From this article you will learn:
- what is dental pulp and its functions,
- structure and architectonics of pulp layers,
- histological preparations.
Dental pulp (pulpa dentis) is a specialized type of loose fibrous connective tissue rich in blood vessels and nerve fibers that fills the cavity of the tooth, i.e. pulp chamber and root canals. Due to the presence of a large number of receptor nerve endings in it, the pulp provides very high pain sensitivity of tooth tissue to the effects of mechanical, physical, and chemical stimuli.
Inflammation of the pulp (pulpitis) most often develops as a result of pathogenic bacteria entering it. This occurs when the carious process spreads to the deep layers of dentin surrounding the pulp chamber, but in some cases the cause of inflammation can be physical trauma to the tooth or a thermal burn (for example, due to errors when preparing a tooth for a crown). Most often, pulp inflammation occurs acutely, with severe pain, but in some cases the course can be asymptomatic - with a predominance of hyperplastic processes.
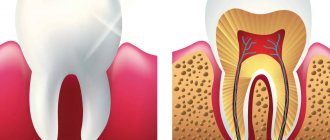
Structure of the dental pulp (diagram) –
Due to the abundance of blood vessels in the pulp, as well as due to the presence of narrow apical openings at the apexes of the roots, with the development of acute pulpitis, inflammatory edema always increases rapidly. Since the volume of the pulp is limited by the walls of the pulp chamber, inflammatory edema leads to compression of the veins and lymphatic vessels, thereby disrupting the outflow of fluid. This leads to the development of necrosis and death of the pulp. In addition, swelling also leads to compression of nerve endings, which actually causes the development of acute pain.
It should be noted that the dental pulp contains entire nerve plexuses, including a large number of receptors that are capable of perceiving stimuli of any kind - pressure, temperature, chemical and physical influences. But at the same time, effector nerve endings are also described in the pulp. Part of the nerve fibers of the pulp (together with the processes of odontoblasts) exits it into the predentin and the inner zone of the peripulpal dentin, located in the dentinal tubules.
What does dental pulp consist of?
Anatomical structure of the dental pulp
From an anatomical point of view, the tissue is divided into two zones. The coronal dental pulp has a loose structure and is involved in dentinogenesis; all layers of the dental pulp in this part are penetrated by an extensive network of capillaries and nerve cells. The root pulp of a tooth is denser because it does not contain a large number of cellular elements, but is saturated with collagen fibers. Through the apical foramen, the canals communicate with the periodontal tissues and allow minerals and nutrients to reach the tooth walls.
The pulp and dentin of the tooth form a strong complex - the hard tissue protects the tooth pulp from external irritants, and it, in turn, helps the formation of dentin.
The pulp of the front tooth smoothly passes from the crown to the root part, the dental pulp of the molars has clear boundaries - the mouths of the dental canals.
Histological structure of dental pulp
The pulp contains a large number of different elements:
- Elastin and collagen fibers supply the organ with hyaluronic acid, reducing susceptibility to toxins and bacteria.
- Odontoblasts and stellate cells are responsible for the regeneration of dental pulp.
- Leukocytes, lymphocytes and fibroblasts support the vital activity of the epithelium and organize communication between cells.
- A branched network of nerve processes forms Rashkov's plexus and provokes the occurrence of pain sensitivity when exposed to stimuli - the innervation of the dental pulp occurs due to the trigeminal nerve.
- Vessels and capillaries provide the blood supply to the dental pulp, which is necessary to nourish the tissues.
Composition of dental pulp
The fabric is 74% water, the remainder being organic and inorganic layers. Pulp cells include protein compounds, acids, lipids, glucose and various enzymes, which allows the epithelium to actively consume and process oxygen.
Many people mistakenly believe that the pulp is a nerve. The opinion is incorrect, since in addition to nerve plexuses, the tissue contains blood vessels and collagen fibers. |
Structure and cellular composition
The structure includes several separate parts - the coronal, root and apical foramen. The vascular network is developed, including segments of small arterioles with a very thin wall, which gradually transform into capillaries. It also includes vascular and nerve bundles that perform the functions of nutrition and transmission of sensory signals.
General composition:
- vault of the pulp chamber (the shape depends on the type of tooth and its location in the row);
- horn and pulp chamber in the middle part;
- the bottom from which the lateral and periodontal canals extend;
- ostium (the opening through which blood vessels and nerve bundles exit);
- hole at the top of the tooth root.
The structure of the pulp includes the following layers:
- peripheral (layer with dentinobalsts and immature collagen fibers, cells are pear-shaped, special-purpose processes);
- intermediate, including pre-collagen fibers and pre-dentinoblasts, also includes a cell-free zone;
- the central loose part with nerve plexuses and vessels, including lymphocytes, macrophages, fibroblasts, histiocytes, plasma cells and mast cells.
Age-related changes in dental pulp
The pulp of temporary and permanent teeth has a similar structure and only becomes thinner over time. Before the roots are formed, the pulp of a baby tooth is concentrated in the coronal part. Later, the tissue begins to spread into the dental canals through the apical foramen and grow into a wide network. The dental pulp in a child has a massive and dense structure, as well as a large fiber size.
The development of dental pulp continues throughout life, but with age, regeneration processes slow down: the number of active cells decreases, which leads to vascular fragility, insufficient tissue nutrition, the tooth suffers from odontoblast atrophy, that is, the impossibility of dentin formation. The described changes apply to older people.
Complications: pain of a pulpless tooth
After removing the pulp, followed by filling the canals and restoring the crown of the tooth, the patient may still experience pain, especially when biting. If pain goes away within a week, this is normal. If the pain continues to bother you after 5-7 days, this may indicate poor quality treatment and/or filling. For example, the filling material was carried beyond the root apex and got into the soft tissues, or during the removal of pathologically affected tissues, the tooth root was accidentally damaged, or the patient is allergic to filling materials. Also, if the treatment and/or filling of the dental canals is not thorough enough, pulpitis can turn into periodontitis.
Functions of the dental pulp
The main role of the pulp is to perform several tasks to support the vital functions of the tooth.
- Plastic function.
Formation of basic dentin, as well as the formation of hard tissue in case of damage. - Protective function.
Preventing infections from entering the periodontium through canals, removing dead cells, maintaining regeneration processes. - Sensory function.
A signal about the presence of an external or internal irritant to preserve tooth health. - Trophic function.
Supply of nutrients to dentin and tooth enamel.
Dentin diseases
Very often, the bone substance of the tooth is susceptible to a disease such as caries. When damage affects only enamel and dentin, the disease is classified as moderate. The process begins with damage to the surface layers of tissue, then a carious cavity is formed in which food debris accumulates, which provokes the onset of decay processes and further destruction of the tooth. A diseased tooth causes significant discomfort, reacting with acute pain to various irritants, but after their elimination, the pain stops. These signs should be a signal to visit the dental clinic as soon as possible and fix the problem. Otherwise, caries can reach the root of the tooth in a fairly short period of time. When the root is damaged, a deep form of caries occurs, in which there is a high risk of losing the tooth. In order to keep your teeth healthy for as long as possible, you must observe the following: 1. Perform regular high-quality oral hygiene. 2. Have healthy foods in your diet, enriched with vitamins and minerals. 3. Regularly undergo preventive examinations by a dentist to identify diseases at an early stage in order to prevent further destruction of dental tissues
What can cause pulpitis?
Burn of tooth pulp
As a rule, a pulp burn during tooth grinding occurs as a result of medical error or carelessness. Before prosthetics, the crown part is treated at high temperatures. Insufficient cooling during the preparation process can lead to a burn, which will provoke subsequent inflammation of the dental pulp.
Dental pulp hematoma
After a tooth injury, there is a possibility of getting a hematoma, that is, bleeding into the dentin. The crown acquires a reddish tint and painful sensations occur when pressure is applied. However, a bruise that has not turned into pulpitis or necrosis does not need treatment and goes away on its own over time.
Caries
Through the smallest cracks in the tooth cavity, infection and pathogenic bacteria penetrate into the pulp. Advanced caries is one of the most common causes of pulpitis.
Any damage or complications of diseases can lead to disastrous consequences if left untreated. Dental pulp necrosis is the process of tissue death due to the spread of infected cells. The anomaly can be recognized by the grayish color of the tooth and incessant aching pain. During treatment, the doctor will perform depulpation, clean and seal the canals. |
Types of pulpitis
Today, the main classification that defines diseases, including pulpitis, and its types, is the International Classification of Diseases and Related Health Problems, developed by the World Health Organization, tenth revision (ICD-10). Also considered an authoritative classification among Russian dentists is the MMSI, developed in 1989 at the Research Institute named after. N. A. Semashko.1
According to the clinically and legally accepted international classification ICD-10, pulpitis (K04.0) as a disease is divided into several types, but this classification has some discrepancies with the classification according to MMSI:
K04.00 – initial (pulp hyperemia) / according to MMSI – deep caries
K04.01 – acute / according to MMSI – acute focal pulpitis . Acute pulpitis is a common complication of deep caries and is characterized by severe pain, aggravated by impact on the tooth. According to the MMSI classification, the first stage of acute pulpitis is focal pulpitis, lasting no more than 2 days. Due to the proximity of the carious cavity to the pulp, a sharp “shooting” short-term (10-30 minutes) pain of a spontaneous and cyclical nature occurs: it arises arbitrarily, without affecting the tooth, and also disappears arbitrarily, only to reappear after some time. It “envelops” one tooth without spreading to adjacent teeth and tissues.
K04.02 – purulent (pulp abscess) / according to MMSI – acute diffuse pulpitis . This is the next stage of the disease, when inflammation spreads to the root part of the pulp. The pain becomes radiating - spreading along the branches of the trigeminal nerve, “radiating” to the area of other teeth, to different parts of the jaw, to the cheekbones, to the temples, to the back of the head, to the ears, its attacks become more frequent (especially at night), and the intervals between them become shorter (30-40 minutes) – diffuse pulpitis. If the patient notes that hot food and drink increase pain, and cold food and drinks relieve pain, this often indicates that the purulent stage of pulpitis or a pulpal abscess has occurred. This stage lasts maximum 14 days, after which pulpitis enters the chronic stage.
K04.03 - chronic / according to MMSI - chronic fibrous pulpitis : this is a long-term inflammatory process that lasts from 2-3 weeks to several years. Toothache at this stage becomes less pronounced, “dulls”, worsening during chewing, bleeding of the pulp and fragility of the hard tissues of the tooth may appear. This also correlates with the first stage of chronic pulpitis according to the MMSI classification - fibrous pulpitis, which often occurs secretly, without showing itself or is signaled by mild discomfort and pain. When examined at this stage, a large carious cavity is almost always discovered, which in many cases is connected to the pulp chamber. The pulp is painless, pain appears only when you touch it, and minor bleeding is possible.
K04.04 - chronic ulcerative / according to MMSI - chronic gangrenous pulpitis . This stage of the development of the disease is characterized by atrophy of the nerve fibers of the pulp, a change in its color to dirty gray, increased pain, and the appearance of bad breath. The examination also reveals an extensive and deep carious cavity.
K04.05 – pulp polyp / according to MMSI – chronic hyperplastic pulpitis. From the stage at which the connection of the carious cavity with the pulp is always detected, the growth of tissue, the formation of a painful and bleeding polyp when pressed, filling the free space of the pulp chamber.
K04.08 – other specified pulpitis (retrograde, traumatic, residual)
K04.09 – pulpitis, unspecified
K04.1 – pulp necrosis (pulp gangrene). It is considered to be the final stage of chronic pulpitis, which is characterized by signs of acute and chronic disease at the same time. Attacks of acute pain intensify and become more frequent, soft tissues are affected by necrotic changes, the bone tissue of the tooth is intensively destroyed, and periodontal infection is often detected during examination.
K04.2 – pulp degeneration (dentals, pulp petrification)
K04.3 – improper formation of hard tissues in the pulp (secondary or irregular dentin)2.
Pulpitis, like most diseases in principle, progresses and worsens, moving from one stage to another, but nowadays modern dentistry has methods that, in some cases, can treat this disease while maintaining the viability of the pulp. Chronic pulpitis in 90% of cases is irreversible and the only solution is removal of the pulp.
Therapeutic methods for treating dental pulp
Therapeutic or conservative are methods of treatment that make it possible to do without removing tissue. These methods of preserving dental pulp are not available to all patients; there are certain indications:
- age not older than 40 years;
- deep caries;
- acute serous-purulent or fibrous pulpitis;
- opening of the dental pulp due to trauma;
- lack of medical intervention in the inflammation process to date.
As a rule, the dentist treats the surgical field with antiseptic solutions, removes the affected tissue and places the drug into the cavity. There are two methods for performing this procedure.
- Indirect covering of the dental pulp.
An antibacterial agent is placed at the bottom of the cavity to stimulate the production of bone substance. Regeneration occurs naturally. - Direct covering of the dental pulp.
The medication is applied directly to the soft tissue to preserve the viability of healthy cells, then isolated with a pad.
Next, the tooth is restored with temporary materials, and after a secondary examination, it is finally restored.
Inflammation
Pulpitis, or in other words inflammation of the pulp, occurs in every fifth patient who comes to the dentist with acute pain in the tooth. Let us briefly consider the main issues related to this disease:
- What is pulp inflammation? When damaged enamel gets into the cracks, harmful microorganisms begin to destroy the tooth, making their way to the soft tissues. As soon as the destruction process reaches the nerve endings, very painful inflammation begins.
- Causes of inflammation. For the most part, the causes of the disease are infectious in nature, but pulpitis can begin due to mechanical damage to tooth enamel, and due to poor-quality tooth treatment in the past.
- Symptoms The main symptoms of pulpitis are acute cutting pain of a paroxysmal nature. Over time, the intervals between attacks decrease and the pain becomes constant. In a lying position, especially at night, the pain intensifies, preventing a person from falling asleep.
- Diagnostics. Unfortunately, pulpitis cannot be detected on x-rays, so it can only be diagnosed during a doctor’s examination. So, for example, pain from cold air with an inflamed pulp will last much longer than with other diseases, but tapping on the tooth will give virtually no reaction.
- Treatment. The only way to treat the pulp, as mentioned earlier, is to remove it. It is performed under anesthesia and most often in two steps. During the first, a medicine that kills the inflamed tissue and an anesthetic are placed in the tooth, and during the second, the tooth cavity is thoroughly cleaned and filled.
In recent years, a more gentle method of instrumental removal in one step has been gaining popularity. Currently, methods of treating inflammation with antibiotics and anti-inflammatory drugs are also being developed, however, such methods are not yet widespread.
Surgical methods for treating dental pulp
In cases where therapeutic methods are powerless, the only option left is to remove the dental pulp. This option is used in cases where the patient’s immunity is weakened, the disease is at an acute stage, or the tooth will be used in the future as a support for prosthetics. Surgery involves amputation or extirpation of the dental pulp.
- Amputation of the dental pulp
- during the procedure, only the coronal part is removed. Prescribed for acute pulpitis or mechanical damage to the dental pulp. - Extirpation
is the complete removal of the pulp. Used for all forms of pulpitis.
The pulp can be removed vitally, that is, under anesthesia without prior killing. If this method is not possible, the doctor resorts to devitalization of the dental pulp - the toxic substance is left in the cavity for about a day, after which the dead tissue is painlessly removed. Means for devitalizing dental pulp include arsenic or paraformaldehyde paste.
Purpose of individual cell classes
The individual components of the pulp perform different tasks:
- fibroblasts are needed for collagen synthesis;
- lymphocytes are responsible for the production of immunoglobulins;
- macrophages are needed to organize antitoxic work and remove dead cells;
- odontobalsts perform a plastic function, that is, the production of primary dentin by the pulp, the formation of a secondary one after the process is completed (the synthesis is constant, with age this leads to a decrease in the volume of the tooth chamber).
The tooth cavity is not tightly closed, so in the absence of proper care there is a risk of infection. In addition, the condition of the tissues is negatively affected by injuries, unsuccessful filling and other factors. Therefore, inflammatory processes may begin to develop inside. At the first signs, which also include pain, you should immediately contact a dentist, who will diagnose and prescribe treatment. If addressed early, the tissue can be treated, leaving the tooth alive.
Treatment methods
Primary or acute pulpitis is eliminated using three methods. Once the tooth has been diagnosed and opened, the following treatment options may be used:
- conservative (biological);
- extirpation (the exact procedure depends on the condition of the tissue);
- amputation, that is, removal of the affected pulp.
Biological treatment is aimed at restoring the condition and health of tissues and shows effectiveness only at the initial stage. For therapy, treatment is carried out with special drugs that have an anti-inflammatory effect. To do this, the cavity is opened and a tampon soaked in antimicrobial compounds or antibiotic-based solutions is placed inside. After eliminating the inflammation process, the cavity is sealed with a temporary filling. The therapy period takes about five to seven days, after which the cavity is opened, washed with a disinfectant solution and sealed.
With the extirpation method, the condition of the tissue and the viability of the organ are first determined. For the chronic stage with signs of development of the gangrenous process, vital methods of treatment are recommended; for the chronic form, preliminary devitalization is recommended. If the condition is acute diffuse, treatment is selected by the doctor based on other indicators. The main technique is to completely remove the affected pulp, which can no longer be restored. Next, the cavity is processed and sterilized, closed with a temporary filling mass for the period of elimination of inflammatory processes.
The third treatment option is to remove the pulp mass, that is, amputate it. Depending on the working conditions, two methods are distinguished - vital and devital elimination of affected tissues. The first case is usually observed in pediatric dentistry, when the mass is removed at the canal level, after which a filling is installed for a period of up to six months. After six months, the temporary polymer plug is removed and a permanent filling is placed. The second method involves the use of means to kill the pulp, which is then left in the canal for further observation.
The doctor chooses a treatment method based on the diagnosis performed and taking into account the possibility of maintaining the functionality and aesthetics of the series. If the disease is detected at an early stage, removal can be avoided, but the Patient is required to contact the dentist in a timely manner and strictly follow the rules of care. This is a mandatory condition for preserving tissue, eliminating the development of complications, inflammatory and other lesions of the pulp. Regular scheduled examinations are also needed, during which problems can be identified in a timely manner and treatment can begin.
PERIODONTIUM
The root of the tooth is held in the socket by connective tissue fibers that make up the root membrane or periodontium.
The periodontium is located in a narrow, slit-like space between the tooth root and the jaw bone. The thickness of the periodontium is 0.15-0.25 mm. With age, as well as from mechanical load, the thickness of the periodontium changes and amounts to 1.2-1.2 mm.
The basis of periodontal connective tissue are bundles of interdental and cemento-alveolar fibers, which are woven, on the one hand, into the compact plate of the alveoli, and on the other hand, into the cementum of the tooth root. In the area of the tooth neck, fibrous fibers have an almost horizontal direction and include numerous collagen fibers, circularly covering the cervical area (circular ligament). The apical periodontium contains more loose connective tissue and cellular elements. Fibrous fibers in the area of the tooth apex are represented by looser, more delicate bundles and are arranged radially; with the help of the fibers, the tooth is suspended and fixed in the bone bed.
The blood supply to the periodontium is abundant and it has a fairly developed lymphatic network. Periodontal vessels form several plexuses (external, middle, capillary) in the root area. Cellular elements are represented by fibroblasts, mast cells, plasma cells, histiocytes, cementoblasts, osteoblasts, and epithelial remnants of the neoplastic epithelium. The main function of the periodontium is support and retention. In addition, the periodontium distributes and regulates pressure on the tooth (shock absorbing), has a plastic function due to cellular elements and a barrier function (due to the unique anatomical structure and resistance to adverse environmental influences). The reflexogenic function of periodontium is also highlighted.