Abscess on the tongue - what is dangerous about an abscess in the mouth and how to remove it without consequences
Tongue abscess is a serious pathological condition, which is characterized by the appearance of a purulent neoplasm against the background of rapid spread of inflammation. In this case, the patient begins to experience severe malaise, the body temperature may rise sharply, and the organ itself will become swollen, which will result in problems with diction, eating, and even breathing. As part of the diagnosis, the doctor may suggest performing a puncture to find out more about the contents of the abscess. Today we’ll talk about the reasons why a purulent process can begin to develop, what accompanying symptoms are characteristic of this condition, and what methods of treating an abscess are used today.
Symptoms
The main symptoms of this disease are:
- An increase in acute, throbbing or aching toothache, intensifying with food intake;
- Experiencing a bitter taste or unpleasant odor in the mouth;
- Feeling of general weakness, headache, apathy, insomnia, lack of appetite;
- Increased tooth sensitivity;
- The gums become inflamed, there is swelling, redness, a small compaction or swelling filled with pus is formed;
- There is an enlargement of the cervical lymph nodes;
- As the infection develops, nausea appears and body temperature rises;
- Facial asymmetry may appear, the size of one cheek, lower or upper lip may increase.
It is important to know that an abscess that begins on one tooth, if left untreated, can spread to the next. If the outer shell cannot withstand and ruptures, the pus comes out, it becomes easier and the pain goes away, but there is a risk of purulent masses getting into healthy tissues and teeth, and the sad story repeating. Ignoring purulent seals in the oral cavity can lead to such dire consequences: tooth loss, death of jaw tissue, development of respiratory diseases (pneumonia, sore throat) and vision. This is also fraught with paralysis of the facial nerves, and the entire body is exposed to acute intoxication.
Features of a purulent abscess
An abscess on the oral mucosa is a kind of abscess, which is characterized by severe inflammation and the formation of purulent masses. Gradually, it leads to the death of living tissue, and in an advanced stage it is accompanied by a general deterioration in the patient’s condition and the appearance of severe pain during talking, chewing food and even breathing. Obviously, this pathology can provoke very serious consequences for the body as a whole, so under no circumstances should an abscess in the oral cavity be ignored.
The photo shows a tongue abscess
An abscess of the root of the tongue, as, in fact, of any other part of this organ, is quite readily treatable, but requires an integrated approach to solving the problem. It is important to understand here that the sooner inflammation is detected, the easier and faster it can be eliminated. The pathology in question has a serious impact on the overall health and immunity, so do not hesitate with treatment.
Abscesses and phlegmons of the tongue
Purulent processes of the tongue can occur both in the own muscles of the moving part of the tongue and in the cellular spaces of its root. Abscesses of the mobile part of the tongue most often occur as a result of infection of wounds, as well as when foreign bodies of a food nature, most often fish bones, are introduced into the tongue. The patient complains of sharp pain when swallowing and moving the tongue. When palpating the tongue, there is a painful infiltrate, which is located more often on the lateral surface, less often on the dorsal surface. Fluctuation is usually not determined due to the localization of the purulent focus in the muscle layers. The opening of abscesses of the movable part of the tongue is carried out with longitudinal incisions at the site of the greatest protrusion.
The boundaries of the root of the tongue are: above - the own muscles of the tongue; below - mylohyoid muscle; outside - the genioglossus and hyoglossus muscles of the right and left sides. On the pharyngeal surface of the root of the tongue there is a lingual tonsil, which is part of the lymphoid ring of the Pirogov-Waldeyer pharynx (palatine, tubal, pharyngeal and lingual tonsils).
The main source of infection can be infected wounds of the tongue. The purulent-inflammatory process that develops in the area of the root of the tongue can spread from the lingual tonsil, from the sublingual, submental and submandibular tissue spaces. Less commonly, the source of infection is foci of odontogenic infection located in the area of the large molars of the lower jaw. We should not forget about suppuration of congenital cysts of the tongue.
Clinic. With abscesses and phlegmon of the root of the tongue, patients complain of severe pain in the area of its root, which radiates to the ear. Swallowing saliva and liquid is extremely painful and sometimes even impossible. When you try to take a sip, the liquid enters the respiratory tract and causes a painful cough. As a rule, due to swelling of the epiglottis, breathing problems occur; sometimes, as a result of eustachitis, hearing decreases.
The clinical course of phlegmon of the root of the tongue is severe . The tongue is sharply enlarged in size, does not fit in the oral cavity, and its mobility is sharply limited. The mouth is slightly open, thick saliva is released from the mouth, often with an unpleasant odor. Palpation reveals uniform swelling and density of the tongue; pressing on its back (along the midline) causes sharp pain.
pain. The mucous membrane of the tongue is hyperemic and cyanotic. Fluctuation is usually not determined, since the purulent focus is located between the muscles. The back of the tongue is covered with a dry purulent coating. The infiltrate can be felt in the depths of the submental region above the hyoid bone.
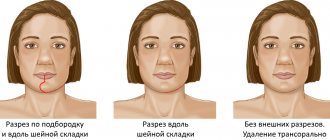
Treatment. Surgical access for purulent-inflammatory processes of the root of the tongue, extraoral. A 4 cm long incision is made from the side of the skin along the midline or in the submental area. Spreading the edges of the wound with hooks, the mylohyoid muscles are cut along the seam. They stupidly push apart the soft tissues and penetrate to the purulent focus. Drainage of the latter is carried out with active double tubular drainage. Sometimes, with increasing hypoxia, there is a need to form a tracheostomy.
Operative access to a purulent focus can be either intraoral or extraoral. The incision is made from the side of the oral cavity, parallel to the inner surface of the lower jaw. Its length should be 3 cm. Only the mucous membrane of the floor of the mouth is cut with a scalpel, and it is penetrated deeper in a blunt way to avoid damage to the lingual artery. They penetrate the purulent focus, bluntly exfoliating the underlying soft tissue. In case of a diffuse purulent-inflammatory process, an incision is made in the submandibular region with dissection of part of the fibers of the mylohyoid muscle, and drainage of the purulent wound is carried out with active double tubular drainage.
The peripharyngeal space (spatium parapharyngeum) is an almost isolated space (Fig.), limited on the inside by the lateral wall of the pharynx, in front by the ascending part of the mandible and the internal pterygoid muscle, behind by the prevertebral fascia, outside by the deep layer of the parotid fascia.
Along this space runs the internal carotid artery (a. carotis int.), the hypoglossal, vagus, glossopharyngeal, accessory nerves (nn. hypoglossus, vagus, glossopharyngeus, accessorius), to which the internal jugular vein (v. jugularis) adjoins on the inside int.). Through a hole in the deep layer of the fascia of the parotid gland, the peripharyngeal space communicates with the internal part of the bed of this gland. The peripharyngeal space is connected with the retropharyngeal space (see). Downwards, the O. p. passes into the median fissure of the neck, located under the body of the hyoid bone between the middle and superficial fascia of the neck on one side and the deep fascia of the neck on the other. At the upper aperture of the chest, the median fissure of the neck passes into the mediastinum.
Acute inflammatory processes in the peripharyngeal space often occur as an abscess or phlegmon. They can arise as a result of penetration of a virulent infection by tonsillogenic, odontogenic, otogenic and from the parotid gland.
With the development of a peripharyngeal abscess, the patient’s general condition suffers sharply: high temperature, sometimes chills, leukocytosis increases and ROE accelerates. As a result of the inflammatory process in the internal pterygoid muscle, prolonged trismus of the lower jaw can develop. When examining the pharynx, enlargement and protrusion of the tonsil or areas of the lateral wall of the pharynx and swelling of the soft palate are visible. Along with the enlargement and pain of the regional lymph nodes, a diffuse, very dense and painful swelling appears in the area of the angle of the lower jaw and along its edge, sometimes spreading to the parotid gland. With an odontogenic peripharyngeal abscess, inflammatory changes in the area of the posterior sections of the alveolar processes of the lower jaw come first.
Treatment is surgical with the simultaneous use of antibiotics and sulfonamides. First of all, it is necessary to eliminate the focus (tonsillectomy for peritonsillar abscess, tooth extraction, trepanation of the mastoid process, etc.), and then open the peripharyngeal abscess. When the patient’s condition is very serious, sometimes it is necessary to first open the abscess. In more complex cases, a peripharyngeal abscess or phlegmon is opened through the neck. To do this, an incision is made along the anterior edge of the sternocleidomastial muscle along its upper third, starting 1 cm above the angle of the lower jaw. The digastric and stylohyoid muscles running together are looked for; the latter are pulled downwards. Using a blunt instrument, or preferably an index finger, they penetrate above these muscles into the loose tissue of the anterior part of the peripharyngeal space, keeping the direction upward and somewhat anteriorly, open the abscess and then pack the wound or insert rubber drainage into it; several close sutures are applied.
Phlegmon of the floor of the mouth is understood as diffuse purulent inflammation of the tissues located above and below the so-called muscular diaphragm of the floor of the mouth. Essentially it is a phlegmon of the sublingual and submandibular areas^
Reasons for the formation of an abscess on the tongue
Most often, the formation of a purulent focus on the body and the root of the tongue in particular becomes a consequence of mechanical or thermal effects. Damage opens a direct path for the penetration and spread of bacterial infection. As practice shows, the formation of an abscess is often preceded by injury to the mucous membrane with sharp fish bones.
“In my case, the abscess was generally the result of my passion for dried vobla! Once again I accidentally scratched the edges of my tongue, then it turned red, began to hurt, and one fine morning I discovered a small abscess on it. I was scared, of course, and immediately made an appointment with a doctor. Fortunately, everything worked out without surgical intervention. The doctor prescribed rinsing with chlorhexidine.”
Anna Semenova, 43 years old, Omsk, from correspondence on the forum www.32top.ru
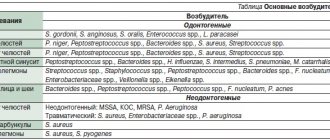
Quite often, the oral mucosa is injured by sharp edges of teeth or crowns, as well as worn-out prosthetic structures and incorrectly adjusted orthodontic devices for correcting the bite. Patients suffering from periodontitis, ulcerative stomatitis, and acute tonsillitis are also at risk. In this case, pathogenic bacteria can spread from the source of chronic infection in the oral cavity. Thus, to date, experts in the field of dentistry have identified the following main reasons for the development of pathology:
- penetration of infection, staphylococci and streptococci,
- trauma to the mucous membrane,
- imbalance of oral microflora,
- dental diseases,
- glossitis,
- stomatitis,
- tonsillitis.
Trauma to the tongue can cause an abscess.
It should also be noted that quite often an abscess develops after a burn as a result of consuming too hot food or drinks. Infection can also appear through fresh scratches from hard foods or sores caused by eating spicy or salty foods.
Characteristic symptoms
The pathology is characterized by a fairly rapid pace of development. Based on where exactly the neoplasm is localized, experts distinguish between deep and superficial forms of abscess. Let's look at each of them in more detail.
Surface view
In this case, an abscess occurs on the back of the organ. The person experiences acute pain during swallowing, which often radiates to the ear. As part of a visual examination, noticeable swelling of the mucous membrane can be detected; when touched, a compaction can be clearly felt. Such an abscess can open without outside help, but in any case professional treatment is necessary.
Deep view
This is a more dangerous form of pathology, in which purulent processes develop in the thickness of the tissues of the organ. Experts include the following conditions as associated symptoms:
- general weakness,
- poor appetite
- restless sleep due to constant painful sensations,
- tachycardia,
- heat,
- enlarged lymph nodes,
- increased salivation,
- severe swelling of the organ, acute pain,
- blue mucous membranes, formation of gray plaque,
- the appearance of bad breath.
The main danger is that when an abscess develops, the tongue greatly increases in size. As a result, problems arise not only with speech, but also with breathing.
How is diagnostics carried out?
At the first appointment, the doctor is obliged to ask the patient about all the symptoms that worry him. He also needs to find out the circumstances under which the mucous membrane was injured. Next, the specialist sends the patient for blood tests, since the formation of an abscess usually causes a significant increase in the level of leukocytes and ESR.
For diagnosis, a blood test is required.
In order to identify the pathogen, bacterial culture is performed. The patient may also be referred for an X-ray examination, which will help detect the source of the infection, especially if there are complications. Competent diagnosis makes it possible to distinguish between diseases such as tongue abscess and Ludwig's tonsillitis, lymph node abscess, lymphadenitis.
Possible complications
The pathological condition under consideration, especially if the formation of an abscess occurs at the very root of the organ, is fraught with serious consequences for the entire organism as a whole. If treatment is not started in time, the abscess may well result in serious complications. Thus, in advanced stages it is often accompanied by purulent inflammation of the tissue - the formation of phlegmon, the occurrence of sepsis and severe intoxication of the body, and this, in turn, can lead to death.
Treatment of tongue abscess
Conservative therapy involves taking antibiotics and rinsing with antiseptic agents, such as Furacilin or Chlorhexidine. However, such treatment can be effective only at the earliest stage of pathology development. If the situation is advanced, immediate surgical intervention will most likely be required. The dentist will perform an emergency opening of the abscess, thereby preventing further spread of the infection. If a purulent neoplasm has formed deep at the base of the organ, the doctor may perform an autopsy from the outside under the chin. After removing purulent discharge, the specialist will thoroughly rinse the cavity using antibiotics and proteolytic enzymes1.
In some cases, surgery is performed to remove the pus.
In the most advanced cases, when the patient is already experiencing serious breathing difficulties, a tracheotomy is performed. The patient is prescribed antibiotics, anti-inflammatory drugs and antihistamines. To strengthen the body's defenses, it is recommended to take multivitamin complexes and regularly rinse the mouth with antiseptics, including decoctions of medicinal herbs - chamomile and sage. It is important to understand here that the use of any pharmaceutical drugs and traditional medicine must be agreed upon with the attending physician.
Treatment
To get a complete picture of the disease, dentists use modern diagnostic methods, on the basis of which they select the optimal solution to this problem. These include radiography, ultrasound, sampling of purulent mass and their analysis, visual examination of the condition of the pharynx (pharyngoscopy). Based on the results obtained and studying the history of the disease, appropriate therapy will be prescribed.
Before visiting a doctor, you can alleviate your condition a little by taking painkillers and warm antiseptic solutions, but you should not put off visiting the dentist for long, because the process develops very quickly and does not go away on its own.
Treatment of an oral abscess is usually carried out using two methods:
- Surgical intervention Allows you to avoid most of the complications that may arise from an unauthorized breakthrough of a purulent sac. The operation is performed under local anesthesia by a dental surgeon, with the help of special instruments the abscess is opened, the wound is cleaned and drainage is placed, after the operation antibiotics, antihistamines, vitamins and immunomodulators are prescribed;
- Medication Medications (Fluocinonide gel, Chlorhexidine solution, Ibuprofen) are prescribed only in the initial stage; timely consultation with a doctor and timely prescribed medications help avoid surgical intervention.
When the pus comes out, relief comes: there is no more pain, the temperature returns to normal, and the swelling disappears. The course of treatment ends with the necessary physical procedures: electropharesis with the addition of an antiseptic on the gums, UHF heating, and the procedure for silvering teeth affected by caries. Until the wound in the mouth completely heals, the patient must abandon hard vegetables and fruits in favor of soft cereals and liquid soups.
Prognosis and prevention
The success of treatment largely depends on how deeply the infection has spread and how quickly the person receives medical care. If an abscess is diagnosed in a timely manner, the likelihood of a favorable outcome will be at the highest level - the disease can be cured in just a couple of weeks. If the problem is neglected, the situation may result in the development of phlegmon and sepsis. To prevent the appearance of an abscess on the tongue, including relapses, it is enough to follow the recommendations of doctors:
- pay close attention to oral hygiene, brush your teeth and tongue twice a day,
- minimize the consumption of too spicy and salty foods,
- take care of the condition of the oral cavity, try not to injure the mucous membrane with foreign objects,
- in case of accidental damage, you should thoroughly rinse your mouth with water and an antiseptic solution, and also, just in case, consult a specialist to eliminate the risk of infection of the wound,
- strengthen the immune system - a healthy lifestyle, frequent walks in the fresh air, sports and proper nutrition,
- systematically visit the dentist for preventative care.
Preventive examinations with a dentist will help you avoid problems.
If you detect any suspicious changes in the condition or appearance of the oral cavity, you should definitely consult a doctor for advice. It is better to waste your time and go to a specialist than to undergo long and grueling treatment.
Prevention
In general, the effectiveness of treatment depends on at what stage of the disease the patient sought medical help and his general health. It is very important to follow all doctor’s orders and treatment procedures immediately after they are prescribed. A timely surgical operation and the absence of complications after it are a guarantee of healing the abscess within one to two weeks.
Preventive measures to prevent this disease are very simple:
- Maintain hygiene, which includes high-quality and proper care of teeth and gums (brushing teeth and tongue at least twice a day, cleaning interdental spaces with dental floss after meals, regular use of mouth rinses);
- Treat carious teeth and other oral diseases in a timely manner;
- Protect the jaws and oral mucosa from injury;
- Have a complete diet, including vitamins and vital microelements.
Simple tips, the implementation of which depends only on your desire, will help in the future to avoid serious consequences caused by an abscess. And remember: oral health directly affects the beauty and charm of your smile.
Home remedies
To speed up the wound healing process after treatment, you can resort to proven home methods. Here it should immediately be noted that their use is justified only if the attending physician has given his consent. Here are some reliable tips:
- rinsing with a light saline solution at the rate of 2 teaspoons per glass of water at room temperature,
- treating wounds with a solution of hydrogen peroxide or Chlorhexidine,
- applying a piece of ice to relieve acute inflammation.
Tongue abscess is a disease that is inevitably accompanied by very unpleasant symptoms. A general deterioration in health, high temperature, pain, problems with speech and breathing are only a small part of what the development of such a serious and dangerous phenomenon in an advanced stage entails. To prevent the situation from worsening, consult a doctor immediately when the first signs of pathology appear.
- Vernadsky Yu.I. Fundamentals of maxillofacial surgery and surgical dentistry, 2003.
Ultrasound examination of the maxillofacial area
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
The ultrasound research method has become firmly established in general diagnostic practice; its role can hardly be overestimated. A modern approach to diagnosing diseases in the clinic of internal medicine is unthinkable without ultrasound examination of the abdominal organs (including the retroperitoneum and pelvis), thyroid gland, mammary glands, heart and blood vessels.
Compared to the above-listed areas of application of echography, ultrasound examination of the maxillofacial area is performed much less frequently. This is due, on the one hand, to the clinical isolation of dentistry and maxillofacial surgery, which does not allow general practitioners of ultrasound diagnostics to gain sufficient experience in research in this area, and on the other hand, to some conservatism of dentists and maxillofacial surgeons, who consider the main diagnostic tool for them to be X-ray examination method. Their skepticism regarding ultrasound examination is based on the fact that almost all soft tissue structures of the maxillofacial region are accessible to palpation, and the skin and mucous membranes are accessible to inspection.
However, paying tribute to the history of the development of ultrasound diagnostics, it is necessary to mention that the object of the very first (then still one-dimensional - in A-mode) echographic studies performed by a group of researchers led by D. Howry in 1955 were the parotid glands.
Ultrasound of soft tissues of the face and neck in its modern version does not require the use of any special ultrasound scanners or sensors and can be performed on equipment designed for studying peripheral structures: linear sensors with an oscillation frequency of 5.0-7.5-9 are quite sufficient .0 MHz. Transcutaneous echography is quite informative and generally satisfies the needs of clinicians: almost all parts of the face and neck (including the body and root of the tongue) are accessible to echographic examination using external sensors. Only the upper parts of the peripharyngeal space and the pterygomaxillary space, shielded by the branch of the lower jaw, are inaccessible.
There are no age restrictions or special preparation of the patient for an ultrasound examination.
For an ultrasound diagnostic physician, the maxillofacial area can be of great professional interest, since diseases of all nosological groups are found here (from inflammatory, autoimmune and degenerative-dystrophic to tumor), as well as various malformations (angiodysplasia, lymphangiomas, congenital cysts). Differential diagnostic difficulties increase due to the fact that the maxillofacial area is a zone of massive infection and the existence of primary non-inflammatory diseases is often masked by the addition of an inflammatory process with the entire spectrum (from erased to clinically pronounced) of its signs.
The complexity of the anatomical structure of the maxillofacial region creates additional difficulties for interpreting the results of ultrasound examination. At the same time, anatomical detail is of great importance, since determining the organ affiliation of the pathological process and clarifying the topographic and anatomical features of its distribution are one of the most important diagnostic tasks, along with identifying the nosological form of the disease. This point becomes especially relevant if we take into account that during operations specifically on the maxillofacial area, surgeons are especially faced with the task of finding a compromise between choosing the optimal access to carry out the maximum possible radical intervention and causing the least possible aesthetic damage to the patient’s face.
Particular diagnostic issues
Currently, thanks to the introduction of ultrasound diagnostic technologies into obstetric practice, the maxillofacial area becomes an object of medical interest even before the birth of the child. This makes available the intrauterine detection of clefts and other malformations of the fetal face and neck, a number of syndromes with facial signs (Down syndrome, Turner syndrome, Goldenhar syndrome, etc.), as well as recognition of teratomas, hemangiomas and lymphangiomas of the fetus.
Timely detection of these changes forces in some cases to reconsider the approach to pregnancy management tactics or to provide for the need to carry out certain organizational, tactical and therapeutic measures in the perinatal and neonatal periods. This concerns, in particular, the expansion of the obstetric team with the involvement of maxillofacial surgeons to provide specialized care as early as possible.
Ultrasound examination makes a significant contribution to the diagnosis of diseases of the major salivary glands.
In inflammatory diseases of the parotid glands, echography allows for differential diagnosis of various forms of mumps, identifying sialodochitis - inflammation in the ducts of the salivary glands, recognizing inflammation of the intraglandular lymph nodes (lymphadenitis) and clarifying its stage. All this is essentially a distinction between surgical and non-surgical pathology of the parotid glands (Fig. 1-7).
Rice. 1.
Right-sided acute parotitis.
Rice. 2.
Left-sided chronic parenchymal parotitis.
Rice. 3.
Sialodochitis of the left submandibular gland.
Rice. 4.
Acute serous lymphadenitis in the left parotid gland (in two scanning planes).
Rice. 5.
Acute serous lymphadenitis in the left parotid gland with limited periadenitis.
Rice. 6.
Acute serous lymphadenitis with widespread periadenitis (lymphogenous mumps, Herzenberg's mumps) in the left parotid gland.
Rice. 7.
Purulent lymphadenitis in the parotid gland (parotid abscess).
In salivary stone disease, which is most often found in the submandibular glands, ultrasound allows one to identify stones regardless of their location (in the parenchyma of the gland, intraglandular ducts, excretory duct) and the degree of their mineralization, to clarify the presence of sialadenitis - inflammation of the parenchyma of the gland, which can be independent or accompanying salivary stone disease (Fig. 8-11).
Rice. 8.
Salivary stone disease. Calcified calculus in the area of inflection of the excretory duct (typical location) of the left submandibular gland. Associated sialadenitis.
Rice. 9.
Salivary stone disease. Uncalcified calculus in the ampullary part of the excretory duct of the submandibular gland.
Rice. 10.
Salivary stone disease. Calcified stones in the parenchyma of the left submandibular gland. Perifocal edema of the gland parenchyma.
Rice. eleven.
Sialadenitis of the right submandibular gland.
The use of echography in extraorgan inflammatory processes on the face and neck makes it possible to distinguish purulent (abscess, phlegmon) and non-purulent (infiltrate) lesions of soft tissues, and when a purulent lesion is detected, accurately localize accumulations of pus (Fig. 12-14).
Rice. 12.
Infiltration of the left buccal area.
Rice. 13.
Phlegmon of the submandibular region after opening and drainage (drainage is visible).
Rice. 14.
Abscess of the submandibular region.
Visualization of the outer (vestibular) surface of the jaw bones makes it possible to establish periostitis, which is one of the most common causes of inflammatory changes in the soft tissues of the face (Fig. 15).
Rice. 15.
Serous periostitis of the lower jaw on the right. Infiltration in the soft tissues of the right cheek.
The exceptionally developed lymphatic system of the face and neck brings significant specificity to the spectrum of diseases in this area. This applies to both inflammatory and non-inflammatory lesions of the lymph nodes. An echo-graphic study allows one to visualize altered lymph nodes and, based on a number of reference signs (the number of altered nodes, their size, shape and proportions, the nature of the contours, the presence or absence of inclusions and their distribution in the node, the degree of decrease in echogenicity) to reconstruct with a high degree of reliability what is happening in the lymphatic node processes.
In the structure of inflammatory diseases of the soft tissues of the maxillofacial region, inflammatory lesions of the lymph nodes occupy one of the first places. An echographic examination allows one to reliably distinguish reactive (inflammatory) hyperplasia of the lymph nodes from their true inflammation - lymphadenitis (Fig. 16-18).
Rice. 16.
Acute reactive (inflammatory) hyperplasia of the lymph node of the neck.
Rice. 17.
Chronic reactive (inflammatory) hyperplasia of the lymph node of the neck.
Rice. 18.
Acute serous lymphadenitis of the neck.
The key point in choosing a treatment method for lymphadenitis is to determine the nature (stage of development) of the inflammatory process: serous or purulent lesion of the lymph node. Ultrasound examination, even in B-mode, makes it possible to resolve this issue with a high degree of reliability, and the use of blood flow visualization techniques (color Doppler mapping, power Doppler mapping) makes it possible to identify the process of purulent melting at its earliest stage (Fig. 18-21).
Rice. 19.
Purulent lymphadenitis of the neck with periadenitis.
Rice. 20.
Purulent lymphadenitis of the submandibular region.
Rice. 21.
Dopplerographic dynamics of the process of purulent melting of the lymph node (over 3 days).
All this makes it possible to rationally approach the combination of methods of conservative therapy and surgical treatment, to choose adequate treatment tactics, avoiding the use of unjustified treatment methods. In everyday practice, metastatic lesions of the lymph nodes of the neck are often encountered, as well as their involvement in the pathological process in lymphoproliferative diseases. An echographic examination makes it possible to distinguish these groups of diseases with a high degree of reliability and differentiate these types of lesions from inflammatory changes in the lymph nodes.
In case of injury from glass, wooden and plastic objects, as well as after gunshot wounds and road traffic accidents, foreign bodies often remain in the soft tissues of the face and neck, the timely detection of which allows for the most effective primary surgical treatment of the wound and reduces the risk of inflammation.
After gunshot wounds, multiple and, as a rule, metallic foreign bodies usually remain in the soft tissues, the high radiopacity of which allows traditional X-ray examination to see even the smallest of them and determine their skeletotopy. In these cases, echography, of course, is inferior to x-ray examination in determining the number and size of foreign bodies, but ultrasound examination is certainly necessary to clarify their organotopy in relation to soft tissue structures - vascular bundle, muscles and fascia.
In cases where there are glass, plastic or wooden foreign bodies in the soft tissues, echography is essentially the only method that allows you to study the infiltration zone, obtain an image of foreign bodies, determine their number, size, location and organotopy (Fig. 22- 26).
Rice. 22.
Foreign body in the soft tissues of the left parotid-masticatory region (metal ball - air gun bullet).
Rice. 23.
A foreign body in the subcutaneous tissue of the left cheek is a glass fragment.
Rice. 24.
A foreign body in the left cheek area is a splinter.
Rice. 25.
Foreign bodies in the keloid scar of the lower lip are small stones and asphalt crumbs (after a traffic accident).
Rice. 26.
A foreign body in the submandibular region is a fragment of a plastic catheter.
A significant proportion of diseases of the maxillofacial area are congenital cysts of the neck and oral cavity. An echographic examination makes it possible to visualize them, clarify their structure and organotopic characteristics, on the basis of which differential diagnosis is based.
Among congenital cysts of the neck and oral cavity, there are: thyroglossal (middle) and branchial (lateral) cysts and fistulas, retention cysts of the sublingual gland, as well as dermoid cysts.
The urgent need for distinctive recognition of the group affiliation of congenital cysts and fistulas is dictated by the necessity of their radical excision in order to avoid relapse. And if dermoid cysts and retention cysts of the sublingual gland are characterized by a clear demarcation and absence of fistulous tracts, then thyroglossal cysts usually have a connection with the hyoid bone and the root of the tongue, and branchial cysts are often connected by a fistulous tract with the lateral wall of the pharynx (Fig. 27-30).
Rice. 27.
Thyroglossal (median) cyst of the neck. There is a connection with the hyoid bone and the root of the tongue.
Rice. 28.
Branchial (lateral) cyst of the neck. Relationship with the vascular bundle of the neck (compression of the internal jugular vein and displacement of the common carotid artery).
Rice. 29.
Dermoid cyst of the floor of the mouth.
Rice. thirty.
Retention cyst of the right sublingual gland.
Clinicians are well aware of the difficulties in distinguishing between festering cysts and abscessing lymphadenitis. The specificity of the echographic picture makes it possible not only to solve emerging differential diagnostic difficulties, but also to determine the severity of scar changes around the cyst.
Congenital cysts of the neck and oral cavity often have to be differentiated from the cystic form of lymphangioma, which is essentially a malformation of the lymphatic vessels. Cystic lymphangioma is more characterized by multiple chambered cavities or multiple cyst-like formations, as well as significant prevalence. All these signs are clearly identified echographically. In cases of single-chamber and limited prevalence of lymphangioma, differential diagnosis is significantly difficult (Fig. 31).
Rice. 31.
Lymphangioma of the left parotid gland.
In the face and neck area, pathological formations from blood vessels are often found - so-called “hemangiomas”, which in most cases (up to 95-97%) are vascular hyperplasias and vascular malformations (angiodysplasias). True vascular tumors occur only in 3-5% of cases.
In this case, either only the vascular periphery - capillaries, or only larger vessels with the formation of arteriovenous communications (stomachs, fistulas) can be involved in the pathological process; a combination of these options is possible. Dysplastic changes can be localized only in the venous part of the vascular bed; this type of lesion is referred to as “venous dysplasia” (Fig. 32).
Rice. 32.
Venous dysplasia of the right parotid gland.
Vascular formations can have a diffuse distribution in soft tissues or be clearly demarcated, and also have their own hemodynamic characteristics (Fig. 33).
Rice. 33.
Vascular hyperplasia of the right buccal region.
All these factors entail the need for an individual approach to the choice of treatment method and tactics. Ultrasound examination, allowing to determine the main morphological and hemodynamic parameters of vascular formations of the face and neck, is an effective method for their diagnosis.
A very significant role belongs to echography in recognizing tumors of the salivary glands. The possibility of a detailed assessment of the contours of the neoplasm and its internal structure (echostructure) makes it possible to distinguish benign tumors of the salivary glands from malignant tumors with high reliability (Fig. 34-36).
Rice. 34.
Polymorphic adenoma of the left parotid gland.
Rice. 35.
Lipoma of the left parotid gland.
Rice. 36.
Malignant tumor of the right parotid gland (histologically: undifferentiated carcinoma).
Of great importance in clarifying the nature and extent of the tumor process is also the assessment of the condition of the regional lymph nodes, in which echographic examination is a recognized leader (Fig. 37).
Rice. 37.
Malignant tumor of the left parotid gland (histologically: adenoid cystic carcinoma). Metastatic lesions of regional lymph nodes.
The abundance of lymphoid tissue in the parotid glands determines the high frequency of their damage by benign and malignant lymphoproliferative diseases, which also have their own characteristic echographic signs (Fig. 38-39).
Rice. 38.
Damage to the left parotid gland due to lymphoproliferative disease (histologically: lymphogranulomatosis).
Rice. 39.
Damage to the lymph nodes of the neck due to lymphoproliferative disease (histologically: lymphosarcoma).
Without in any way contrasting ultrasound of the maxillofacial area with the traditional clinical examination of the patient, there is every reason to assert that the use of echography is certainly indicated not only in diagnostically unclear cases, but even with an already established diagnosis, when the method allows us to identify individual characteristics of the course of the disease , which can be significant when planning a patient’s treatment.
The non-invasiveness and harmlessness of ultrasound examination makes it possible to carry it out many times to monitor the dynamics of the pathological process and evaluate the effectiveness of treatment measures.
The high information content of an echographic examination (reaching 95-98% in general) makes it possible to limit the use of radiological techniques (traditional radiography, sialography, angiography), significantly less often use invasive diagnostic interventions (soft tissue biopsy) and more rationally approach the use of such expensive studies as computer and magnetic resonance imaging.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.