Surgical removal of the parotid gland is called a parotidectomy . In most cases, surgery is performed due to the presence of a tumor, often benign, of the parotid salivary gland.
Parotid salivary gland and facial nerve - schematic drawing
The salivary glands secrete saliva into the mouth to digest food and protect against infections. When the parotid glands are removed, there are no problems with the secretion of saliva - this function will continue to be performed by the remaining salivary glands: the submandibular, sublingual, and numerous small glands.
The parotid gland is penetrated by nerves, veins and arteries. We are interested in the facial nerve.
Indications
Indications for removal of the submandibular salivary gland are:
- chronic sialadenitis (inflammation);
- benign or malignant tumors;
- multiple cystosis;
- salivary stone disease;
- severe injury to the gland;
- complete blockage of the salivary ducts with the impossibility of restoring their patency.
Depending on the diagnosis, various tests are prescribed before the operation - ultrasound, computed tomography or magnetic resonance imaging, chest x-ray. In the case of a tumor, a biopsy is also necessary to determine the nature of the formation. Salivary stone disease is examined using contrast sialography.
Indications for removal
The main reason for prescribing surgical intervention is the ineffectiveness of conservative therapy.
This often occurs with the development of the following diseases:
- Inflammatory process or sialadenitis. Develops against the background of exposure to a bacterial or viral infection. Symptoms are an increase in the size of the affected area, pain, a decrease in the volume of salivary fluid production, and general malaise.
- Pathological narrowing (expansion) of the excretory duct or sialodochitis. Symptoms are increased production of salivary fluid, a salty taste in the mouth, swelling, distension in the area, pain during eating, stuffy ears.
- Formation of stone-like deposits in the lumen of the gland or sialolithiasis. Surgical intervention is prescribed when the stone reaches a size of 1 mm, which clogs the duct and cannot be washed out by conservative methods. Symptoms are bloating, swelling, unpleasant taste in the mouth, periodic acute pain, difficulty swallowing saliva. At an advanced stage, general intoxication occurs.
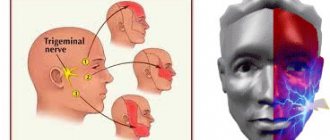
- Bilateral swelling of a non-inflammatory and non-tumor nature or sialosis. Symptoms: local pain syndrome, impaired activity of the facial nerve.
- Mumps or mumps. Develops when the body is infected. Symptoms are swelling of the endocrine glands, high fever, loss or decreased appetite, general malaise, headache.
- Purulent lesion.
- The presence of a tumor-like neoplasm.
- Severe mechanical damage.
For sialodochitis and sialosis, surgical treatment is prescribed in extreme cases, if the swelling has reached its maximum size, thereby causing facial asymmetry.
Preparation for the operation and features of its implementation
Preoperative preparation includes:
- laboratory tests;
- abolition of blood-thinning medications (at least a week before the procedure);
- changing your diet three days before surgery - excluding alcohol, spicy and rough foods, hot drinks.
- Smoking is also prohibited before surgery.
Removal of the submandibular salivary gland is a complex and specific operation, since its anatomical location near the nerve and choroid plexuses, muscles and other organs is associated with risks of serious complications. Such a procedure can only be performed by experienced specialists - dental surgeons or maxillofacial surgeons.
In the case of a malignant tumor, especially when it grows beyond the gland, the organ is removed along with the affected tissue of nearby muscles and lymph nodes. In other cases, only gland tissue is removed.
Surgery to remove the submandibular salivary gland can be performed in several ways:
- The traditional method is surgical excision of tissue with removal of the pathological gland. This type of operation does not require specific equipment, which explains its lower cost and speed of implementation. Postoperative wounds are quite large; the time for suture removal varies from 1 to 3 weeks.
- A microsurgical endoscopic operation that does not require large tissue intersections - all actions are carried out using manipulators, and observation is carried out using a probe that transmits an image to the screen. The great advantage of this type of operation is the targeted effect, due to which in case of salivary stone disease, benign tumors and cystosis of the gland, there is no need for its complete removal - only a small area of it is excised. After the operation, small marks remain, the stitches are removed after a few days. The disadvantage of this method is its high cost.
Diagnosis of salivary gland cancer in Israel
The quality of the subsequent course of treatment depends on the accuracy of the diagnosis. Therefore, Israeli clinics use advanced equipment and modern techniques for examining patients. The following diagnostic methods are usually used:
- Examination and consultation with an oncologist.
- Ultrasonography. Ultrasound helps determine the location and size of the affected area of the salivary gland.
- MRI. During the session, the person lies motionless in the apparatus. All metal objects must be removed before the examination. Patients whose body weight is more than 150 kg are not required to undergo MRI. The duration of the examination is no more than an hour.
- Biopsy. Cells are collected from the tumor-affected area of the gland using a thin needle and syringe.
- CT scan. The procedure allows you to obtain an image of any necessary area of the patient’s body. If necessary, a certain amount of dye is injected into the vein. This is necessary to improve the quality of the pictures. The examination of one area lasts about 20 minutes. The dye is eliminated from the patient’s body on its own within a few days.
If the diagnosis has confirmed that the tumor is not malignant, its treatment is still recommended. The fact is that about eighty percent of benign tumors eventually degenerate into malignant ones. Cancer treatment in Israel is a priority. Specialists of the Tlv.Hospital consultation center will take care of all issues related to organizing the diagnosis and treatment of salivary gland cancer in Israel.
Performing surgery to remove the salivary gland
With the traditional method of surgery, the patient assumes a lying position with his head thrown back and to the side. The operation involves local infiltration anesthesia. Several parallel incisions are made in the submandibular area, the tissue is lifted, and the capsule of the salivary gland is discovered, which is opened, and the gland tissue is extremely carefully removed and removed. When a malignant tumor grows together with nearby tissues, the latter are also removed. After this, stitches are applied.
During endoscopic surgery, both local and general anesthesia can be used. Through small punctures in the tissue, manipulators and a video probe are inserted, which projects all the actions performed on the screen. When the manipulators reach the gland, small incisions are made with their help, through which pathological tissue is removed. The endoscopes are then removed and sutures are placed at the puncture sites.
Postoperative care of the surgical site includes:
- hygiene - no water or dirt should get into the wounds;
- special diet - the diet will consist of semi-liquid warm food, no hot or cold drinks, no alcohol;
- smoking ban;
- special treatment - it is recommended to regularly treat the seams with antiseptics, and the oral cavity after each meal should be rinsed with a mixture of antiseptic and water.
If all the recommendations of the attending physician are followed, complete wound healing occurs within a few months.
Pleomorphic adenoma (mixed tumor). This benign tumor is the most common, occurring in 72% of all epithelial tumors of the salivary glands. In terms of frequency of lesions, the parotid salivary gland is in first place, the mucosalivary glands of the palate are in second place, then, respectively, the submandibular, sublingual and minor salivary glands, glands of the lip, cheek, and tongue.Pleomorphic adenoma grows painlessly, slowly, over several years and can reach large sizes. When the adenoma is localized in the parotid salivary gland, paresis of the facial muscles is not observed. Upon examination, a tumor is detected in the area of the salivary gland, mobile, often with a bumpy surface. Its consistency is densely elastic, sometimes with areas of softening due to the mucus-like component. The skin above it does not change, it folds freely. The salivary function of the affected gland is usually not affected. Pleomorphic adenoma has a capsule, but may not be completely encapsulated, in which case the tumor cells penetrate into the adjacent glandular tissue. This explains tumor recurrences after extracapsular removal. Sometimes tumor growth accelerates significantly (within 1 month), and pain may appear. Such symptoms are characteristic of tumor malignancy; in such cases it is interpreted as carcinoma in pleomorphic adenoma.
The diagnosis of a tumor is clarified by cytological examination of the punctate, which is obtained in the needle in the form of a crumbly whitish mass.
Macroscopically, pleomorphic adenoma is a tumor in a thin translucent capsule, on a section in the form of a pasty mass of white-gray color with areas of mucus and compaction.
Microscopically, the tumor, in addition to pronounced epithelial tissue, contains mesenchyme-like areas consisting of myxoid or cartilage-like structures, the presence of which is explained by the accumulation of mucoid or hyaline substance between the myoepithelial cells.
Treatment is surgical. If the tumor is localized in the submandibular and sublingual salivary glands, the tumor is removed along with the gland. Tumors located on the palate, cheek, lips, tongue are excised within unaffected tissues. The peculiarity of the operation on the parotid salivary gland is associated with the branching of the facial nerve in the thickness of the gland. The nature and extent of surgical intervention depend on the size and location of the tumor. In all cases, it is necessary to excise the tumor with adjacent glandular tissue. Some authors suggest extracapsular tumor removal. When the tumor is localized in the lower pole of the gland, resection of this section is used. If the tumor occupies the anterior section and lies in the gland above the branches of the facial nerve, subtotal resection of the gland is performed in the plane of the branches of the facial nerve. Parotidectomy with preservation of the branches of the facial nerve is performed when most of the gland is affected and the tumor recurs, as well as when there is a tumor of the pharyngeal part of the gland. Access to the gland is carried out by two well-known methods - Kovtunovich and Redon. In the first case, the operation begins with exposure of the peripheral part of the facial nerve (middle branch), in the second - the central trunk.
The operation is parotidectomy with preservation of the branches of the facial nerve. A skin incision is made in front of the auricle 2-3 mm, starting from the scalp of the temple, bordering the earlobe and continuing in the retromaxillary and submandibular areas. the skin-fat flap is prepared and retracted anteriorly. The parotid-masseteric fascia and the anterior edge of the gland are exposed. When approaching the peripheral branches of the facial nerve, the location of the middle branch is determined: it is located next to the duct of the parotid gland along the line connecting the tragus with the angle of the mouth. The middle branch is dissected to the point of division of the trunk, then the upper and lower branches are isolated from the gland, holding them with threads to reduce trauma. The surface layer of the gland is removed, bandaged and the salivary duct is crossed. By lifting the branches of the nerve, the deep and pharyngeal parts of the gland are dissected and removed along with the tumor, and the external carotid artery is ligated along the way.
In an operation using the Redon method, after removing the skin-fat flap, the posterior edge of the gland is released and the external carotid artery is ligated. Then the trunk of the facial nerve is found deep in the wound between the mastoid process and the posterior edge of the mandibular ramus. The location of the nerve branch is determined and all three main branches are prepared. The further course of the operation is identical to that described.
An operation that involves removing only the superficial layer of the gland along with the tumor located above the branches of the facial nerve is called subtotal resection of the glands in the plane of the nerve branches.
In case of resection of the lower pole of the parotid salivary gland, a skin incision is made bordering the angle and body of the jaw, moving downwards by 1.5-2 cm, so as not to damage the marginal branch of the facial nerve. This must also be remembered during excision of the gland due to its location in this area. Subcutaneous tissue is dissected, m. platysma and fascia. The lower part of the gland, where the tumor is located, is exposed and removed. The wound is sutured in layers.
A mucous retention cyst most often forms in the minor mucosalivary gland of the lower lip, less commonly in the cheek, the anterior floor of the mouth, the lower surface of the apex of the tongue and palate. The predominant localization on the lower lip is associated with biting it.
The cyst is located under the mucous membrane, has the appearance of a hemispherical elevation with clear boundaries, ranging in size from 0.5 to 2 cm, with a bluish tint. Sometimes the mucous membrane over it is whitish in color, which is due to the presence of scar changes due to injury. Palpation of the cyst is of elastic consistency with ripple, painless. Biting the mucous membrane over the cyst can lead to its emptying, releasing a clear, viscous fluid. When the contents become infected, inflammation occurs.
Pathohistologically, the cyst wall is a connective tissue with granulations, turning into fibrous tissue, sometimes the inner side of the wall is partially lined with stratified squamous epithelium.
A mucous retention cyst must be differentiated from tumors of the minor salivary glands, which are less common, have an elastic consistency, sometimes with a bumpy surface, without fluctuation. In some cases, it is necessary to differentiate it from cavernous hemangioma, which is characterized by a purplish-bluish coloration and a symptom of filling.
Treatment consists of removing the cyst. Two converging semi-oval incisions are made in the mucous membrane above the cyst. Using a hemostatic mosquito clamp, the membrane is separated semi-bluntly from the surrounding tissues, the connective tissue bridges are cut with scissors and the cyst is isolated. Injured small glands protruding from under the edges of the wound and interfering with suturing are removed with tweezers or a “mosquito”, each separately and entirely. Using a scalpel for these purposes can lead to their dissection, incomplete removal and recurrence of the cyst. The operation is completed by applying catgut sutures to the mucous membrane.
Cyst of the sublingual salivary gland (ranula). This cyst is located, as a rule, in the anterolateral part of the floor of the mouth near the frenulum of the tongue. Clinically defined as an oval bulge, covered with unchanged mucous membrane or translucent with a bluish tint. The cyst is always intimately associated with one of the areas or the entire sublingual salivary gland. Its former name ranula (“frog tumor”) is determined by the type of cyst and its resemblance to the laryngeal bladder of a frog. It grows slowly, over months, and does not cause pain. When it reaches a significant size, speech is impaired and eating becomes difficult. Sometimes the cyst can extend beyond the midline of the floor of the mouth, displacing the tongue posteriorly or into the submandibular region. In the latter case, it is difficult to differentiate from a cyst of the submandibular salivary gland. On palpation, the cyst often appears as a formation with fluctuation, sometimes it is more elastic. When the membrane breaks through, a viscous transparent fluid is released abundantly from the cyst, and it is not contoured. After time, the cyst fills with fluid again and becomes visible.
Microscopically, the cystic fluid contains protein substances (clumps) and sometimes so-called cystic cells, apparently of epithelial origin.
Macroscopically, the cyst shell is thin, bluish-white. In terms of its microstructure, it is fibrous and granulation tissue associated with the interlobar connective tissue layers of the gland. The inner lining of the membrane rarely has cubic or columnar epithelium.
Diagnosis of a sublingual salivary gland cyst is usually not difficult. It should be differentiated from a cyst of the submandibular salivary gland, a dermoid cyst and vascular tumors (lymphangiomas and hemangiomas) localized at the bottom of the oral cavity.
Treatment: given the close connection of the cyst with the parenchyma of the gland, they are completely removed. The previously recommended cystotomy has limited use due to the frequent development of relapses. A cyst of the sublingual salivary gland, which spreads in the lower part of the floor of the oral cavity in the form of an hourglass, is operated on in two approaches: through an incision in the submandibular triangle, the lower part is bandaged and removed; from the side of the oral cavity, the sublingual gland with the remaining part of the cyst is excised.
A cyst of the submandibular salivary gland is much less common than a ranula. It is located in the submandibular triangle and is a painless formation of soft consistency. It grows slowly and is detected by chance when a swelling is detected in the submandibular region. A large cyst pierces the mylohyoid muscle (m. mylohyoideus) or bends around it from behind and spreads to the upper part of the floor of the mouth. In these cases, its bulging into the sublingual area is also determined. The salivary function of the gland is not affected.
Diagnosis of a cyst of the submandibular salivary gland is sometimes difficult. To clarify the diagnosis, a puncture is used: obtaining a yellowish mucous fluid suggests the presence of a cyst.
A cyst of the submandibular salivary gland is differentiated from lymphangioma, lipoma, lateral neck cyst, dermoid cyst.
To determine the topography of the cyst, a double contrast method is used: cystography and sialography. Different X-ray projections allow you to determine the relationship between the cyst and the gland
Treatment. The cyst of the submandibular salivary gland is removed along with the gland.
Parotid salivary gland cyst. This is a rare disease, localized in the superficial and deep layers of the gland, mainly in the lower pole. The cyst grows slowly. It is often discovered by accident.
The cyst is a limited, painless swelling in the parotid region of soft elastic consistency. The skin over the cyst is of normal color and gathers loosely into a fold. Unchanged saliva is released from the gland duct. The contents of the cyst are yellowish liquid, sometimes cloudy, mixed with mucus. Histologically, the walls of parotid salivary gland cysts do not differ from the walls of cysts of other salivary glands.
A parotid salivary gland cyst is differentiated from organ-specific tumors, lipomas, vascular tumors of the gland, as well as from a branchial cyst caused by pathology of the first branchial cleft.
Treatment consists of removing the cyst. Due to the close connection of the cyst shell with the parenchyma of the parotid gland, the adjacent section of the latter is excised. The complexity of the operation is related to the location of the branches of the facial nerve. Surgical access to the gland is the same as when removing benign tumors of the parotid salivary gland.
"Surgical Dentistry" edited by Robustova T.G.
Fourth edition. Moscow "Medicine" 2010
Clinical cases:
Pleomorphic adenoma of the left parotid salivary gland.
Types of surgical operations
When problems with the functioning of the gland are detected, the doctor’s main task is to preserve the glandular tissue.
There are the following types of operation:
- endoscopy is the most gentle operation, which is prescribed in the presence of a stone-like stone in the lumen and narrowing of the duct;
- resection, prescribed for the purpose of excision of a cyst, a tumor-like formation of a small volume;
- extirpation is an intervention necessary to remove a malignant neoplasm along with nearby lymph nodes, part of the facial nerve, skin (sometimes with bone tissue).
The features of the intervention differ depending on the location of the affected area.
Removal of the submandibular gland
The organ is removed through external access, cutting the skin in the chin area.
After excision, the wound is sutured. To reduce swelling and prevent the accumulation of pathological fluid, a drainage tube is inserted into the incision, through which the exudate comes out. The drainage is removed after 2-3 days.
If the reason for removal is the presence of a tumor-like neoplasm, the excised biological material is sent for histological examination. This will determine the nature of the growth and the presence of malignant cells in it.
The duration of the operation to remove only the affected organ is up to 40 minutes. If excision of nearby tissues or lymph nodes is required, the time increases to 2-3 hours.
Extirpation on video:
Excision of the parotid gland
It is removed by first making an incision on the cover in the ear fold. If a tumor is present, a superficial parotidectomy is indicated. The facial nerve and its branches are preserved if the formation does not involve them in the lesion and is located higher.
In other cases, when nerve branches are involved in the lesion, extirpation is prescribed, during which the lymphatic mesh is removed and the underlying tissue is excised.
The duration of the operation is approximately an hour. The wound is sutured, and a drainage tube is inserted into the incision to remove exudate.
Sublingual extirpation
In this case, the sublingual gland is removed through the mouth. The duration of the operation is up to 30 minutes. Indications for extirpation are small adenoma or cyst.
If the tumor has reached a significant size, a second access is created through the skin under the chin. In such cases, complete excision of the organ is required.
Recovery period
Activities during the early recovery period are assigned to a medical professional. The doctor checks the level of functioning of the facial muscles, treats the operated area and the place with a drainage device, and prepares a dietary diet for the patient.
It is recommended to start following a proper diet immediately after discharge from the hospital. Food is served ground, semi-liquid, neither hot nor cold (optimally at room temperature). Spicy, salty, and sour foods are excluded from the diet.
Among the permitted products:
- vegetable puree: from potatoes, carrots, zucchini;
- pureed soup from broth cooked with lean meat (chicken or turkey);
- semi-liquid porridge (wheat, oatmeal).
After eating, rinse the mouth with warm water or herbal infusion (chamomile, calendula, oak bark).
After surgery, the person operated on can lead a normal lifestyle.
To exclude recurrence of the primary disease and complications, it is enough to adhere to the following simple rules:
- keeping the postoperative area clean;
- cleansing the wound surface with hydrogen peroxide twice a day or antibacterial ointment (as prescribed by a doctor);
- Cleaning the operated area with mild soap and water after removing the suture.
Symptoms such as fever, general malaise, swelling, pain, bleeding, nausea and vomiting syndrome, feeling of shortness of breath, discomfort in the sternum should be a reason to consult a doctor.
Removal of small glands
More often, surgery on small glands is performed for adenoma, cyst, or stones in the duct.
Before the operation, the patient is given a local anesthetic drug. The operation is performed on an outpatient basis. The stitches are removed after about a week. Features of care and nutrition are similar to those provided after excision of large glands.
The photo shows the suture after the operation:
Possible complications and consequences
According to numerous reviews from those who have undergone the procedure, complications are rare after removal of the salivary gland, but the operation does not guarantee the absence of the risk of negative consequences.
- paresthesia (partial or complete numbness) of the face and ear from the operated organ;
- violation of the integrity of the nerve responsible for the mobility of the facial muscles;
- ingrowth of salivary nerve fibers into the sweat glands, which is characterized by increased sweating in the operated area;
- hemorrhage;
- the addition of a secondary infection with corresponding symptoms;
- swelling of the respiratory tract;
- tissue scarring;
- the formation of a fistula between the oral cavity and the nose, throat, and skin;
- with the development of cardiovascular pathology - heart attack, stroke.
Those at risk for complications include people with high blood pressure, diabetes, and those who abuse smoking and alcoholic beverages. This also includes elderly patients.
In the photo, facial paresthesia is a possible consequence of removal of the salivary gland:
Gymnastics to restore facial muscles
If the functioning of the facial muscles is impaired, you can perform special exercises: puff out and retract your cheeks, stretch your smile to the sides, stretch out your lips, close your eyes, and wink. Exercise therapy is indicated 2 weeks after surgery. Each exercise is repeated up to 5 times daily. The duration of one exercise therapy session is up to 15 minutes.
Gymnastics for the face, video:
Extirpation of the salivary gland is not an operation with a high risk of complications and recurrence of the primary disease. However, to reduce the possibility of negative consequences after the intervention, it is recommended to follow the doctor’s recommendations.