From this article you will learn:
- why is the gum around the tooth swollen,
- The gum is swollen and hurts - what to do.
The article was written by a dental surgeon with more than 19 years of experience.
If your gums are swollen, what to do in this case will depend on the cause of the inflammation. There may be two main reasons. The first reason is associated with the development of periodontitis, i.e. inflammation at the apex of the tooth root (Fig. 1-3). The development of inflammation is associated here either with poor-quality dental treatment in the past, or with the lack of timely treatment. And in this case, you can always find a carious defect, filling or crown on the causative tooth.
The second reason that the gums are swollen and painful may be the development of localized or generalized forms of periodontitis in the patient. With these forms of gum inflammation, the attachment of the gingival margin to the neck of the teeth is destroyed - with the formation of so-called “periodontal pockets” between the gum and teeth (Fig. 4-6). In such gum pockets, good conditions are created for the growth of bacteria, which can also lead to the development of purulent inflammation in the gum pocket and the appearance of gum swelling.
Swelling of the gums due to periodontitis –
Swelling of the gums due to periodontitis -
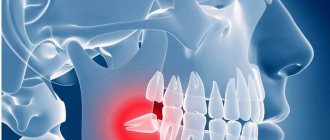
A separate question in this article is what to do if the gums near the wisdom tooth are swollen. Most often this occurs in the lower jaw, and in this case the swelling of the gums is not associated with either periodontitis or periodontitis. This inflammation of the gums is called a special term - pericoronitis (which means inflammation of the “hood” over the wisdom tooth).
Etiology and pathogenesis
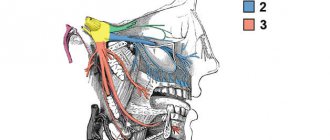
The development of periostitis most often occurs with inflammatory diseases of the oral cavity and teeth, pulpitis and periodontitis. Also, the development of purulent inflammation of the periosteum can occur after jaw fractures, injuries and wounds of the soft tissues of the cheek, after treatment with anesthesia. Through damage to the dental tissue, gums or cheeks, the pathogen enters the jawbone, causing inflammation.
Acute periostitis can develop as a result of acute or chronic periodontitis, with suppuration of odontogenic cysts, and difficulty in teething. The process begins with the inner layer of the periosteum, gradually spreading to all other layers. Periostitis occurs when the focus of primary infection of the tooth canal or gum is blocked and its contents penetrate into the periosteum. The exudate penetrates through small holes in the alveolar plate through the channels.
Less commonly, flux develops in diseases of the pharynx (sore throat, pharyngitis, laryngotracheitis) or in the presence of a focus of infection in the body, from where it can be transferred to the periosteum with the blood or lymph flow.
When examining purulent contents during purulent periostitis, staphylococci (Staphylococcus aureus is one of the main causes of flux development), streptococci, various types of bacilli and putrefactive bacteria are often found.
Reference! 25% of all pathogenic microflora during flux are aerobic bacteria, the rest is anaerobic forms.
General factors influencing the development of the disease:
- weak immunity;
- hypothermia;
- stressful situations;
- poor oral hygiene;
- carious processes in teeth;
- old fillings;
- frequent medical interventions;
- bad habits.
Forms of periostitis
Depending on the cause of the flux and its course, we talk about its forms:
- Acute: simple – occurs as a result of a bruise of the face, with fractures and injuries of the jaw bones;
- purulent – penetration of periodontal infection to the periosteum;
- tuberculosis - when Koch's bacillus is carried into the periosteum and bone tuberculosis;
- syphilitic - as a complication of congenital or acquired syphilis.
- ossifying – chronic form with the development of compactions in the form of bone tissue;
First aid for swollen gums
Under no circumstances should a heating pad be applied to an inflamed gum! This is dangerous due to the rapid spread of infection and the development of complications.
To “live until the morning” when you can go to the doctor, you can take several actions that can alleviate the condition:
- apply cold to the sore side - this will constrict the blood vessels and temporarily relieve the fever;
- take an analgesic - but only while you sleep at night; in the morning you need to come to the doctor without pain relief, so as not to erase the picture of the disease;
- drink an antipyretic - if a high temperature prevents you from falling asleep, you can bring it down, but don’t forget to mention it in the morning at the doctor’s office;
- rinse your mouth with an antiseptic - this will slightly slow down the spread of inflammation;
- use a spray with lidocaine on the painful area - this will temporarily relieve the pain.
All of the above measures can only be used as temporary measures. Only a doctor can prescribe adequate treatment after an in-person examination.
Clinical picture
The main symptom for all types of flux is severe toothache at the site of infection, sometimes diffuse (with extensive bone damage). Swelling gradually begins to increase: first it is localized above the site of inflammation, and then along the surrounding tissues, sometimes affecting the neck, temple and eye.
Important! Sometimes flux occurs painlessly or with a mild pain effect, which, as a rule, indicates the development of a chronic form with sluggish inflammation and periodic relapses.
Inflammation is accompanied by the following symptoms:
- pulsation at the site of the lesion;
- increase in body temperature to subfebrile and febrile levels;
- headache;
- enlarged lymph nodes on the affected side;
- weakness, lethargy, lack of appetite;
- pain when swallowing, talking, opening the mouth;
- pain when pressing on the gum;
- redness of the oral mucosa at the site of the lesion.
When gums are inflamed and even your cheeks hurt
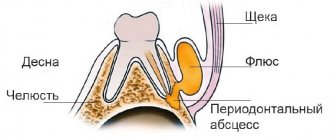
Sometimes the gums not only swell, but a new growth becomes noticeable on it. It is often pale in color due to the presence of pus inside. This is what a periodontal abscess looks like:
- the surface of the neoplasm is elastic and tense;
- swollen tissue around the abscess;
- the palate and cheek swell;
- sometimes the general body temperature rises, more often local;
- swollen tissues of bright red color;
- fluid movement is felt inside the abscess.
This disease is often called "flux". It has a rather characteristic picture. An abscess develops due to lack of treatment for periodontitis: suppuration appears that cannot come out. “Flux” is accompanied by very severe pain and swelling.
Treatment of an abscess is carried out only surgically and in a hospital setting. Attempts to cure flux at home with lotions or self-opening can result in phlegmon, sepsis and, in rare cases, even death. In the best case scenario, the patient will receive major surgery with pus removed through large incisions in the face instead of a small hole in the gum. Therefore, you should not delay visiting the dentist.
Therapy and rehabilitation
Treatment of the disease is carried out by two methods - conservative and surgical. The choice of method depends on the form of the disease, its severity, and the course of the disease. In the early stages of development of the pathological process, conservative treatment is possible by prescribing a complex of drugs:
- broad spectrum antibiotics
- anti-inflammatory;
- painkillers;
- antipyretic.
IMPORTANT! Conservative treatment requires careful compliance with all doctor’s instructions until the process is completely eliminated. Otherwise, there is a risk of the disease becoming chronic.
Purulent periostitis is treated by wide opening of the purulent sac with dissection of the periosteum to the bone. At the same time, the issue of treating the tooth that caused the inflammatory process is being resolved. Most often, such a tooth is removed. After removing the pus, medications are prescribed, including antibiotics, anti-inflammatory and painkillers. Additionally, physical therapy may be prescribed: UHF, microwaves. The patient is recommended to frequently rinse the mouth with a solution of baking soda or sage tincture.
Simple periostitis requires complete rest of the injured area and treatment with physiotherapeutic procedures. All other types are reduced to treating the underlying disease or eliminating the focus of fibrous tissue growth.
IMPORTANT! Under no circumstances should you treat flux yourself. It is especially not recommended to pierce a purulent sac: there is a high risk of infection in neighboring tissues.
To speed up the treatment and recovery processes, you can resort to traditional medicine methods.
Pathology in tooth eruption
Usually in adults this problem is caused by wisdom teeth. however, nothing can be stated unequivocally; in each case, the problem is solved individually. For example, let’s look at wisdom teeth and the pathology of their eruption. The wisdom tooth begins to hurt as soon as it begins to “peck”. It moves nearby teeth and often grows in the wrong direction. Usually we drink painkillers and then go about our business. But the problem remains unresolved. The tooth continues to grow, begins to violate the integrity of the mucous membrane and forms a “pocket” in it, into which food debris gets trapped. These residues naturally begin to rot under the gums. And the pain becomes much more serious and acute. In this case, urgent medical intervention is necessary. The dentist will clean the wound and install a drainage gum so that it ensures the outflow of infiltrate. You may need to take antibiotics for some time to speed up recovery. After the situation has stabilized, the unfortunate wisdom tooth is removed. This is not done right away, because you had an active focus of inflammation in the gum, and the removal of a wisdom tooth could provoke infection into deeper tissues, which means the spread of this inflammation to the entire jaw. Such inflammation will be much more dangerous and more difficult to treat. Therefore, the treatment will be carried out in stages and will take you some time.
Prevention
Flux is easier to prevent than to treat. Prevention methods are simple and known to almost everyone. They consist of timely treatment of carious teeth, timely removal of the gum hood from wisdom teeth, the correct choice of toothbrush and toothpaste, and timely replacement of oral hygiene products. It is recommended that you visit your dentist at least twice a year and have your teeth professionally deep cleaned to remove plaque at least once a year.
IMPORTANT! Don’t forget about strengthening your immune system and giving up bad habits.
Dental flux is an unpleasant disease that requires treatment by specialists at an early stage of development. Self-medication in case of periostitis is unacceptable. With a favorable course and initial stage of development, conservative treatment is possible, but most often they resort to the surgical method.
How to treat swollen gums
Treatment of inflamed gums begins with identifying the cause of the disease. To do this, an X-ray of the jaw and an examination of the oral cavity are performed.
Further tactics depend on the established diagnosis. If surgical intervention is necessary (opening an abscess, removing a cyst), it is performed immediately. The patient is anesthetized in the dentist's chair, and then all necessary manipulations are performed.
After surgical treatment, maintenance drug therapy is prescribed. It allows you to avoid the development of complications. Most often, the patient is prescribed rinsing with an antiseptic solution and taking anti-inflammatory drugs. Antibiotics are sometimes recommended to prevent bacterial complications. They should be taken only as prescribed by a doctor, and exactly the drug that is indicated in the prescription. This is important to achieve a guaranteed positive effect.
Some drugs do not combine with each other. Therefore, uncontrolled use of medications can harm the patient himself. If you choose the wrong antibiotic, the bacteria will not only not die, but will also develop resistance to the drug. Then it will take a long time to select a suitable remedy, which will complicate the patient’s life - it will no longer be possible to quickly get rid of unpleasant symptoms.
Rinse recipes
The patient's attending physician should prescribe rinses. They are not allowed for all diseases. After surgical treatment, rinsing too hard can cause the suture to come apart. An infection or food particles will get into an open wound, which will cause new inflammation and suppuration.
It is impossible to completely cure swollen gums with rinses. But they are advised to be combined with drug treatments to alleviate the condition and enhance the effect of the drugs.
- Decoctions of medicinal herbs: chamomile, calendula, lemon balm, sage, St. John's wort. Some components can cause allergies, so you need to be careful with them. However, they have a mild anti-inflammatory effect and can help relieve swelling and reduce inflammation.
- Propolis tincture - dilute it with warm water and rinse your mouth 2 times a day. The product helps against ENT diseases (sore throat and sinusitis), which often develop into inflammation of the gums.
- Soda and salt - add 1 teaspoon of each powder to a glass of warm water and stir. The product has a wound healing effect and helps stop bleeding gums.
In addition to rinsing, lubricating the area of inflammation with tea tree or fir oil is also effective. They have an anti-inflammatory and wound-healing effect. However, they should not be applied to the site of suppuration. It is also worth considering the risk of plant allergies.
There are many reasons for gum swelling, not all of them are obvious. Only a doctor after diagnosis can figure out what caused the inflammation. Independent attempts to cure the disease often lead to serious complications, so you should not expect that the swelling on the gums will go away on its own. It is better to visit a doctor and make sure there are no risks or get competent and timely treatment.
Content:
- Why does the gum around the wisdom tooth hurt? 1.1. Pain due to wisdom tooth cutting 1.2. Pericoronitis as a cause of pain 1.3. Dental neck caries 1.4. Other reasons
- Signs of inflammation
- What to do at home
- Treatment
- How to avoid inflammation
If your gums near your wisdom tooth hurt, you need to visit a dentist and undergo a prescribed examination. Self-medication for painful symptoms is usually ineffective, since it is not possible to establish the true cause of the disorder. Consequently, all measures taken will be aimed exclusively at relieving the unpleasant symptom.