Normal condition of tonsils
Tonsils are collections of lymphoid tissue located in the nasopharynx and oral cavity. Tonsils perform protective and hematopoietic functions, participate in the development of immunity - they are the first line defense mechanism against inhaled foreign pathogens. The full immunological role of the tonsils still remains unclear.
Together with other lymphoid formations of the nasopharynx, the tonsils form the pharyngeal lymphatic ring
The tonsils serve as a local immune organ, a kind of barrier against bacteria and viruses that enter the pharynx during the acts of breathing and swallowing.
Tonsils are divided into:
- paired: palatine - in the recess between the soft palate and the tongue (first and second tonsils).
- tubal - in the area of the pharyngeal opening of the auditory tube (fifth and sixth tonsils)
- pharyngeal (nasopharyngeal) - in the area of the fornix and the back of the pharyngeal wall (third tonsil, Luschka’s tonsil). Pathological enlargement of this particular tonsil is called adenoids
Palatine tonsils - a focus of inflammation in chronic tonsillitis
In the upper respiratory tract of a person there are a number of formations representing an accumulation of lymphoid tissue, the so-called lymphoepithelial organs - tonsils. There is a whole lymphopharyngeal ring consisting of 7 tonsils. These are unpaired pharyngeal (adenoids), lingual, laryngeal tonsils, and paired palatine and tubal tonsils. Like any organ in our body, the tonsils can be subject to inflammatory diseases.
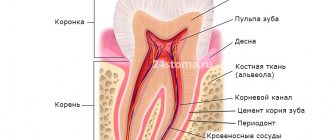
Acute inflammation of the tonsils is a sore throat. Chronic tonsillitis refers to a long-term inflammatory process in the palatine tonsils. In most cases, tonsillitis is an exacerbation of chronic tonsillitis. The palatine tonsils (tonsils) are essentially the same mucous membrane only folded into an accordion; they are dotted inside with passages - crypts, which open on the pharyngeal surface of the palatine tonsils with lacunae.
Due to the anatomical features and location of the palatine tonsils, which are located at the crossroads of the digestive and respiratory systems, they are most often, of all other lymphoepithelial formations, susceptible to the inflammatory process, which consists of degenerative processes, as a result of which, in chronic tonsillitis, the palatine tonsils are a constant source of infection and the cause of endointoxication.
Read more about tonsils
It must be said that the palatine tonsils are the largest lymphoid formations of the entire pharyngeal ring, and they play, perhaps, the leading role in the disposal of bacterial and viral infections that enter the pharynx by airborne droplets.
Due to their size, the palatine tonsils are the first to stand in the way of microbes that enter the oral cavity from the external environment, and protect the body from infection by viruses, bacteria, spirochetes, protozoa and other microorganisms.
The palatine tonsils have depressions - lacunae, which in turn are exit holes for deep and sharply convoluted canals - crypts, which are located in the thickness of the palatine tonsil, leading to its root. The number of lacunae and crypts can vary from 1 to 14, but on average, in each amygdala there are from 4 to 7 lacunae. The diameter of the lacunae can also vary, depending on gender, age, individual characteristics of the patient, as well as the duration and severity of the disease and the presence of scar changes in the tonsils themselves.
It is believed that the wider the exit hole - the lacuna - the higher the likelihood of the palatine tonsil to self-cleanse. This statement is true. Accordingly, the smaller the diameter of the lacuna, the more pronounced and severe the tonsillitis. Moreover, if the tonsil produces a large amount of caseous-necrotic detritus (plugs), the severity of the course also noticeably increases.
Normally, on the mucous membrane of the palatine tonsils, as well as in the thickness of the palatine tonsils, in the lacunae and crypts, there is a growth of non-pathogenic and conditionally pathogenic microflora, in normal (permissible) concentrations. If there are more microorganisms (for example, due to intensive growth, or the addition of other pathogenic microflora from the outside), the palatine tonsil immediately destroys and utilizes the dangerous infection and normalizes a dangerous condition for the body. At the same time, the macroorganism, that is, the person, does not notice this in any way.
The tissues of the palatine tonsils produce the following main protective substances: lymphocytes, interferon and gamma globulin.
The palatine tonsils act as a serious infectious and inflammatory barrier and are an important component in creating not only local, but also general immunity in the human body. Therefore, when it comes to removing the palatine tonsils, you first need to think ten times, weigh the pros and cons, and only after that make a decision about removing the tonsils.
Why do we get chronic tonsillitis?
The main causes of the development of chronic tonsillitis are inflammation of the tonsils and ongoing tonsil reactions, which can be caused by long-term exposure to an infectious factor.
In the photo - lymphopharyngeal ring
During the development of chronic tonsillitis, the overall level of the body’s immunity is of no small importance.
Types of chronic tonsillitis
There are several classifications of chronic tonsillitis. The issue of classification of chronic tonsillitis is closely related to the clinical manifestations of this disease. The most widely used classification is that there are only two forms: compensated and decompensated.
- The compensated form is characterized by a course without complications, rare sore throats, often the only complaint can be only plugs in the throat, the protective role of the tonsils works by holding back harmful bacteria, and their further penetration, due to this, no special manifestations of the disease are observed.
- Decompensated form This form of chronic tonsillitis is characterized by frequent sore throats at least once a year, the occurrence of local complications, such as peritonsillar abscess, and diseases of other organs and systems of the body, such as glomerulonephritis, rheumatism.
Symptoms of chronic tonsillitis
The main manifestation of chronic tonsillitis is tonsillitis; as a rule, all patients suffering from this disease at least once have had tonsillitis. Sore throat is a fairly serious disease that affects all systems of the body and carries the risk of a number of serious complications, so the choice of treatment tactics for chronic tonsillitis should be related to the frequency of tonsillitis. The main symptoms of the disease can be identified:
| Smell from the mouth | One of the most common symptoms disturbing the patient is bad breath. This symptom is due to the fact that the area of the epithelium of the palatine tonsil is quite large; during inflammation, pathological secretions accumulate in the crypts of the tonsils in the form of caseous (curdled) masses. Caseous masses are evacuated through the lacunae into the pharyngeal cavity, causing bad breath. |
| Sore throat, ear | One of the main symptoms of chronic tonsillitis is pain in the throat, often a feeling of a lump in the throat. Also, the symptoms of chronic tonsillitis can be expressed by headache, unpleasant sensations in the ear, mild pain in it, which is caused by irritation of the nerve endings in the parenchyma of the palatine tonsil and irradiation of pain along the nerve fiber to the ear. |
| Enlarged lymph nodes | You can often observe an enlargement of the lymph nodes located under the jaw, and the cervical lymph nodes also enlarge. When palpating the lymph nodes, mild pain occurs. |
Quite a large number of patients do not immediately detect the symptoms of chronic tonsillitis and delay contacting an ENT doctor, which often leads to decompensation of the disease and longer treatment in the future.
Treatment or removal of tonsils?
Dear patients! If you have visited several specialists in this field, if a course of treatment for chronic tonsillitis has been carried out and none of the methods has brought the expected result, then only in this case should you think about removing the tonsils.
If a conservative approach gives lasting results for 4-6 months or more, then the palatine tonsils are able to fight on their own. Your task is to help the tonsils by regularly sanitizing them and stimulating their work physiotherapeutically.
How to identify chronic tonsillitis
Diagnosis of chronic tonsillitis does not present any particular difficulties for an experienced otolaryngologist. The patient's medical history and complaints are of utmost importance in diagnosis; as a rule, the history includes previous sore throats and complaints of frequent pain and discomfort in the throat.
Examination of the throat for chronic tonsillitis
During mesopharyngoscopy (examination of the pharynx) for chronic tonsillitis, the following signs are present: hyperemia and roller-like thickening of the edges of the palatine arches; cicatricial adhesions between the tonsils and palatine arches; loosened or scarred and hardened tonsils; caseous-purulent plugs or liquid pus in the lacunae of the tonsils.
How is the tonsil rinsing procedure performed?
No special preparation is required before performing this procedure. Washing on this device occurs in several stages:
- first, the tonsils are treated with lidocaine; a vacuum attachment is fixed to the surface of the formation; the device creates negative pressure; the nozzle pulls out purulent plugs and removes them into a special container; the lacunae are washed with an antiseptic solution. Ultrasound injects a drug into the tonsil.
The procedure relieves inflammation, activates tissue regeneration, and removes swelling.
Complications of chronic tonsillitis
Chronic tonsillitis has serious complications; they are divided into two groups: local and general. All complications, as a rule, occur during an exacerbation of the process occurring in the form of a sore throat and represent the consequences of untimely treatment of chronic tonsillitis.
With chronic tonsillitis, in the upper respiratory tract of a person, more precisely in the palatine tonsils, there is a focus of chronic inflammation; the problem of focal infection is very acute in modern medicine. Currently, there are about fifty different metatonsillar diseases, which are the result of chronic inflammation in the palatine tonsils. Let's take a closer look at what this can most often threaten.
Peritonsillar abscess
This is the most common local complication. The fact is that between the palatine tonsil and the muscles of the pharynx to which it is attached there is fiber, the so-called paratonsillar fiber. With severe inflammation, the infection can enter this tissue through the hematogenous route, causing its infiltration and purulent melting, and an abscess is formed. Peritonsillar abscess is a very serious disease that requires immediate surgical treatment, usually in a hospital setting, since there is a threat of the purulent process spreading through the cellular spaces of the neck into the mediastinum, which can be fatal.
Diseases of the heart, joints and kidneys
An important role in the inflammatory process in chronic tonsillitis is played by group A beta-hemolytic streptococcus, which often parasitizes the palatine tonsils. The fact is that immune complexes that form in the body as a response to the aggression of this antigen can also attack healthy tissue in the joints, heart and kidneys, which, if not treated in a timely manner, can even lead to disability.
Weakness and decreased ability to work
The parenchyma of the palatine tonsils is densely penetrated by blood and lymphatic vessels, and in the thickness of the organ there are many nerve endings that connect to important autonomic centers. In chronic tonsillitis, inflammatory products enter the circulatory and lymphatic systems, and constant endotoxification occurs. All these factors plus pathological impulses from irritated nerve endings lead to decreased tone, bad mood, and apathy.
Regular colds
With chronic tonsillitis, the body spends a lot of effort to contain inflammation in the tonsils, the immune system is under constant stress, which leads to its significant weakening. Added to this is the not always correct work-rest regime, nutrition, and environmental conditions, as a result of which a person with chronic tonsillitis may literally not “get out” of a cold.
Inflammatory diseases of the respiratory system
The palatine tonsils are anatomically located in the pharynx, close to such organs as the trachea, larynx, and paranasal sinuses. With chronic tonsillitis, microbial contamination of the entire area of the respiratory mucosa occurs, which contributes to the development of diseases such as sinusitis, bronchitis, and laryngitis.
Stomach and intestinal problems
The palatine tonsils are located at the crossroads of the digestive and respiratory systems. Due to certain anatomical features, they represent a rather large conglomerate of the mucous membrane. In chronic tonsillitis, this entire area of the mucosa is involved in the inflammatory process and secretes a pathological secretion in the form of a liquid fraction and caseous masses. This pathological content is evacuated into the pharynx through lacunae and then swallowed with saliva, which often causes disturbances in the functioning of the gastrointestinal tract.
Chronic tonsillar pathology occupies a special place among chronic lesions of the ENT organs. This is due to both the relatively rapid chronicization of the process in the palatine tonsils and the possibility of the development of generalized, even fatal, complications, as well as the peculiarities of the course and influence on the body of associated (metatonsillar) diseases. According to various authors, from 4 to 35% of the population suffer from chronic tonsillitis, while in different regions of the Russian Federation there is an increase in the number of patients suffering from this pathology.
Chronic tonsillitis, being a classic example of a focal infection, is essentially a chronic infectious-allergic disease with a local inflammatory reaction in the palatine tonsils, which makes it possible to develop a whole set of complications based on the activity of β-hemolytic streptococcus, its antigens and various pathogenicity factors , in which streptolysins play a key role.
It is known that most acute inflammatory diseases characterized by damage to the ENT organs, in the absence of adequate therapy, tend to become chronic. However, the pathology associated with the palatine tonsils has pronounced distinctive features both in the formation of chronic inflammation and in the strict phasing of the development of this pathological process. In the natural physiological functions of the palatine tonsils, normal and pathological processes interact so closely that, despite the large number of diverse studies that have been carried out on this problem, until now it has been practically impossible to establish an absolutely definite “point of no return” when irreversible pathomorphological changes occur in the structure of the palatine tonsils, and radical treatment methods, in particular tonsillectomy, are already required. The lack of a consensus solution on this issue in the modern medical community only further aggravates the problem.
Thus, very often in routine clinical practice, when choosing further tactics for patient management, doctors are guided primarily by anamnestic data on the number of sore throats and peritonsillar abscesses suffered, focusing more on subjective sensations than on objective clinical symptoms and data from laboratory research methods. Meanwhile, the currently existing classification of chronic tonsillitis B.S. Preobrazhensky—V.T. Palchun (and the diagnostic criteria embedded in it), developed at one time at the Department of Otorhinolaryngology of the Russian National Research Medical University named after. N.I. Pirogov, allows you to clearly differentiate various forms of chronic tonsillar pathology and gives a clear indication of further tactics for managing this patient [1, 2]. Unlike existing classifications of chronic tonsillitis, this classification reflects the stages of development of the pathological process in the structure of the palatine tonsils and the influence of these processes on the body as a whole in accordance with the main pathogenetic links of this disease. At the same time, the comments to this classification directly state the need to perform tonsillectomy in patients with chronic tonsillitis of the toxic-allergic form (TAF) II, as well as, in case of ineffectiveness of conservative therapy, in patients with chronic tonsillitis TAF I. However, despite this, it is regrettable to state that in the medical environment and especially in the therapeutic community, there is still an opinion about the need to preserve the palatine tonsils as an immunocompetent organ by any means, even despite the possible severity of general somatic symptoms and the obvious failure of the palatine tonsils in conditions of profound changes in its structure against the background of pronounced chronic changes .
That is why, when choosing a treatment method for a patient with chronic tonsillar pathology, it is necessary, first of all, to be guided by the knowledge that has been accumulated on this problem at present, and to objectively assess the risk of complications that can lead to the development of, including lethal symptoms, and the classification of chronic tonsillitis B.S. Preobrazhensky - V.T. Palchuna should be the main guideline for detailing the diagnosis and, on this basis, choosing tactics for further management.
The stages of development of pathomorphological changes in the structure of the palatine tonsils, as well as the formation of general and local associated diseases (metatonsillar complications), reflected in the classification of B.S. Preobrazhensky—V.T. Palchun, are largely determined by the biological properties of the main etiologically significant microorganisms [3].
According to the results of many studies conducted in recent decades, among the microorganisms that claim to be the leading etiological factor in the development of chronic tonsillitis, one can find a large number of pathogens with different properties, including streptococci, staphylococci, Haemophilus influenzae, lymphotropic viruses, etc. In accordance with According to the results of these studies, chronic tonsillitis is considered to be a polyetiological disease. Considering this issue from the perspective of clinical microbiology, it should be noted that in most cases, causally significant microorganisms are primarily bacteria growing in the distal parts of the crypts of the palatine tonsils. Since these sections of the tonsils have an extremely low oxygen content, the dominant flora growing on the surface of the mucous membrane of the tonsil crypts are microorganisms with an anaerobic type of metabolism, which are represented by peptococci and bacteroides. prevotella, fusobacteria, etc. However, the leading role in the development of chronic changes in the palatine tonsils, as well as local and general complications of chronic tonsillitis is given to β-hemolytic streptococcus of the serological group, A ( S
.
pyogenes
) - a microorganism that also uses anaerobic respiration for its life. At the same time, the palatine tonsils are the only natural reservoir of pyogenic streptococcus in the macroorganism [4, 5].
And it is this fact that in most cases determines the development of toxic-allergic manifestations in the human body, leading to the formation of common diseases associated with chronic tonsillitis. Among these diseases, acute rheumatic fever and post-streptococcal glomerulonephritis should be particularly highlighted, which, as a rule, lead to pathology of the cardiovascular and urinary systems, and also worsen the quality of life and, ultimately, shorten it [6-8].
S
.
pyogenes
are microorganisms that are gram-positive cocci, having a classic type of arrangement for streptococci - in the form of a chain, giving complete lysis of red blood cells (beta-hemolysis) on blood agar and belonging to the serological group, A in the antigenic classification of streptococci by R. Lensfield. Streptococcus pyogenes has significant resistance to physical and chemical environmental factors. The only natural reservoir of pyogenic streptococcus in the macroorganism is the distal sections of the lacunae of the palatine tonsils.
The pathogenesis of pyogenic streptococcal infections is associated with the activation of these microorganisms in the deep sections of the lacunae of the palatine tonsils, their subsequent invasion into the structures of the lymphoid tissue of the tonsils due to the presence of a large number of extracellular enzymes - streptokinase, which catalyzes the conversion of plasminogen into the proteolytic enzyme plasmin, hyaluronidase, which destroys hyaluronic acid, which is the main a component of connective tissue, streptodornase (DNAase), which destroys elements of the genome of connective tissue cells, etc. The production of membrane-damaging toxins O- and S-streptolysins specific to this pathogen leads to the development of systemic intoxication, cardiotoxicity, which is explained by the suppression of energy processes in the mitochondria of myocardial cells under conditions of O-streptolysin activity, which also has hemolytic activity and immunogenic properties. The action of S-streptolysin together with the antichemotactic factor (peptidase C5a) is associated with the suppression of the activity of phagocytic cells and the destruction of mitochondrial membranes of cells in the lesion. The specificity of clinical symptoms of damage to the palatine tonsils is primarily due to the action of these pathogenicity factors.
In addition, a feature of the cell wall of pyogenic streptococcus can be considered the presence of a large number of surface protein structures, in particular M-protein, which is an important adhesin of these microorganisms. M-protein ensures binding to collagen, fibronectin, as well as serum proteins - fibrinogen, components of the complement system, as well as other elements of various organs and systems, causing activation of the primary phase of development of metatonsillar complications. The ability of pyogenic streptococcus to penetrate into epithelial cells with the development of the phenomenon of internalization is associated with the presence of M-protein. Streptococcus pyogenes has a hyaluronic capsule that protects it from immunological surveillance authorities and is a factor in antiphagocytic activity.
In addition, S
.
pyogenes
has and synthesizes a large number of substances that have the properties of superantigens, cause mitogenic activity and lead to polyclonal proliferation of T lymphocytes. Superantigens of streptococci include pyrogenic exotoxins (SPE A, SPE B, SPE C, SPE D), the mitogenic factor SPE F and, probably, type-specific M proteins [2, 9]. Pyrogenic toxin, A (Spe A), whose gene is localized on a temperate bacteriophage, is associated with the most severe forms of streptococcal infection. The gene encoding this toxin is detected in ½ of cases of scarlet fever and rheumatic fever. The pyrogenic toxin B gene is localized in the chromosomal DNA of the cell and is a cysteine proteinase that is capable of breaking down fibronectin in the macroorganism. In patients with invasive forms of streptococcal infection (cellulitis, pneumonia, necrotizing fasciitis), there is an increased level of antibodies to pyrogenic exotoxin B (SPE B). In addition, the production of SPE B by streptococci was combined with a high risk of developing acute post-streptococcal glomerulonephritis [10, 11].
It has now been proven that streptococci can not only attach to the cells of the macroorganism, but also penetrate them. Thus, A. Osterlund [12], examining the tonsils of children with recurrent tonsillitis, identified streptococci located inside the cells, and 30% of failures in the treatment of chronic tonsillitis are associated with the presence of the pathogen intracellularly.
It should also be noted that β-hemolytic streptococcus persists in the structure of the mucous membrane of the crypts of the palatine tonsils not in the form of planktonic cultures, but in the form of pathological biofilms, which determine not only protection from exogenous environmental factors, but also resistance to various methods of therapeutic intervention [13, 14].
In the development of the stages of the clinical picture of tonsillitis (which are reflected in the classification of B.S. Preobrazhensky - V.T. Palchun), several factors associated with pyogenic streptococcus take part: 1) a toxic factor that determines the pathological effect of streptolysins on the cardiovascular, nervous and endocrine system, which is manifested by general intoxication, fever, etc.; 2) a septic factor, which is associated with the influence of enzymes of the pathogenicity of beta-hemolytic streptococcus, resulting in a local inflammatory reaction in the structure of the palatine tonsils and further invasion of microorganisms deep into the tissues with the possibility of further generalization of the process, often hematogenously, up to the development of tonsillogenic sepsis, severe reaction of lymph nodes, etc.; 3) an allergic factor (a complex of surface substances of pyogenic streptococcus), which causes sensitization of the macroorganism to beta-hemolytic streptococcus and antigens of destroyed body tissues, which then leads to the development of glomerulonephritis, myocarditis, etc. [2].
Analyzing all of the above, we have to state that the pathogenicity factors of streptococcus pyogenes and its biological properties directly affect the nature of the clinical course of tonsillar pathology and its complications, which proves the leading role of this microorganism in the genesis of chronic tonsillitis.
Features of the anatomical and histological structure of the palatine tonsils, along with the biological properties of pyogenic streptococcus, also make a significant contribution to the development of chronic inflammation in them. Being part of the lymphoepithelial pharyngeal ring, the palatine tonsils are not only the largest in size, but also the most complex structure among all the elements of this ring, which largely determines the development of a focus of chronic infection.
Thus, it is known that the palatine tonsil consists of lobules that have a complex structure. From different parts of the connective tissue capsule of the tonsil, bundles of connective tissue run towards the pharynx surface, forming the basis of the lobules (stroma). Then these main cords branch into smaller ones that penetrate the entire amygdala. The tonsil parenchyma is a group of lymphoid follicles located in a finely looped connective tissue network. In the center of such more or less rounded follicles there is a zone that, when preparing a microslide, has a lighter color - the so-called germinal center, where young lymphocytes are formed, which, as they develop, are gradually pushed towards the periphery of the follicle. An important feature of the palatine tonsils, which determines both normal physiological and pathological processes, is the presence of crypts. They begin on the pharynx surface and go deep into the tonsil, branching like a tree. The crypts, like the entire pharyngeal surface of the tonsil, are lined with stratified squamous epithelium in 6-8 rows.
In some places of the crypts the epithelial cover is interrupted (areas of physiological angization). Here contact between microorganisms and lymphocytes occurs. It is the areas of physiological angization that provide contact of microorganisms with the mantle zone of the follicles. Microorganisms growing on the surface of the crypts freely penetrate into the lymphadenoid tissue exposed in these breaks in the epithelium. In this way, a natural biological mechanism is formed that ensures the penetration of an infectious agent from the external environment into the lymphoid tissue of the tonsil, which leads to the initiation of the development of the germinal center of the follicles of the palatine tonsil, the differentiation of B-lymphocytes into highly specific plasma cells capable of synthesizing high-avidity antibodies. Immune control ensures the death of microorganisms that have penetrated into the parenchyma of the NM. In this case, the source of infection is inactivated by the general immune factors of the macroorganism. The bacteria die, but retain particles of their antigenic structure, which is an additional stimulus for the activation of local and general immunological reactions.
Recognition of antigenic structures of microorganisms also occurs due to Toll-like receptors. At the same time, a number of authors note that not only lymphocytes express Toll-like receptors (TLRs) on their surface, which play a key role in the recognition of microorganisms. These receptors are found in epithelial cells of the tonsils, primarily in the cryptal and luminal cells [15]. The detection of these receptors in the epithelium of the tonsils may indicate its functional role as antigen-presenting cells, and this also serves as confirmation that in conditions of a normally functioning tonsil, the lining of the crypts is not damaged.
Thus, the very structure of the amygdala, namely tree-like branching crypts with 4-6 orders, contributes to the formation of acquired immunity, increasing the time of contact of the pathogen with immune cells. However, in situations where the outflow of contents is delayed beyond a certain time, the lacunae acquire the ability to cystic expansion. Under these conditions, the crypt epithelium begins to be affected for a long time by toxins of microorganisms, which subsequently take a direct part in the formation of various toxic-allergic manifestations. That is why the delay in the outflow of the contents of the lacunae is one of the important mechanisms for the development of chronicity of the process, and also takes part in the genesis of associated pathology, the further systemic impact of the formed chronic focus of infection on the macroorganism and the formation of gross pathomorphological changes in the tissues of the tonsils themselves.
The starting point in the development of chronic tonsillitis is a violation of the local immune status of the mucous membrane of the palatine tonsils, which, together with the effects of bacterial toxins and sometimes lymphotropic viruses on the crypt epithelium, can lead to its thinning and the formation of areas of no longer physiological, but pathological angization. This allows etiologically significant microorganisms to penetrate into the deep cellular layers of the mucous membrane, deep into the tonsil parenchyma, into the blood vessels and initiate further pathological processes.
It should be noted that in modern literature there is little data on the changes that occur in the palatine tonsils at different forms and stages of chronic tonsillitis at the cellular level. The research conducted at our department helped to complement the understanding of the physiology and pathophysiology of the palatine tonsils in conditions of the formation of chronic inflammation in them. During the study, the autoradiography method was used to evaluate the histoarchitecture of the palatine tonsils, as well as to determine the functional activity of microorganisms located in the tonsillar parenchyma, both normally and in patients with chronic tonsillitis. The essence of the method was the use of radioactive precursors of nucleic acids (3H-thymidine, 3H-uridine). The accumulation of 3H-thymidine by the cell demonstrates the ability of these cells to synthesize DNA, i.e., indicates their proliferative activity. The synthesis of RNA, which is the template for protein synthesis, reflects the functional activity of the cell. In addition, the cell's ability to absorb and accumulate radioactive tracers makes it possible to differentiate viable bacteria and normally functioning tonsil cells from nonviable cellular debris.
According to the results of these studies, in the tissues of unchanged palatine tonsils, microorganisms were found exclusively on the surface of the mucous membrane of the crypts, while the epithelial cells of the palatine tonsils had a normal structure, were characterized by a normal nuclear structure, and the absence of pathological proliferative activity. In addition, in healthy palatine tonsils, only individual endothelial cells showed insignificant functional activity, i.e., they synthesized RNA.
During the formation of a chronic focus of infection and the development of toxic-allergic forms, on the contrary, a violation of the cytoarchitectonics of the tonsil tissue was observed: the growth of connective tissue into the lymphoid tissue, the appearance of individual foci of necrosis, signs of destruction of the walls of microcirculatory vessels, and necrotic changes in the epithelial lining of the crypts appeared. A characteristic feature of patients with toxic-allergic forms of chronic tonsillitis was the detection of microorganisms in the tonsil tissue. At the same time, microorganisms absorbed both 3H-uridine and 3H-thymidine, which indicated not only their functional (protein synthesis), but also proliferative activity. Moreover, some functionally active microorganisms were compactly located in the structure of the pathologically altered vascular endothelium. It is necessary to understand that the formation of connective tissue, microabscesses, granulations inside the parenchyma of the tonsils contributes to the isolation of microorganisms, as well as their resistance to conservative treatment methods. Pathomorphological changes that occur in the palatine tonsils lead to the loss of the immune function of the latter.
In addition, a detailed study of tonsil follicles using various immunohistochemical markers provides insight into the processes occurring in the tonsils at the cellular level. A study on the Ki-67 cell proliferation marker in patients with hypertrophic tonsillitis and a negative test for β-hemolytic streptococcus group A in comparison with patients with chronic tonsillitis and laboratory-confirmed streptococcal presence indicates a predominance of cell division in patients without an infectious process in the tonsils, in difference from patients with chronic tonsillar pathology associated with pyogenic streptococcus. At the same time, markers of apoptotic and anti-apoptotic activity demonstrate a picture of degenerative changes in the structure of the palatine tonsils in patients with chronic tonsillar pathology. Thus, changes in caspase-3, Fac/CD95, Fax suggest the predominance of cell death processes in the tonsils with chronic inflammation caused by a bacterial nature.
The expression of markers of anti-apoptotic activity, such as Bcl-2 and surferin, also demonstrates their predominance in the palatine tonsils of patients with chronic tonsillar pathology [16].
The penetration of pathogens into the tonsil parenchyma, in addition to the events described above, is characterized by a slight increase in the volume of lymphoid follicles, disorganization of reticular fibers, and subsequently their death with replacement by connective tissue and the development of a scar process [2, 17]. All this gradually leads to a decrease in the total area of active lymphoid tissue in the tonsil and contributes to the “burying” of microorganisms between scar tissue, and also creates conditions for the development of reactive complications of chronic tonsillitis.
Thus, chronic inflammation developing in the structure of the tonsils radically changes the cytoarchitectonics of the palatine tonsils, transforming them from functionally active immune structures into a dangerous focus of the infectious process in the body, leading to its sensitization and the development of toxic-allergic manifestations.
The issue of treatment of patients with chronic tonsillar pathology remains, perhaps, one of the most controversial in otorhinolaryngology. And if making a diagnosis of “chronic tonsillitis”, as a rule, does not cause difficulties, then deciding on the stage, phase, form of the disease and, as a consequence, the choice of treatment method, raises a large number of questions and is often based on the subjective feelings of the doctor.
Along with the classical bacteriological method for diagnosing chronic tonsillitis and identifying the pathogen, in recent years a large number of new methods have been developed not only for diagnosing chronic tonsillitis, but also for assessing the functional state of the tonsils.
A method for assessing the functional state of the palatine tonsils by cytological examination of the contents of their crypts in chronic tonsillitis is proposed.
E.V. Tyrnova and G.S. Maltsev propose a biochemical method for diagnosing chronic tonsillar pathology, based on the determination of C-reactive protein, rheumatoid factor and antistreptolysin-O in blood serum [18].
V.M. Tsirkunov et al. [19] propose a method for diagnosing the degree of activity and stage of chronicity of chronic tonsillitis, based on a biopsy of the palatine tonsils.
L.A. Dyukov et al. [20] propose a method for quantitative scoring of the state of intestinal microbiocenosis in patients with chronic tonsillitis with the determination of the dysbiosis index as a method of additional diagnosis of various forms of chronic tonsillitis.
However, none of these methods are widely used in clinical practice for various reasons. But it is the timely and correct determination of the form of the disease that guarantees success in treatment and protects the patient from complications.
In the current conditions, based on the polyetiology of chronic tonsillitis, the lack of a generally accepted instrumental or functional diagnostic method, the danger of developing local and general complications, the classification of chronic tonsillitis proposed by B.S. Preobrazhensky and V.T. Palchun, not only has not lost its relevance, but, on the contrary, is acquiring primary importance in the choice of treatment methods for this disease and makes it possible to establish strict indications for surgical treatment.
The undoubted advantage of the classification of chronic tonsillitis under consideration is its clear focus on the etiology, pathogenesis of the disease, the risk of developing concomitant and associated diseases, as well as a reflection of the stages of development of the process in the macroorganism both at the systemic and cellular levels.
Thus, with a simple form of chronic tonsillitis and the absence of signs of systemic changes in the macroorganism, courses of conservative therapy are possible.
In case of chronic tonsillitis TAF I degree, when microorganisms penetrate into the tonsil parenchyma and progressive inflammatory changes develop, leading to sclerosis of the parenchyma, the walls of blood vessels are damaged and their lumen increases, the patient is shown a test course of conservative treatment, including local (washing the lacunae of the palatine tonsils) and systemic antibacterial therapy. If success is achieved with this treatment, it may be continued. However, dynamic monitoring of the patient is necessary so as not to miss the moment of transition of the disease to the next form. If there is no effect from the test course of therapy, surgical treatment is indicated.
A characteristic feature of stage II TAF is the formation of microfoci of necrosis in the structure of the tonsillar, which leads to complete functional failure of the tonsil, expressed in atrophy and death of the follicles. In the tonsils, decay processes prevail, microbial cells are found in the lumen of blood vessels along with cellular and microbial detritus, and metatonsillar complications develop. With this form of chronic tonsillitis, there is no need to talk about the possibility of conservative treatment of a source of chronic infection in the body, and the only method to cure the patient and prevent the development of complications is to remove the tonsils.
A timely tonsillectomy not only cures the patient and protects him from serious complications, but is also cost-effective. In a study conducted in 2002 by N. Bhattachatyya and L. Kepnes [21], patients were observed after tonsillectomy (average follow-up duration 37.7 months). In addition to the subjective improvement in quality of life, during the 12 months after surgery, there was a decrease in antibiotic consumption by an average of 5.9 weeks per year. The number of days of disability associated with chronic tonsillitis decreased by an average of 8.7 days per year. The number of disease-related visits to the doctor decreased by an average of 5.3 visits per year. And taking into account all the economic costs of the operation, the break-even point occurs 2 years after the operation.
Even taking into account the obvious differences in the tactics of treating chronic tonsillitis, which are a consequence of fundamental differences in the issues of financing and organization of medical care, the place of scientific research in clinical practice, the capabilities of health insurance systems in Russia and abroad, the understanding of the inevitability of eliminating the source of infection for the patient’s health remains the same . In this case, the main guideline for deciding the choice of therapeutic treatment tactics or the need to perform tonsillectomy should be the form of chronic tonsillitis in accordance with the classification of B.S. Preobrazhensky–V.T. Palchuna. In this regard, and also taking into account the stated modern ideas about the etiology, pathogenesis and clinical picture of chronic tonsillitis, it is worth thinking about the need for widespread use of this classification in the practice of otorhinolaryngologists in Russia. We invite specialists to take part in a discussion on this issue on the pages of the magazine.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about authors
Palchun V.T. — e-mail; https://orcid.org/0000-0002-3521-7424
Kryukov A.I. — e-mail; https://orcid.org/0000-0002-0149-0676
Gurov A.V. — e-mail; https://orcid.org/0000-0001-9811-8397
Ermolaev A.G. - e-mail; https://orcid.org/0000-0003-2642-5173
Corresponding author:
Gurov A.V. — e-mail: [email protected]
Palchun V.T., Kryukov A.I., Gurov A.V., Ermolaev A.G. Palatine tonsils: physiology and pathology. Bulletin of Otorhinolaryngology
. 2019;84(6):11-16. https://doi.org/10.17116/otorino20198406111
Surgical treatment of chronic tonsillitis
The whole variety of methods for treating chronic tonsillitis is divided into two large groups: surgical methods and conservative ones. Let us dwell in detail on surgical treatment. A radical surgical method is tonsillectomy - removal of the organ along with the capsule should not be confused with tonsillotomy, which is often done in childhood.
Video: tonsillectomy - removal of tonsils
With tonsillotomy, unlike tonsillectomy, not the entire organ is removed, but only a fragment of the hypertrophied parenchyma of the pharyngeal surface of the tonsil. It is necessary to resort to tonsillectomy in extreme cases; for this there must be compelling indications, such as a complicated advanced form of the disease, despite the fact that all possible methods of conservative treatment have been exhausted. Despite these “canons” that have been established for many years, removal of tonsils is often resorted to due to the lack of availability of conservative treatment, and sometimes due to the banal lack of a competent specialist dealing with this issue.
The function of the palatine tonsils is extremely important - it is an element of the pharynx, after the removal of these organs, areas of the pharynx that were covered by these formations begin to be subject to irritation by air and food masses, is this good or bad? Apparently this is bad, since nature, as a result of a long process of evolution, did not give us a single extra organ.
Preparation of an ozonized solution for a session of deep vacuum ultrasonic sanitation of the palatine tonsils
Often, tonsils are removed from patients who have not even had a history of sore throat, and whose only complaint was caseous plugs in the throat and bad breath. The long-term result of operations to remove palatine tonsils is often severe sore throat and the development of atrophic pharyngitis, which is difficult to treat.
Conservative methods of treating chronic tonsillitis include various methods of washing the tonsils. Comprehensive information about this manipulation is presented in the article washing the tonsils.
Surgical removal of tonsils
If we talk about the removal of the tonsils, then the operation to completely remove the tonsil tissue is called a bilateral tonsillectomy.
Partial removal of the tonsils is called a bilateral tonsillotomy.
It is extremely rare that the palatine tonsil is removed routinely on one side. There is also a practice of a number of hospitals (they like to do this in the Pirogov City Clinical Hospital No. 1) of removing the palatine tonsil or tonsils in case of a paratosillar abscess. This operation is called abscessonsillectomy. But it must be remembered that against the background of severe pain caused by an abscess, removal of the tonsil is extremely painful. Due to the purulent process, it is impossible to provide adequate anesthesia. Therefore, it is necessary to anesthetize the peri-almond tissue only with strong anesthetics: Ultracaine and Ultracaine DS-forte.
Routinely, palatine tonsils can be removed under local anesthesia or general anesthesia. Previously, this operation was performed only under local anesthesia.
Fortunately, there is now modern equipment that allows removal of palatine tonsils under general anesthesia or under anesthesia using cold plasma coagulation - Coblator.
Treatment of chronic tonsillitis without surgery
Despite the wide market of medical services, there are not so many effective conservative methods of treating chronic tonsillitis. The fact is that in modern otorhinolaryngology it is customary to divide the mucous membrane into fragments, there are doctors who deal only with diseases of the nose - rhinologists, there are specialists who deal only with the treatment of the throat. In fact, the entire area of the mucous membrane lining the upper respiratory tract is one organ.
Session of deep vacuum ultrasonic sanitation of palatine tonsils with ozonated solution
We are forced to obtain oxygen from the air, and the air is not sterile; the respiratory organs, like no other system of our body, experience a colossal biological load and are constantly in contact with microbes. The anatomical structure of the upper respiratory tract is the product of a long period of evolution. The upper respiratory tract is a complex mechanism created by nature with one purpose: to be a protective barrier. Moreover, many ENT diseases (adenoids, vasomotor rhinitis, sinusitis, chronic pharyngitis), which are classified as different and treated in different ways, are essentially one disease in different stages of development, so to speak, a “machine” in different stages of breakdown.
Video: treatment of chronic tonsillitis
So, the essence of many inflammatory ENT diseases, including chronic tonsillitis, is a degenerative process in the mucous membrane, caused by the microbes that we breathe, as a result of the weakening of the protective properties of the mucous membrane. It follows from this that when doing treatment you need to influence the entire area of the mucous membrane of the upper respiratory tract, you just need to take into account some anatomical features - such as the structure of the palatine tonsils, and taking these features into account, locally enhance the therapeutic effect. Since the palatine tonsils are essentially the same mucous membrane only folded into an accordion, washing the tonsils should be an integral part of the treatment process.
Conducting a photodynamic therapy session on the pharynx area for chronic tonsillitis
The lack of effective methods for treating chronic tonsillitis is also due to the fact that there are a number of dogmas in modern medicine. One of them is that the most common way to fight germs today is with antibiotics. Antibiotics, unfortunately, do not penetrate well into the upper layers of the degenerative mucous membrane; moreover, they do not restore it. With chronic inflammation, the regeneration of the mucous membrane is disrupted and microerosions form on it. Figuratively speaking, the mucous membrane becomes like a “sieve,” which is the most important basis for the inflammatory process.
Stimulation of reflexogenic zones in chronic tonsillitis
Taking into account the above, the main task of treating chronic tonsillitis is to influence all parts of the pathogenesis of the disease, therefore the following methods are used in our clinic:
| Cleansing tonsils with ozonized solution | In our clinic, we wash the palatine tonsils using the tonsillor apparatus with an ozonated solution, which is by far the most effective way to cleanse the entire thickness of the tonsils from pathological contents. |
| Sanitation of mucous membranes with mineral salts | In our clinic, we irrigate the entire mucous membrane with a solution of individually selected mineral salts, which sanitize the mucous membrane and restore it, which cannot be achieved with modern antibiotics. We also activate mucosal regeneration using photodynamic therapy. Lymph stasis plays an important role in the pathogenesis of inflammation, including chronic tonsillitis. Activation of lymph flow in the area of inflammation plays an important role: this is how the “soldiers” of our immunity - lymphocytes - move along with lymph. |
| Stimulation of reflexogenic zones | With the help of injections into the reflexogenic zone of the neck, ozone causes a spasm of the subcutaneous lymphatic vessels, which activates the lymph flow in the pharynx, leading to rapid stabilization of the immune system. The integrated approach we use affects all parts of the pathogenesis of chronic tonsillitis, which allows it to be treated conservatively, avoiding surgical treatment. |