Jaw cancer is a malignant neoplasm that affects bone tissue. The disease has no age restrictions; it is characterized by rapid growth, metastasis, and pronounced pain. The structural features of the maxillofacial region, proximity to important vessels and nerve centers further complicate treatment.
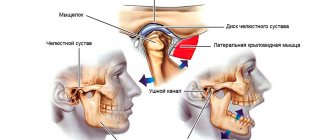
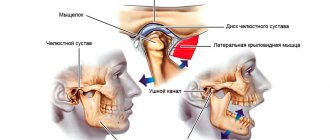
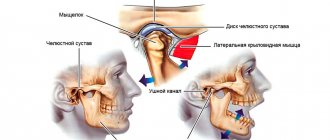
Anatomical structure
The oral cavity is the initial section of the digestive tract, in which food is chewed and saliva is produced to digest food. It is involved in the process of breathing, swallowing, articulation and speech.
The composition of the oral cavity includes:
- vestibule (lips, front side of teeth, inner surface of cheeks);
- gums;
- the bottom on which the tongue lies;
- two thirds of the tongue;
- teeth;
- retromolar triangle - the space on the lower jaw behind the third molar;
- hard and soft palate.
Classification
Oral cancer is divided into three types:
- papillary. The nodule in the mucous membrane increases in size and hangs into the oral cavity. The neoplasm progresses slowly;
- infiltrative. The seal on the pinkish mucosa is distinguished by a whitish color, clear contours and shape, and thinning of the membrane around it. On palpation from the side of the cheek, a dense infiltrate is felt. The tumor tends to grow rapidly. The patient complains of unbearable pain;
- ulcerative The most common form of the disease. Ulcers on the mucous membrane do not heal, they grow, and the border around them turns red. The outline is torn and its edges are bleeding.
Tumor metastases appear quickly. Malignant cells grow into the mental, submandibular, and deep jugular lymph nodes. This process is influenced by the thickness and depth of the tumor. Thus, when the tumor deepens by 4-5 mm, metastases occur in 98% of cases. At the T1 stage of oncology, metastasis is detected in half of the cases, and when the T4 stage is reached, distant spread of cancer cells is observed in 85% of cases.
Detection of pathology
Detection of tumors of the lower jaw is based on a thorough study of the course of the disease, as well as morphological and radiological data. The diagnosis is made by x-ray, since x-rays can detect destructive changes in the bone early.
In the initial stages of sarcoma or jaw cancer, x-rays show bone loss. Its changed area does not have clearly defined boundaries; they are blurred. If jaw cancer is localized in the area of the alveoli, then the cortical plates of its walls are destroyed, and an extensive zone of destruction of the spongy substance is visible around the circumference. If the process has spread, then the radiograph shows complete destruction of a certain part of the bone.
Histological analysis of the tissues of the surface of the extracted tooth during its mobility is informative. It is always necessary to strive to establish the cause of loose teeth. If the mucous membranes of the mouth have ulcerations and the area is clearly visible, a cytological analysis of the mucosa is performed to confirm the diagnosis.
Causes
The prevalence of oral cancer is growing and is currently diagnosed in 2% of patients among the total number of cases. Since 2009, the incidence has increased by 25%, with mostly squamous cell carcinoma being detected and only in isolated cases adenocarcinoma.
Most foci of oncology are observed in the tongue. Slightly less malignant formations on the floor of the mouth. Cancer of the soft and hard palate, gums and cheeks is detected in 20% of cases. Much less frequently diagnosed is damage to the alveoli of the lower jaw - 4%, the arches of the palate, retromolar region and vestibule - 3%.
Based on practice, men are more susceptible to oral cancer than women. This is due to bad habits, for example, the abuse of cigarettes or chewing tonic mixtures increases the production of saliva, which washes away beneficial elements from the mucous membrane. The risk group includes patients with HPV, elderly people, workers in hazardous industries, patients with lichen planus, people whose oral mucosa is systematically injured by fillings, prostheses, and metal objects.
Risk factors
Most malignant tumors of the oral cavity arise in already changed tissues. Usually these are long-term inflammatory changes and various precancerous conditions. Precancer is a special condition of tissues in which at some point their malignant degeneration may occur, although a benign tumor and a complete return to normal state may be a possible outcome. The causes of precancerous conditions and their progression into a malignant process are not known with certainty. Scientists suggest that this depends on the immunobiological status of a person and the characteristics of exposure to the carcinogen.
Factors that contribute to the appearance of precancerous changes can be both external damaging agents and various disorders in the body:
- Constant mechanical impact - malocclusion, poorly fitting dentures.
- Chemical agents - alcohol, tobacco smoke, spices, industrial irritants.
- Temperature agents - constant consumption of very hot food, hot tobacco smoke, work in hot shops.
- Biological agents: various microorganisms of the oral cavity, both frankly pathogenic and opportunistic, which make themselves known only under favorable conditions.
- Ionizing radiation, including due to medical procedures.
- Diseases of the digestive system.
- Some systemic lesions, in particular lupus erythematosus.
Among these factors, one of the most important is biological. There has been a proven connection between precancerous changes in the oral mucosa with caries and gum disease due to excessive bacterial growth. The second, but no less important factor is smoking - the disease is registered in smokers 6 times more often than in non-smokers.
Symptoms
A malignant ulcer from ordinary stomatitis in the mouth can be identified by swelling and swelling of the cheeks, pain and constant discomfort even at rest. You should be wary of prolonged non-healing of the wound and its bleeding.
As the disease progresses, the symptoms intensify:
- swelling increases and spreads to the neck;
- the red or white spot on the oral mucosa intensifies;
- discomfort when chewing and swallowing;
- difficulty speaking due to friction of the mucous membrane on the teeth when moving the jaw;
- the appearance of bad breath;
- feeling of a foreign object in the throat;
- anemia of the mouth.
In the late stages of cancer, teeth fall out and body weight rapidly decreases.
General information
Jaw tumors refer to neoplasms in the cat's tissue. This pathology accounts for 13 to 29% of the total number of dental surgical diseases.
Due to its close location to the teeth, brain and eyes, the pathology is characterized by a special clinical course. Tumor formations in this area lead to functional disorders, aesthetic defects and even death.
Depending on the tissue of which the tumor is composed, it can be osteogenic or non-osteogenic. According to the clinical development of pathologies, there are malignant, benign or locally destructive.
Treatment of jaw tumors is a complex and lengthy task that requires high competence and professionalism from the doctor.
Diagnostics
At the initial consultation, the doctor examines the oral cavity, examines ulcers, erosions, damage to the mucous membrane, and then takes a smear for examination. To confirm the inflammatory process, the patient is sent for a general and biochemical blood test.
The diagnosis is confirmed by the results of the examination:
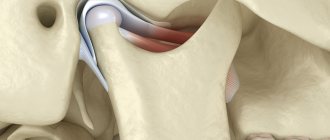
- MRI and ultrasound of soft tissues of the neck. The images reveal the localization of the pathology, the depth of germination and the structure of the tumor, compaction from blood and lymph, decomposition of the cortical layer of the bone;
- if metastases are suspected, a fine needle aspiration biopsy of the lymph nodes under the chin, under the jaw and in the upper third of the neck is performed;
- positron emission tomography. Shows the depth of the tumor, as well as early metastases;
- osteoscintigraphy. Skeletal bones are examined to look for displaced cancer cells;
- CT scan of facial bones with contrast. The images show the tumor growing into the neck vessels, jaw or base of the skull.
Forecast criteria
The survival rate of patients with maxillary sinus cancer averages about 40% over 5 years.
At an early stage, when treated in European oncology clinics, tumors have a cure rate of up to 80%.
Patients with unresectable tumors treated with radiation had a survival rate of less than 20%. Survival rates have now improved slightly due to advances in skull base surgery.
In patients with squamous cell carcinoma of the nasal cavity or maxillary sinus, better survival outcomes are achieved when patients receive adjuvant radiation therapy, adjuvant chemoradiotherapy, or neoadjuvant therapy in addition to surgery.
In patients with sinonasal adenocarcinoma, better disease-free survival was associated with surgery followed by radiation therapy compared with surgery alone, for all tumor stages (T1-T4).
Treatment
The choice of treatment tactics depends on the stage and extent of the tumor. When the tumor grows rapidly, treatment methods are combined.
Operation
The doctor determines the principle of surgical intervention after determining the stage of the tumor and its spread. If cancer cells have penetrated the periosteum and surrounding tissues, a wedge-shaped, planar or sagittal resection of the jaw is performed. If the examination reveals the growth of cancer cells directly into the bone or the defect is noticed during surgery, segmental resection of the lower jaw is performed. The doctor assesses the lesion on site and determines the thickness of the excised layer.
The next stage of the operation is partial or complete excision of the cervical lymph nodes to prevent metastases if the thickness of the tumor is more than 4 mm or the location of the tumor in the floor of the mouth or on the tongue. If the tumor is located in the midline, then the cervical lymph nodes are excised on both sides. The operation ends with the immediate replacement of damaged tissue.
After removal, the tumor is sent for histological examination. Its size, thickness, depth, edges are assessed. Further treatment is affected by cell growth beyond the boundaries of the capsule of the removed lymph node, and the spread of cancer cells to neighboring organs.
Radiation therapy
Radiation after surgery is prescribed when diagnosing T3, T4, N2, T3 stages of the disease no later than six weeks after tumor removal. The need for radiation therapy increases with perineural invasion of the lymphatic vessels. The total focal dose for all sessions is 60 g, and the single focal dose for one session is 2 g. When metastases are detected on the neck, the SOD increases to 66 g, and if there is no risk of metastasis, the SOD decreases to 50 g.
As the main treatment, radiation therapy is used in a total focal dose of 60-70 g. The procedure is performed five days a week and is combined with chemotherapy. Every three weeks, 100 mg of cisplatin is administered.
Chemotherapy
Anticancer drugs are prescribed before surgery or along with radiation therapy to reduce the size of the tumor. Sometimes therapy is prescribed simultaneously with surgery.
Treatment involves the use of a 5-fluoroacyl regimen together with cisplatin or other agents - carboplatin, methotrexate, bleomycin. They cause a number of side effects, for example, vomiting or nausea, hair loss, decreased appetite, and increased bleeding. Symptoms disappear after treatment, but permanent hearing loss is sometimes observed after taking cisplatin.
The prognosis of oral cancer depends on the stage at which the disease is detected. If treatment is started at stage zero, the disease will stop. It is worth noting that smoking provokes relapse or degeneration of the tumor, so repeated surgery or radiation may be required. Surgery at the first stage increases survival rate to 80-85%, and the combination of radiation therapy with surgery at the second stage by 60-80%. Already at subsequent stages of cancer development, the survival rate is no more than 50%, and all three treatment methods are used simultaneously.
Tomotherapy for oral cancer
The use of external beam radiation therapy is accompanied by two problems: damage to healthy tissue and insufficient regression of the tumor. Side effects sometimes completely neutralize the achieved treatment result and increase the risk of developing postoperative complications. Intensity modulated radiation therapy (IMRT), and in particular TomoTherapy HD technology, can solve these problems and increase the effectiveness of radiological treatment.
TomoTherapy HD is a complex that combines a computed tomograph and a modern particle accelerator. The system allows you to accurately deliver a dose of radiation to a tumor, no matter how complex it is (localize the tumor, plan treatment and carry it out), protecting healthy tissue from radiation exposure. This approach can significantly reduce the risk of unwanted manifestations.
The ability to deliver a dose of radiation with minimal impact on healthy tissue allows for a more pronounced effect on the tumor and reduces the likelihood of severe side effects in the future
Dispensary observation
Since the tumor can recur and metastasize, after completing the course of treatment the patient is registered with the oncology clinic. The first year you should visit a doctor every month, the second year a preventive examination is carried out every 4-6 months, and then once a year or in case of any ailments. The examination involves an examination - ultrasound and contrast MRI of the soft tissues of the neck, PET, osteoscintigraphy. Consultation with an otolaryngologist, dentist and oncologist is required. The doctor may shorten the period of medical examination if there is a high risk of relapse.
List of references on the topic:
- Gantsev Sh.H. Oncology – M, 2012 – P.204-205.
- Golovin D.I. Errors and difficulties in diagnosing tumors, D.: Medicine. Leningr. department, 2015 305 pp.
- Selected lectures on clinical oncology/Ed. IN AND. Chissova, S.L. Daryalova. – M., 2010
- Matyakin E.G., Alferov V.S. Chemotherapy of head and neck tumors // Mat. 2nd Ros. oncol. conf. “Current trends in the development of drug therapy for tumors” December 8–10, 2016 – M., 256 p.
- Tumors of the head and neck: hands/ A.I. Paches. - 5th ed., add. And revised - M.: Practical Medicine, 2013. -478 p.
- Shine A.A. Oncology. M – 2014 365 pp.
- Encyclopedia of Clinical Oncology/Ed. M.I. Davydova. – M., 2014 –P.140-179.
- Bityutsky P.G., Kitsmanyuk Z.D., Trofimov E.I. Diagnosis and treatment of cancer of the oral mucosa // Medical consultations. - 2014. - No. 1. - P. 23-27.
- Byakhov M. Yu. Options for combined and complex treatment of locally advanced cancer of the oral mucosa and oropharynx: Dis. Dr. med. Sci. - M., 2013.
Stages of the disease
Stage I is characterized by the presence of a tumor up to 1-2 cm in diameter, not extending beyond the affected area (cheek, gums, palate, floor of the mouth), limited to the mucous membrane. Metastases are not detected in regional lymph nodes.
Stage II - a lesion of the same or larger diameter, which does not extend beyond any one part of the oral cavity, but extends into the submucosal layer. There are single metastases in regional lymph nodes.
Stage III - the tumor grows into the underlying tissues, but not deeper than the periosteum of the jaw, or has spread to adjacent parts of the oral cavity. In regional lymph nodes there are multiple metastases measuring up to 2 cm in diameter.
Stage IV - the lesion spreads to several parts of the oral cavity and deeply infiltrates the underlying tissues, in the regional lymph nodes there are immobile or disintegrating metastases, and the presence of distant metastases is also characteristic.
Classification by stages is periodically subject to revision; you can find a division of stages into subtypes - A and B. Currently, classification by stages is used less and less, the TNM classification is more relevant. Its principle is that this coding indicates the characteristics of the tumor itself, the condition of the closest (regional) lymph nodes, and the presence or absence of distant metastases.
In the diagnosis, the oncologist indicates the histological type of cancer, since different types of cells differ in growth rates, tendency to metastasize, and sensitivity to treatment. All types of classifications serve one purpose - to correctly assess the extent of the spread of the disease, the degree of damage and develop the right tactics of assistance.
Book a consultation 24 hours a day
+7+7+78