- Facial neuritis is an inflammatory disease that causes partial, unilateral paralysis or paresis of the face.
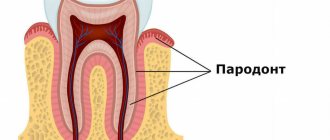
The facial nerve is responsible for contractions of facial muscles and consists primarily of motor fibers. It is one of twelve paired cranial nerves. It begins in the brain and, branching, innervates the face. Its inflammation can occur both at the base (in the core area) and throughout, involving one or more branches. Depending on this, the symptoms of the disease vary.
In most cases, treatment of neuritis of the facial nerve is carried out using conservative methods, and only in the most severe cases (for example, with injuries with a complete rupture of the nerve canal), if therapy is ineffective, surgical treatment is used.
At the Tibet Clinic, treatment of neuritis of the facial nerve is carried out without surgery, using reflexology and physiotherapy. Positive results are achieved in 97 - 98% of cases.
As a result of treatment, contractions of the facial muscles and facial symmetry are restored, spasticity and other symptoms disappear, and the inflammatory process is stopped. These results are long-term and persistent.
Information about the disease
The facial nerve is responsible for ensuring the movements of facial muscles, the lacrimal gland, the tensor tympani muscle, and also innervates the anterior two-thirds of the tongue. It leaves the skull in a narrow canal located deep in the temporal bone. The slightest swelling in this area leads to compression of the fibers and the development of corresponding symptoms.
The pathology most often occurs in middle-aged people, who often neglect preventive measures due to the high pace of life. The peak incidence occurs in the cold season, since low temperatures are one of the provoking factors.
Make an appointment
Psychogenic causes of facial neurosis
Undoubtedly, disturbances in facial sensations quite often become a consequence of pathology of internal organs and blood vessels.
But often they are caused by psychological disorders and pathological thoughts that arise in our heads.
Facial paresthesias can be situational in nature and develop during episodic nervous excitement: as a result of quarrels, prolonged and intense screams. Such phenomena cause overstrain of the muscles, especially the cheeks and those located around the mouth. As a result, we experience facial numbness and even mild soreness.
The feeling of fear causes us to breathe quickly and shallowly, or to hold our breath. Disturbances in the respiratory rhythm can also provoke impressions that are atypical for us. A feeling arises that is characterized as a “chill running through.” Moreover, it is more concentrated at the roots of the hair. In this case they say: “chills to the marrow of the bones.” The face also becomes cold, a slight tingling appears in its area.
Such phenomena are disturbing when we are overwhelmed by strong emotions. But they accompany people suffering from mental disorders systematically.
A special type of neurotic facial manifestations is a nervous tic. It is characterized as an uncontrolled and systematic contraction of the facial muscles.
The disorder more often accompanies men. And it manifests itself with the following symptoms:
1.Motor:
- frequent blinking, winking;
- setting the lips with a tube;
- nodding head;
- constant spitting or sniffing;
- opening or upturning of the corner of the mouth;
- wrinkling of the nose.
2. Vocal:
- screaming;
- grunt;
- coughing;
- repetition of words.
There are also signs – precursors – that signal the appearance of a tic.
These include itching, facial heat and other paresthesias. Naturally, these signs are considered pathological if they occur in an inappropriate situation. It happens that only the patient himself feels them, but they are not visible to others.
But often twitching and other nervous symptoms become noticeable by other people, and they cause a lot of discomfort to the patient.
Tics can be simple, when there is only one symptom, or complex, which combines several manifestations.
The most common, main cause of tics is mental stress. It can be caused by a strong stress factor of one-stage action. Perhaps you were very scared of something, or broke up with your loved one. That is, the shock was so strong for you that your nervous system lost control.
Or, on the contrary, disorders develop as a result of prolonged monotonous exposure. Symptoms often appear due to lack of sleep and overwork.
Their duration varies. A situational nervous tic disappears a few hours or days after the cause is eliminated. In another case, it persists for years or haunts the patient throughout his life. In such a situation, in addition to eliminating the provoking factor, subsequent psychological work with the patient is required. This type of disorder is called chronic.
A nervous tic can be one of the signs of mental disorders such as neurosis, obsessive thoughts and phobias, depression.
Another group of provoking factors include:
- diseases - stroke, brain injury, infections or poisons;
- neurodegenerative diseases - Huntington's chorea. Characterized by destruction of brain tissue. Accompanied by uncoordinated, sudden movements, as well as neurological disorders of the face. Of these, the first sign is slow eye movements. Then a muscle spasm of the face occurs, which manifests itself in grotesque facial expressions - grimacing. Speech, chewing and swallowing are impaired;
- burdened heredity;
- parasitic infestations;
- eye fatigue due to prolonged eye strain;
- unbalanced diet, when the body receives little magnesium, calcium, glycine. These elements participate in the normal conduction of nerve impulses and are responsible for the coordinated functioning of the nervous system.
Causes
Depending on the cause, the following forms of facial nerve neuropathy are distinguished:
- idiopathic: the cause of paralysis remains unidentified (the most common variant of the disease);
- infectious: pathology occurs against the background of infectious damage to nerve fibers due to herpes, tuberculosis, mumps, syphilis and some other diseases;
- otogenic: is a complication of inflammation of the middle ear or mastoid process;
- traumatic: neuropathy develops against the background of traumatic brain injury;
- ischemic: the disease is associated with impaired blood flow and decreased oxygen supply to nerve fibers.
The risk of pathology increases significantly in the following situations:
- for metabolic disorders, including diabetes mellitus;
- with advanced forms of arterial hypertension;
- during pregnancy, especially with severe toxicosis.
The triggering factor for the development of pathology is often hypothermia.
Prerequisites for the occurrence of neuritis
Causes of Bella's Palsy:
- Genetics. One of the reasons for the development of Bella syndrome is a narrow canal of the facial nerve, which is inherited.
- Alcoholism and drug abuse.
- Necrosis of facial tissue due to severe hypothermia.
- Oncology.
- Plastic surgery.
The following prerequisites will help determine the development of pathology:
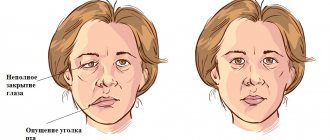
- Noticeable weakening of the facial muscles, inability to control one or another muscle.
- Difficulty closing the eyes completely. This pathology is called lagophthalmos.
- Increased sensitivity to loud noises.
- Dulling of taste buds.
- Unreasonable tearing of the eyes or, conversely, their excessive dryness and redness.
- There is noticeable facial asymmetry.
- Paralysis of parts of the face or individual muscles.
- Swelling of the face.
- Difficulty controlling salivation.
- Jaw dropping.
Paralysis of the facial nerves, or so-called Bella syndrome, is characterized by slow progression, thanks to which it is possible to determine the development of the pathology and take the necessary treatment measures in a timely manner.
Symptoms
Symptoms of facial neuropathy make it possible to immediately suspect the disease. Signs arise from the affected nerve. Patients note:
- acute pain: it usually begins in the ear area and gradually spreads throughout the face and begins to radiate to the occipital region;
- intense lacrimation, less often dry mucous membranes of the eyes;
- discomfort or ringing in the ear due to sharp sounds;
- disturbance of the sense of taste in the anterior parts of the tongue.
As the disease progresses, signs of damage to the motor fibers of the nerve appear:
- smoothness of skin folds, especially nasolabial folds;
- swelling of the cheek when exhaling or trying to pronounce a consonant sound;
- lack of complete closure of the eyelids, rotation of the eyeball upward and outward (lagophthalmos);
- leakage of fluid from the corner of the mouth;
- food getting stuck between the gum and cheek when eating;
- limitation of facial expressions: the patient cannot frown or smile.
If the cause of neuropathy is an infectious process, the characteristic signs are accompanied by symptoms of general intoxication:
- high body temperature;
- headache;
- nausea and vomiting;
- weakness.
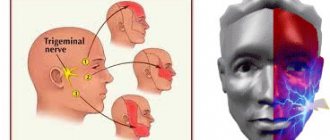
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Diagnostics
Neurological disorders characteristic of facial neuropathy can also occur with other diseases, in particular with stroke. That is why, if any similar symptoms occur, you should urgently consult a neurologist.
Diagnosis of pathology includes:
- collection of complaints;
- taking an anamnesis, during which the doctor clarifies the time and circumstances of the onset of symptoms, records previous and chronic diseases, injuries and other important details;
- neurological examination, during which a specialist checks skin sensitivity, motor function, muscle strength, quality of reflexes, functioning of the central nervous system, etc.;
- tests: general blood and urine analysis, biochemical blood test with mandatory determination of glucose levels, determination of antigens and antibodies to infectious diseases if their presence is suspected;
- X-ray of the chest organs: allows you to diagnose tuberculosis, tumors;
- MRI or CT scan of the brain: helps visualize tumors, areas of acute ischemia, hemorrhages, consequences of injuries and strokes;
- CT scan of the temporal bone;
- electroneuromyography: assessment of the speed of impulse transmission along nerve fibers and muscles, allows you to determine the level of damage and severity of the disease;
- consultations with specialists: therapist, otorhinolaryngologist, endocrinologist, infectious disease specialist, if necessary.
The list of studies can be adjusted depending on the specific clinical situation.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Treatment of facial nerve neuropathy
A combination of drug and non-drug methods is used for treatment. As a rule, doctors prescribe medications from these groups:
- non-steroidal anti-inflammatory drugs (NSAIDs): ibuprofen, meloxicam, nimesulide, diclofenac and other drugs; necessary to relieve pain and inflammation, eliminate swelling; used for mild to moderate neuropathy;
- glucocorticosteroids: prednisolone, hydrocortisone, dexamethasone; have an anti-inflammatory effect, relieve swelling; used for severe forms of the disease, as well as when NSAIDs are ineffective;
- diuretics: furosemide, lasix; necessary to eliminate tissue swelling;
- vascular drugs: pentoxifylline, nicotinic acid, cavinton; stimulate active blood flow in the affected area, improve tissue nutrition;
- metabolic agents: actovegin; necessary to stimulate metabolism and regenerate damaged structures;
- antiviral and antibacterial agents for the infectious nature of the pathology;
- anticholinesterase drugs: neuromidin, axamon; improve the transmission of excitation from nerve to muscle, help to quickly get rid of paralysis of facial muscles;
- B vitamins: milgamma, combilipen; stimulate nerve regeneration and improve impulse conduction.
If neuropathy has become chronic and muscle paresis has given way to spasm, muscle relaxants are prescribed: mydocalm, carbamazepine, baclofen. They replace anticholinesterase drugs and promote muscle relaxation. If these remedies are ineffective, injections based on botulinum toxin are used.
Drug treatment is complemented by physiotherapy. In the acute period the following are used:
- UHF;
- exposure to alternating magnetic field;
- phonophoresis with hormones.
After one and a half to two weeks from the onset of the disease, these methods are added:
- electrotherapy (diadynamic currents, etc.);
- electrical stimulation of muscles;
- electrophoresis;
- magnetic therapy;
- laser therapy;
- Darsonvalization.
An additional effect is provided by mud applications, therapeutic baths, and acupuncture.
During the acute period it is also recommended:
- sleep only on your side (affected side);
- tie a scarf around your face to prevent stretching of paralyzed muscles;
- carry out muscle taping: tighten the muscles using an adhesive plaster (duration from 30-60 minutes to 2-3 hours);
- tilt your head in the direction of the lesion several times a day and support the muscles with your palm; The duration of the procedure is 10-15 minutes.
After acute inflammation has subsided, it is recommended to perform therapeutic exercises to develop the affected muscles:
- frown and raise your eyebrows;
- open and close your eyes wide;
- widen the nostrils;
- puff out one's cheeks;
- smile with your mouth open and closed;
- stretch out your lips, blow out an imaginary candle, whistle;
- stick out tongue, etc.
The more the patient grimaces, the faster the muscles will recover. During the same period, a light therapeutic massage to stimulate blood circulation is acceptable.
If treatment does not bring effect within 2-3 months, doctors recommend using surgical treatment methods. Two types of operations are used:
- restoration of impulse transmission along the nerve: decompression of the nerve fiber when it is compressed in the canal of the temporal bone;
- reinnervation: replacement of the affected area with a donor nerve (segment of the hypoglossal, phrenic or accessory nerve, as well as healthy branches of the facial nerve);
- partial suturing of the eyelids (tarsophasia);
The choice of a specific treatment method depends on the form of the disease, its cause, severity and level of damage.
Make an appointment
Prevention
Compliance with the rules for the prevention of facial nerve neuropathy can reduce the likelihood of pathology occurring. This is especially true if there is an increased risk of developing the disease. Doctors recommend:
- avoid hypothermia and facial injuries;
- observe safety precautions at work to prevent eye damage;
- consult a doctor in time for infections and otitis media;
- control blood sugar levels;
- promptly diagnose and treat chronic diseases.
Complications of the disease
Neuritis of the facial nerve can lead to contracture of the facial muscles. It appears 4-6 weeks after the onset of the disease due to incomplete restoration of the motor functions of the facial muscles. Contracture is a contraction of the muscles of the affected half of the face. At the same time, it seems that it is not the diseased part of the face that is paralyzed, but the healthy one.
To avoid complications of inflammation of the facial nerve, you need to consult a doctor in time. For prevention, we recommend doing facial exercises. You will find examples of exercises at the end of the article.
Treatment at the Energy of Health clinic
Facial nerve neuropathy requires the fastest and most accurate diagnosis and comprehensive, comprehensive treatment. Only in this case can a rapid restoration of impaired functions be achieved. Neurologists at the Energy of Health clinic use the most effective techniques:
- modern drug regimens that affect the cause of the disease and relieve symptoms;
- physiotherapy courses for tissue restoration;
- massotherapy;
- training in facial gymnastics techniques;
- taping the affected areas;
- observation throughout therapy, adjustment of dosages and medications if necessary;
- a full range of measures for quick and complete rehabilitation;
- organization of sanatorium-resort treatment for the most complete recovery.
Surgery
Surgical treatment of facial nerve neuritis is usually carried out to restore its integrity, damaged by injury (rupture of nerve fibers). For this purpose, the nerve is sutured.
In addition, surgery may be performed if the cause of nerve inflammation is compression by a tumor, aneurysm, scar tissue, or other neoplasm. The cause of the compression is removed (an example of such an operation is neurolysis - removal of connective tissue proliferation).
Another type of surgical treatment is replacing the damaged portion of the facial nerve with a graft. Such operations are usually performed for injuries. The section of nerve to be transplanted is taken from the leg. The volume of plastic surgery is determined by the surgical plan. In particular, the transplant can be sutured to the facial nerve on the healthy half of the face. In this case, the signal from the brain will arrive to the facial muscles simultaneously on the right and left sides.
Surgical treatment is indicated in cases where conservative therapy does not bring results. It can be carried out within 12 months from the onset of symptoms of neuritis. Carrying out the operation later does not make sense, since by this time the facial muscles have time to atrophy.
Advantages of the clinic
The Health Energy Clinic provides each visitor with medical care of the highest level, regardless of his age and reason for visiting. We offer:
- screening diagnostic programs to assess health status;
- accurate and quick diagnosis of obvious and hidden pathologies;
- modern methods of drug therapy, physiotherapy, exercise therapy, massage;
- minor surgical operations within the walls of the clinic;
- course treatment of chronic diseases in comfortable day care wards;
- organization of hospitalization in a specialized hospital if necessary;
- preparation of documents for sanatorium-resort treatment, selection of sanatorium;
- remote consultations with foreign doctors to obtain an alternative opinion;
- modern rehabilitation programs.
Facial nerve neuropathy is a fairly common pathology. To prevent it from leading to irreversible facial asymmetry, contact a specialist as soon as possible. Neurologists at the Energy of Health clinic will always come to the rescue.