Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
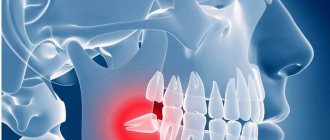
Pericoronitis is a popular dental disease that most often affects the gums of the lower jaw near the wisdom tooth. This is an inflammation of the gingival structures that occurs due to teething. The main thing is not to confuse periodontal disease. As a rule, the pathology occurs in people of older age groups and is accompanied by very unpleasant symptoms.
“Eight” is considered one of the most problematic teeth. Not surprisingly, these teeth appear later than all others, there is little space left for them. Therefore, often the wisdom tooth remains in the jaw without erupting. Sometimes the “figure eight” rests on neighboring teeth and cheeks, grows at an angle and causes a lot of unpleasant sensations.
Causes of pericoronitis
The disease most often results from:
- epithelial injuries due to difficult long-term tooth eruption;
- impacted (formed, but not erupted outward) teeth;
- atypically located tooth roots;
- thickening of the gum mucosa;
- accumulation of soft plaque under the hood and, accordingly, infection of tissues;
- reduction in the size of the dental arch, lack of space for teething;
The catalyst for pericoronitis of wisdom teeth is often a source of infection in the oral cavity. Very often the disease is provoked by caries, stomatitis or periodontitis. Sometimes the disease occurs against the background of ignoring the rules of personal hygiene, prolonged stress, hypovitaminosis and other conditions accompanied by decreased immunity.
Symptoms of tooth pericoronitis
The main clinical manifestations of dental pericoronitis may be the following symptoms:
- swelling of the soft tissue of the gums in the area of the growing tooth;
- redness of soft tissues;
- pain that worsens when eating and brushing teeth;
- pain radiating to the temple, ear or eye socket (on the affected side);
- Difficulty opening the mouth and talking due to pain and swelling;
- bad breath;
- purulent discharge from under the gingival hood;
- increase in body temperature to 37.5 degrees.
If the disease has acquired a serious form, an increase in the submandibular and parotid lymph nodes (on the affected side) is observed, as well as a significant deterioration in the patient’s well-being.
Meanwhile, the most characteristic manifestations of wisdom tooth pericoronitis are:
- swelling of the gums;
- redness of the gums;
- pain in the gum area.
Often, with acute pericoronitis, the swelling is so severe that the patient has difficulty speaking and it becomes difficult to open and close his mouth.
Specialist help
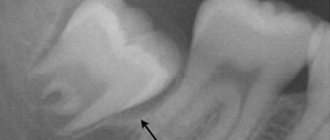
In case of inflammation of the gingival tissues around the eights, the best solution is to immediately visit a dentist. The specialist will conduct an x-ray and a visual examination of the condition of the tooth and the surrounding area. Based on the examination results, competent treatment will be prescribed:
- Medication - by prescribing antihistamines and anti-inflammatory drugs, antibiotics, special ointments and gels, antiseptic baths.
- Surgical - cutting the gum or gingival hood, removing the figure eight that caused the problem.
If inflammation is accompanied by unbearable acute pain and severe swelling of the gums, a specialist performs a novocaine blockade. Sometimes laser therapy is prescribed, which has an anti-inflammatory effect on the affected area.
Types of pericoronitis
Depending on the complexity and localization of inflammation, pericoronitis is divided into:
- Spicy.
The initial stage of the disease, which is characterized by pain, hyperemia and swelling of the gums. In case of acute pericoronitis of a wisdom tooth, there is no purulent discharge and the general condition of the patient does not suffer. With proper timely treatment, this type of disease disappears in 3-5 days.
- Ulcerative.
The disease develops against the background of epithelium damaged by fusospirochetes. A characteristic symptom of ulcerative pericoronitis is the appearance of a necrotic rim along the edges of the gums. Small ulcers form on the mucous membrane. When plaque is removed from the gum surface, bleeding begins.
- Purulent
Pericoronitis, as a rule, occurs in a subacute form and is manifested by severe pain. Pus is released from the source of inflammation, and the temperature rises. In the absence of timely treatment, the disease can provoke the formation of abscesses, phlegmon and periostitis.
- Posteriormolar.
The disease develops when molars erupt incorrectly. A gingival hood forms, which then becomes infected due to the active proliferation of bacteria.
Infectious and inflammatory processes, caries
The hygiene of wisdom teeth is complicated by their inaccessibility, so they are prone to various dental diseases. Due to incomplete eruption, specific structure and prolonged germination, eights are predisposed to various painful conditions:
- Caries is a common disease that also occurs in impacted eights. Very often, wisdom teeth erupt with signs of crown destruction, even if they have been under the gum tissue for a long time.
- Complications of caries - periodontal cyst, pulpitis, periodontitis.
- Acute purulent-inflammatory processes - fistula, flux and abscess.
Treatment of pericoronitis
Treatment by a dentist and surgeon should be aimed not only at eliminating the symptoms of the disease, but also at eliminating its causes. As a rule, for wisdom tooth pericoronitis, drug therapy and surgical intervention are used.
Drug treatment is the fight against microorganisms that caused the development of the infectious process. The doctor also prescribes medications that reduce pain and inflammation symptoms.
As a rule, the following groups of drugs are used to treat wisdom tooth pericoronitis:
- antiseptics, mouth rinses. The products reduce the microbial load and wash away bacterial and purulent particles.
- nonsteroidal anti-inflammatory drugs, for example, Ibuprofen, Ketorolac.
- antimicrobial, broad-spectrum anti-inflammatory drugs, for example, Amoxicillin, Amoxiclav, Azithromycin.
Surgical intervention for wisdom tooth pericoronitis usually involves excision (removal) of the gum hood over the wisdom tooth. This tactic is chosen in case of frequent relapses of the disease, pronounced pain syndrome, and spread of the purulent process to surrounding tissues. When an area of soft tissue is excised above the surface of the crown, plaque stops accumulating, which prevents infection and progression of the disease.
Excision of the hood takes no more than 10-15 minutes and is performed under local anesthesia.
If removing the hood and conservative treatment does not lead to an improvement in the condition, it is possible to remove the wisdom tooth. Removal is also carried out in case of incorrect tooth position or significant deviation of the “figure eight” from its physiological axis. In rare cases, not only the wisdom tooth is removed, but also part of the bone tissue. After removal, in almost 100% of cases, the patient recovers completely.
It is worth noting that many patients often insist on maintaining the “eight”. Many believe that in the future a wisdom tooth may be useful if prosthetics are needed. However, such an opinion is wrong. The wisdom tooth is located the farthest away and does not bear a significant functional load, taking only 2% of the total load on the dentition. When installing a crown, the wisdom tooth will not withstand the pressure, and the prosthesis will have to be replaced very soon.
If the gums are swollen due to periodontitis -
No less often, complaints that the gums around the tooth are swollen are associated with the patient having an inflammatory gum disease, which is called periodontitis. With periodontitis, there is destruction of the attachment of the gingival margin to the necks of the teeth, destruction of the bone tissue around the teeth, as well as periodontal fibers, due to which the tooth is attached to the bone tissue. As a result of these processes, periodontal pockets are formed between the gum and tooth (Fig. 14).
There are a lot of pathogenic bacteria in such pockets, and therefore serous-purulent exudate is always released from them. When the pocket becomes deep enough (more than 4 mm), the drainage of exudate from the gum pocket may be disrupted, which leads to the formation of a purulent abscess in the depths of the pocket. Dentists usually use the term periodontal abscess in this case (Fig. 15-16).
Swelling of the gums in the projection of the periodontal pocket –
Why gums swell during periodontitis: reasons
Periodontitis can be local and generalized. Local periodontitis differs in that it occurs only in one or several teeth exposed to a traumatic factor. For example, the formation of a periodontal pocket can be caused by trauma to the gums due to the overhanging edge of a filling in the interdental space, or by an incorrectly made crown or removable denture. Also very often the cause is traumatic occlusion, when some teeth are subjected to increased chewing load (for example, due to the loss of part of the chewing teeth).
If the teeth that have swelling on the gums do not have fillings or crowns, and you do not have long-term chronic inflammation of the gums, then you can immediately say that the reason is the presence of premature closure of the teeth in this area of the dentition. As a result, an increased mechanical load is placed on the tooth, which leads to the onset of destruction of the bone around the tooth and the formation of a periodontal pocket (24stoma.ru).
But in chronic generalized periodontitis, the causes of gum swelling are completely different. You can immediately suspect this form of periodontitis if you periodically experience bleeding when brushing your teeth, there is constant low-grade inflammation of the gingival margin in the area of all teeth (which is accompanied by swelling of the gingival papillae, their redness or cyanosis). The cause of this form of periodontitis is the accumulation of soft microbial plaque on the teeth, as well as hard dental deposits.
Microbial plaque and tartar bacteria produce toxins that destroy the dental-gingival attachment and bone tissue around the teeth, and also destroy the periodontal attachment of the tooth to the bone. With this form of periodontitis, periodontal pockets can be found in almost all teeth, and not 1-2 teeth as in the local form of periodontitis. When the discharge of serous-purulent discharge in one of the pockets is disrupted, a periodontal abscess is formed in the projection of the pocket.
Symptoms - if periodontitis, swelling of the gums occurs mainly in the projection of the apex of the tooth root or the bone interradicular septum, then with periodontitis the gums always swell in the projection of the formed periodontal pocket. Sometimes you may notice that thick pus spontaneously secretes from under the gums in the area of swelling, or it may appear when you gently press on the swelling (such symptoms clearly indicate that the cause is periodontitis, not periodontitis).
Also, the fact that the cause was local or generalized periodontitis can be indicated by the presence of mobility of the causative tooth, especially if mobility was present even before the swelling appeared. Let's now figure out what to do if the gums are swollen due to periodontitis... Treatment of the local and generalized forms of this disease will differ, because their development is caused by various reasons.
Treatment of local periodontitis –
When you see a doctor, the doctor, based on an examination and analysis of an x-ray, will determine the presence of a periodontal abscess and the amount of tissue destruction around the tooth (the depth of the periodontal pocket). Treatment immediately begins with eliminating the traumatic factor - removing the overhanging edge of the filling, grinding the contacts on the chewing surface of the causative tooth. At the same time, under anesthesia, the periodontal abscess is opened to allow the pus to drain out.
Next, the pocket is washed with antiseptics, systemic antibiotic therapy is prescribed, as well as a home course of anti-inflammatory therapy, consisting of antiseptic rinses and treatment of the gums with an anti-inflammatory gel. At the same time, the issue of the need to depulpate the tooth can be resolved, i.e. removal of the nerve and filling of the root canals (this is necessary if the depth of the periodontal pocket reaches more than 1/2 the length of the tooth root).
Removal of the nerve in such a situation is required because infection from a deep pocket can penetrate through the bloodstream into the tooth pulp (through the apexes of the roots). And then in this case, the tooth pulp itself becomes a source of infection. But this is all just basic treatment! The main treatment will be an open curettage operation of the periodontal pocket, which will remove the inflammatory granulation tissue from under the gums that has formed at the site of the destroyed bone, as well as fill the pocket with special bone material, which will partially restore the level of inert tissue.
Progress of open curettage operation –
Please note that in the first stage of the operation, the gums are peeled off from several teeth to create good access to the periodontal pocket. In the photo above you can see a deep periodontal pocket between the canine and lateral incisor (at this point all inflammatory granulations have already been cleared from the pocket). Next, the pocket is filled with bone material, which can also be covered on top with a special membrane, after which the gum is returned to its place and sutures are applied. Please note that an x-ray 5 months after the operation shows an increase in bone tissue level of about 2.5-3 mm.
In addition, if a tooth is mobile, it may be necessary to splint it with adjacent teeth using fiberglass and filling material. You can read more about these treatment methods in the articles linked below:
→ Open gum curettage operation, → Teeth splinting technique
Treatment of generalized periodontitis –
In the generalized form of periodontitis, periodontal pockets occur not in just a few teeth, but in almost all teeth. Such periodontitis usually has a chronic course with sluggish symptoms, usually manifested by bleeding and soreness of the gums when brushing, and swelling of the gingival margin. Periodically, an exacerbation of inflammation may occur, and then abscess formation may occur in the area of one or more periodontal pockets (i.e., the formation of a purulent periodontal abscess).
Treatment of the generalized form of periodontitis is very complex, and therefore a separate article is devoted to this problem on our website, which you can read at the link above. But the main stages of treatment in this case will be removal of dental plaque and anti-inflammatory therapy, after which splinting of mobile teeth and/or gum curettage can be additionally applied.
Rinse
Special rinses will help relieve pain and swelling at home. However, such treatment is symptomatic. If inflammation progresses, in no case should you limit yourself to rinsing only.
The treatment for inflammation recommended by dentists is ASEPTA Active mouth rinse. This unique two-component product with a combination of “chlorhexidine + benzydamine” has an antimicrobial, anti-inflammatory effect and provides an immediate analgesic effect.
To eliminate inflammation and relieve discomfort during wisdom tooth pericoronitis, it is possible to use such medicinal herbs as:
- chamomile;
- sage;
- calendula.
Traditional medicine methods
Folk remedies can be auxiliary methods for eliminating inflammation in the early stages. At the initial stages they are able to give excellent results. There are herbs, decoctions and infusions of which can have anti-inflammatory, disinfectant, wound healing and antimicrobial effects. To get such a decoction, you need to pour a teaspoon of beneficial herbs with a glass of boiling water and let it brew. Next, the resulting substance is filtered and the inflamed area is rinsed 4-6 times a day. Healing plants in this situation are chamomile, lemon balm, oak bark, calendula, sage and St. John's wort. A weak soda-salt solution can also have an anti-inflammatory effect. You need to rinse your mouth with it three to five times a day.
Possible consequences
Pericoronitis of the wisdom tooth in the lower jaw is a rather dangerous disease, ignoring which can lead to very unpleasant consequences.
Possible complications of the disease may be:
- abscesses, phlegmon of the vestibule of the mouth, buccal area;
- periostitis;
- osteomyelitis of the jaw;
- periodontitis;
- ulcerative stomatitis;
- actinomycosis;
- paradental cysts.
In addition, if wisdom tooth pericoronitis affects the lymph nodes, if inflammation develops, the lymphatic system may become a victim of infection.
And, of course, without proper treatment, the disease can become chronic and periodically “harass” the patient with unpleasant symptoms. Inflammation can spread to neighboring healthy teeth. Therefore, in order to avoid complications, treatment of the disease should be carried out as early as possible.
Complications of the disease
In the case when treatment of the gums during complicated tooth eruption was not carried out, serious complications of the inflammatory process develop:
- Periostitis, or flux, is inflammation of the periosteum.
- Osteomyelitis - in this disease, inflammation affects both the bone tissue itself and the bone marrow, gradually leading to bone resorption. This can cause abnormal jaw fractures.
- An abscess when the infection spreads to nearby tissues. Purulent inflammation leads to the melting of muscles and fatty tissues with the formation of a large accumulation of pus.
- Cellulitis is the next stage of a purulent process after an abscess, which does not have clear boundaries. Such purulent inflammation is a serious threat to the patient and is treated in a maxillofacial hospital.
These complications are usually difficult to treat, require a serious systemic approach and can lead to irreversible consequences. Therefore, if a person suspects he has pericoronitis, treatment should begin without delay in order to prevent the condition from worsening. You need to be especially careful if gum inflammation occurs during teething in children, since the children's immune system is still immature, the body's resistance to infections is lower and the process quickly becomes more severe.
Prevention
As you know, it is easier to prevent a disease than to treat it. The main disease prevention measures are:
- annual dental examinations;
- timely diagnosis and treatment of impacted molars;
- maintaining oral hygiene;
- timely treatment of caries, gingivitis, periodontitis and other dental diseases;
- Regular (once every six months) professional teeth cleaning in a dental clinic.
Remember: pericoronitis without proper treatment can cause very serious complications. Therefore, if you suspect inflammation, do not delay your visit to the dentist. The doctor will help you cope with unpleasant sensations in a matter of days and prevent the development of the disease.
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
- The use of drugs from the Asepta line in the complex treatment of inflammatory periodontal diseases (N.V. Berezina E.N. Silantyeva S.M. Krivonos, Kazan State Medical Academy. Kazan.) N.V. BEREZINA, E.N. SILANTIEVA, S.M. KRIVONOS Kazan State Medical Academy