have higher than normal amounts of EGFR. By blocking EGFR, cetuximab can help slow or stop cell growth.
Pembrolizumab (Keytruda®) and nivolumab (Opdivo®) are drugs that target the PD-1 checkpoint. It is a protein on the membranes of T cells that normally helps keep these cells from attacking other cells in the body.
By blocking PD-1, these drugs boost the immune response against cancer cells, which can shrink some tumors or slow their growth.
A Brief Overview of Mouthwashes
Pharmacy rinses help relieve acute signs of inflammation, relieve pain and reduce swelling. Among the most effective drugs in this category, experts identify the following medications:
- Chlorhexidine is an inexpensive antimicrobial agent that helps to significantly reduce inflammation and stop the spread of infection. It is recommended to use for rinsing no more than 3 times a day,
- “Stomatofit” is a herbal remedy that helps with gingivitis and periodontitis,
- "Furacilin" - prescribed for inflammatory processes in the throat, palate and oral cavity. Has a pronounced antimicrobial effect and ensures the destruction of pathogenic microflora,
- “Chlorophyllipt” - a composition based on eucalyptus helps to soothe an irritated throat and palate during colds.
Pharmacy rinses help relieve acute signs of inflammation
“For some reason, my palate gets irritated about once every six months. I don't know, maybe it's too sensitive. And it happens that the pain is simply unbearable, you have to swallow painkillers. But in such cases, I usually rinse my mouth with chlorhexidine and after a week everything goes away completely.”
MariaS., from correspondence on the forum www.32top.ru
You should start using any of the drugs described above only after consulting a specialist. First, you should visit your dentist and determine the exact cause of the inflammation.
Rehabilitation after treatment
Treatment of malignant tumors of the palate is always very traumatic. The consequence of the operation is, at a minimum, a violation of the process of swallowing and speech. In multidisciplinary clinics in Belgium, rehabilitation doctors and speech therapists begin working with the patient immediately after the operation - this greatly shortens the rehabilitation period and increases its effectiveness
Reconstructive surgery - palate surgery in Belgium
Palatectomy and maxillectomy operations require subsequent prosthetics.
Small defects of the hard palate can be covered with local flaps from the rest of the hard palate or from the buccal mucosa. Larger defects are adequately and effectively treated with obturators. Because the hard palate is not dynamic, obturators are very effective and well tolerated.
The soft palate is a dynamic structure and its optimal functioning requires muscular action to lift and contract the palate during swallowing and relax it during nasal breathing. Therefore, any reconstruction of the soft palate using flaps and prosthetics does not reproduce its functionality - it will be limited even with the most successful outcome.
Complications
Complications of surgical resection of the soft palate may include:
- velopharyngeal insufficiency (most often);
- hypernasal speech;
- dysphagia (impaired swallowing);
- effusion in the middle ear due to scarring at the opening of the eustachian tube.
The extent and likelihood of these complications depend on the extent of the resection, the size of the defect, and the method of reconstruction. The larger the resection and defect, the greater the likelihood of these complications occurring.
With soft tissue resection preserving only the bony palate and soft palate, the resulting defect heals with granulation and epithelialization, and no complications are expected. If patients have previously had radiation therapy in this area, healing may be delayed.
Palate cancer and its treatment can sometimes cause problems such as loss or changes in taste, dry mouth, or even tooth loss. This can make it difficult to eat, leading to weight loss and weakness due to poor nutrition.
Radiation therapy may also cause long-term or permanent side effects.
- Damage to the salivary glands. It may cause dry mouth. This leads to problems with eating and swallowing. Lack of saliva can also lead to tooth decay (cavities).
- Damage to the jaw bone. This problem, known as osteoradionecrosis of the jaw, can be a serious side effect of radiation therapy. This condition is difficult to treat. Osteoradionecrosis is manifested by pain in the jaw, and sometimes by fractures, which require surgical treatment.
Newer radiation treatments such as IMRT may help reduce this side effect. The drug amifostine (Ethyol®) may also help reduce this side effect by limiting radiation damage to normal tissue. It is injected into a vein over 15 minutes before each radiation treatment.
Angioma
It is a benign formation, which in most cases is a congenital pathology in children. It consists of blood vessels and is dark red in color. Sometimes it looks like a small ball on a leg. Lymphangioma, formed from lymphatic vessels, most often appears on the soft palate. It looks like a small bump with a bubbly surface. First, the tumor grows inside, then a swelling appears that hurts.
The choice of treatment method depends on the type of vessels. The angioma is removed or reduced by sclerotherapy, alcohol injection, or radiation therapy. If there is a risk of severe swelling, the formation is excised with a scalpel. The ball-shaped angioma is removed using a galvanoacoustic loop.
Prevention
Limit smoking and alcohol
Tobacco and alcohol are the most important risk factors for these cancers. Not starting to smoke is the best way to limit your risk of cancer. Quitting tobacco also significantly reduces the risk of developing these cancers, even after years of use. The same applies to alcohol - limiting its amount helps reduce the risk of developing palate cancer.
Preventing HPV infection
Vaccination against HPV reduces the risk of mouth and throat cancer. But vaccines are only effective if they are given before someone gets HPV, given at a young age, before they become sexually active.
Correctly selected dentures and proper oral hygiene
Avoiding sources of oral irritation (such as dentures that don't fit properly) can help reduce your risk of developing oral cancer.