- An effective way to preserve the integrity of the tooth and prevent the spread of infection.
- Modern painless methods of performing the procedure.
- The fastest possible return to normal life.
Sign up for a consultation
Once the pulp (nerve tissue and blood vessels) is removed, the tooth becomes hollow. If it is not filled with filling material, then the process of spreading caries and other infections will continue. Pathogenic microflora can lead to damage to the periodontium - the tissues surrounding the root of the tooth, in which case there is a high probability of its loss. In addition, the spread of infection can lead to the formation of cysts and fistulas, the appearance of sinusitis and osteomyelitis. In order to prevent this, obturation (filling) of the canal of the pulpless tooth is performed.
Indications and contraindications
|
|
Materials for root fillings
Prices for dental canal filling depend on the chosen procedure method and the consumables used. We, as modern dentistry, use:
- plastic material, gutta-percha, for the main filling of the tooth canal
- and special sealers and pastes to ensure maximum tightness.
Gutta-percha is the most modern material with antibacterial activity. It does not dissolve and does not lose its properties throughout the life of the tooth. The sealer we use (AH plus, Dentsply, USA) is recognized as the “gold standard” for root canal treatment all over the world.
Contraindications to root canal treatment
The procedure has a number of contraindications:
- Hypertension during a crisis.
- Diabetes in the stage of decompensation.
- Diseases of the immune system.
- Severe osteoporosis.
- Respiratory infections.
If you are taking medications to thin your blood, you should tell your doctor. In this case, the specialist may prescribe a two-day medication break. If there is a contraindication to the treatment of dental canals, then tooth extraction and prosthetics on an implant can be performed.
Recommendations for recovery
After completing the procedure, you must follow the recommendations:
- Do not eat food for 2-3 hours. This is because the treatment area will not be sensitive and you may accidentally damage it while eating.
- For the first few days, do not eat solid foods.
- Take a course of antibiotics if prescribed by your doctor.
- Clean your mouth regularly and thoroughly.
- Place a permanent filling in a timely manner if, after the procedure, the canal was filled with temporary material. If the temporary filling becomes too thin, you should consult a doctor.
In most cases, one week is enough for the rehabilitation period. During this period, the oral cavity is completely restored. In the first 2-3 days, quite intense pain may be observed. During this period, you should take painkillers that are recommended by a specialist. Cephallosporin antibiotics are usually prescribed for a course of 5-7 days.
For high-quality root canal treatment, contact the World of Dentistry clinic. Our undeniable advantage is qualified dentists and the optimal cost of services.
Canal filling techniques
Lateral condensation method
Vertical condensation of gutta-percha
A simple and effective way to fill root canals. The doctor applies a liquid paste to the gutta-percha pin, after which the latter is inserted into the tooth cavity. Using the tool, the cavity is filled with additional pins, which completely seal the canal.
This is a method of filling tooth canals with a complex shape (anatomy). Using a special thermal nozzle, the doctor introduces heated and softened gutta-percha into the canal.
Mechanical treatment of root canals
The main task of mechanical treatment of dental canals is their expansion for the purpose of high-quality filling. If mechanical treatment is not carried out, the channel will be heterogeneous, having narrowings and expansions. This factor will become an obstacle to completely filling the canal with filling material.
Mechanical treatment of dental canals can be carried out in two ways:
- Using hand tools. The method involves placing medical devices into the root canal and gently rotating them.
- Using an endodontic handpiece. Special profile files made of nickel-titanium are placed in the tips. Under the influence of the tip, the pro-file rotates in the channel, and its sharp edges remove chips from the walls of the channel, making it wider. The advantage of pro files is the so-called shape memory. Thanks to this feature, the instruments do not break even in very curved canals. This eliminates the risk of serious complications associated with a piece of dental instrument remaining in the canal.
Benefits of using an endodontic handpiece
- Compared to the use of hand instruments, the endodontic handpiece provides better treatment of the canals. After machine processing, the canal walls become very smooth. This allows for easy insertion of gutta-percha filling pins.
- Treatment with an endodontic handpiece takes significantly less time compared to manual treatment.
- The technique is safe. Typically, the handpieces are equipped with a micromotor that controls the rotation of the pro-file in the dental canal. If the permissible load is exceeded, the micromotor stops the rotation of the pro-file. Thus, there is no risk of tool breakage, which cannot be guaranteed with manual processing. Not every doctor can feel the extreme resistance at which the instrument may break.
Our clinic uses machine processing using “smart” instruments. The processing is carried out by top-level specialists. Therefore, we can guarantee the safety of the procedure.
Treatment regimen
- Diagnostics Before treatment, an x-ray or computed tomography must be done to determine the number of channels, their location and shape.
- Anesthesia The doctor selects an anesthetic and, if necessary, conducts sensitivity tests to various drugs.
- Installation of a rubber dam An obligatory aspect of modern treatment is the isolation of the tooth from oral fluid using a special latex scarf (rubber dam).
- Instrumental and medicinal canal treatment The essence of root canal treatment is high-quality disinfection of the tooth cavity. To do this, the doctor expands the canal with instruments, gives it the desired shape and rinses it with disinfectant solutions to destroy the infection.
- Preparing the canals The doctor measures the length of the canals using an apex locator, after which they are mechanically expanded and smoothed out the walls.
- Filling canals Cement, a pin, or a combination of both are injected into the prepared cavities, depending on the chosen treatment method.
- Control image The doctor evaluates the quality of canal filling, after which he performs tooth filling and other necessary procedures. In addition, the patient receives recommendations for further oral care.
Clinical aspects of modern means and methods of intracanal medicine in endodontics
Practical recommendations for the use of products available on the dental market. Information is provided on modern means and methods of intracanal medicine, requirements for drugs, classification, description of individual drugs and methods of use.
It is known that one of the most important stages of endodontic treatment, which has a significant impact on its prognosis, is antimicrobial treatment of the root canal system [2,3,5]. Today, endodontics has extensive information about the structure of the root canal system. It is known that the overwhelming majority of root canals have an irregular shape, different diameters in the buccolingual and mesiodistal directions, numerous lateral canals, anastomoses and isthmuses, the presence of a delta in the apical part, the formation of not one, but several apical foramina, etc. In this regard, it becomes obvious that such a complex system is not possible to clean only mechanically [6].
Another major problem in root canal disinfection is intracanal biofilm [1]. According to the modern concept, microorganisms in root canals are present in the form of a bacterial biofilm, which makes their elimination from the root canal system difficult. Biofilm is a community of microorganisms surrounded by an extracellular matrix and attached to a moist surface. The polysaccharide matrix prevents the penetration of antibacterial agents into the biofilm, therefore, to eliminate the biofilm, a combination of both a mechanical factor that destroys the structure of the biofilm and a disinfectant agent that destroys its constituent microorganisms is necessary. Therefore, the main therapeutic measure in endodontics is considered to be the impact on the microflora of root macro- and microcanals using combined medicinal and instrumental treatment. At the same time, given the high infection rate of the root canal system, high-quality and effective medicinal treatment of root canals becomes of great importance.
Requirements for funds
medicinal treatment of root canals.
In recent years, there has been a clear trend towards the use of gentle methods of treating pulpitis and periodontitis, creating favorable conditions for reparative regeneration, and the requirements for medicinal treatment of root canals have increased significantly.
An “ideal” antiseptic for root canal disinfection must meet the following requirements [7]:
- be bactericidal for microorganisms located in root canals;
- be harmless to periapical tissues;
- do not have a sensitizing effect and do not cause the emergence of resistant forms of microorganisms;
- have a quick effect and penetrate deep enough into the dentinal tubules;
- do not lose its effectiveness in the presence of organic substances;
- if possible, have no odor or specific taste;
- be chemically resistant and remain active during long-term storage.
In modern endodontics, there is no universal remedy that can destroy all the diverse microflora found in tooth tissue.
Classification of drugs for intracanal medicine
Medicines used in endodontics, in our opinion, should be divided into the following main groups:
Group 1 - liquids for washing root canals;
Group 2 - drugs used for antiseptic dressings;
Group 3 - means for chemical expansion of root canals;
A separate group should include drugs for drying root canals and stopping bleeding from root canals, as well as drugs for temporary filling of root canals.
The first group is liquids for washing root canals (irrigators).
Certain requirements are imposed on washing liquids: they must have high bactericidal power, washing and dissolving properties without damaging the periapical tissues. These are, as a rule, nonspecific medications that act not on one type of bacteria, but on associations of microorganisms found in the root canals. They are used during instrumental and final medicinal treatment of the root canal. By removing, destroying microorganisms, or inhibiting their growth during medical and instrumental treatment of the canal, rinsing liquids also dissolve the remains of necrotic pulp from the lateral and additional tubules that are inaccessible for instrumental treatment. They clean the canal walls well from dentinal filings, which can clog the lumen of the root canal during instrumentation. Some rinsing liquids are also weak bleaches that prevent discoloration of the tooth crown during treatment (for example, 3% hydrogen peroxide solution, 3-5% sodium hypochlorite solutions).
Flushing liquids include:
- halogen-containing preparations, which include chlorine and iodine, i.e. chlorine-containing preparations and iodinol;
- group of oxidizing agents: solution of potassium permanganate, hydrogen peroxide, urea peroxide;
- drugs of the nitrofuran series;
- derivatives of quaternary ammonium compounds;
- proteolytic enzymes, etc.
Products based on sodium hypochlorite:
The range of action of hypochlorite depends on its concentration in the material. When the solution concentration is up to 1%, only necrotic tissue, decay and pus are dissolved. At higher concentrations, the drug affects living tissues, and the higher the concentration of the solution, the stronger the damage to vital cells. A 3% sodium hypochlorite solution is used to dissolve pulp residues after vital extirpation. When a 5% sodium hypochlorite solution comes into contact with tissue proteins, nitrogen, formaldehyde and acetaldehyde are formed within a short period of time. Peptide bonds are broken and proteins dissolve. Thus, as a result of the action of sodium hypochlorite, necrotic tissue and pus are dissolved, allowing the antimicrobial agent to more effectively disinfect the canal.
Dissolution of the remains of mummified pulp after devitalization with strong medications or after thermocoagulation occurs more effectively when using sodium hypochlorite at 5.2% and 10% concentrations. However, it must be taken into account that high concentration sodium hypochlorite can cause destruction of tooth tissue faster than microorganisms. Therefore, in clinical conditions when treating canals, the exposure time of concentrated solutions (5.2% and 10%) should be strictly limited (no more than 60 seconds).
When working with sodium hypochlorite, one should take into account the dependence of the effectiveness of the solution on temperature: at a temperature of 37 degrees C, the activity and speed of disinfection of low-concentrated solutions (0.5-1%) is not inferior to 3-5.2% solutions. To remove the surface smear layer (appearing as a result of instrumental processing of the canal), sodium hypochlorite is used with preparations containing EDTA, which complexes the calcium of dentin, forming a loose structure in the canal. Combined treatment with sodium hypochlorite and EDTA-based preparations ensures effective cleaning of infected canals and their expansion, and also significantly improves the adhesion of filling materials to the canal walls.
By diluting a 10% solution of sodium hypochlorite with distilled water in a ratio of 1:2, you can obtain a solution of universal use - 3.3%. It should be noted that solutions of sodium hypochlorite are very unstable and are stored in the dark and cold. Shelf life at room temperature is up to 2 months, and in the refrigerator - up to 6 months. Stabilized drugs, when properly stored, are effective for a year.
Today, the range of sodium hypochlorite-based products offered by manufacturers is represented by the following drugs.
1. HYPOCHLORANE-3 (“Omega-Dent”). Sodium hypochlorite solution 3.25% for root canal treatment.
2. HYPOCHLORANE - 5 (“Omega-Dent”). Sodium hypochlorite solution 5% for root canal treatment.
3. SODIUM HYPOCHLORITE 3% solution (“VladMiVa”).
Method of using these solutions: draw the required amount of solution into the syringe and rinse the canal (introduce the needle into the canal, not bringing it to the apex 3-5 mm, since the injected solution enters the canal under a certain pressure), or apply the solution to a cotton swab and inject into the channel. Repeat the operation 3-4 times until a “clean” turunda is obtained after removal from the canal. Sequential treatment of the canal with a solution of sodium hypochlorite and a liquid for chemical expansion allows you to pass through almost any difficult-to-pass canal. The residence time of the hypochlorite solution in the canal should not exceed 5 minutes
4. BELODEZ (“VladMiVa”). Dental material based on a stabilized sodium hypochlorite solution for chemical expansion and antiseptic treatment of tooth root canals. Available in liquid (3%, 5.2% and 10%) and gel (3%) form.
5. PARCAN (“Septodont”). Highly purified sodium hypochlorite solution, stabilized, capped and ready for use. A 3% concentration makes it possible to achieve a good chemical and bactericidal effect without a cytotoxic effect at the apex level. Method of use: draw 10 ml of solution into the PARKAN KIT syringe, then insert a needle specially provided for this into the canal and begin to rinse them.
Products based on chlorhexidine.
Chlorhexidine is one of the most active local antiseptics. It has a rapid and strong bactericidal effect on gram-positive and gram-negative bacteria. In particular, it has high activity against the microflora of the root canals of teeth. The drug is stable and after tissue treatment remains there for some time, continuing to have a bactericidal effect.
Retains activity (albeit somewhat reduced) in the presence of blood, pus, various secretions and organic substances. In dentistry, it is used for applying antiseptic dressings in the form of a 0.2% alcohol solution.
Compared to phenol derivatives, chlorhexidine has a milder and physiological effect on periapical tissues (therefore, there is no need to include anti-inflammatory drugs or steroid hormones in the drug).
Allergic reactions and tissue irritation are extremely rare. An important property of chlorhexidine for dental practitioners is that it does not disrupt the polymerization of composite materials.
It is not recommended to use chlorhexidine with sodium hypochlorite preparations.
1. BELSOL (“VladMiVa”). The Belsol set of dental liquids is intended for antiseptic and preventive treatment of the oral cavity. “Liquid No. 2” (chlorhexidine digluconate 2%) - intended for preventive rinsing and antiseptic washing of the mucous surface in case of gingivitis and initial forms of periodontitis, as well as for washing infected root canals.
2. R4 (“Septodont”). 20% solution based on chlorhexidine digluconate for antiseptic treatment of root canals.
Method of application: after mechanical treatment and washing of the root canal, insert a drop of R4 into the canal using a pipette, apply a cotton ball, and seal with temporary cement.
Iodine-based products.
One of the drugs in this group, IODINOL, is a product of the addition of iodine to polyvinyl alcohol and has a dark blue color. The drug has a pronounced bactericidal and fungicidal effect, stimulates the protective forces of periodontal tissues and accelerates their reparative regeneration. Due to the combination with polyvinyl alcohol, active iodine is released gradually, providing a prolonged therapeutic effect. In addition, the irritating effect of iodine on tissue is reduced.
In endodontics, iodinol is used for medicinal treatment of root canals, and also as an indicator of the cleanliness of the root canal, since it becomes discolored upon contact with media containing tissue decay products and pus.
Another drug in this group, iodonate, is an aqueous solution of a complex of a surfactant with iodine. Contains about 4.5% iodine. Has bactericidal and fungicidal effects.
Oxidizing agents.
Washing liquids can also include a 3% solution of hydrogen peroxide. Upon contact with living tissue or organic matter, hydrogen peroxide immediately dissociates into molecular oxygen and water. The rapid release of gas bubbles, which have a weak bactericidal effect, promotes mechanical cleaning of the canal from necrotic tissue and dentin chips. As a good hemostatic agent, a 3% solution of hydrogen peroxide is successfully used to stop bleeding after vital extirpation of the pulp. However, hydrogen peroxide does not have the ability to dissolve necrotic tissue and other organic debris.
To enhance the cleansing and bactericidal effect of solutions of sodium hypochlorite and hydrogen peroxide, it is recommended that they be used alternately when washing the canal. A violent reaction occurs between these solutions with the release of free oxygen and chlorine, as a result of which microorganisms are destroyed and washed out of the canal.
Among the drugs of the nitrofuran series , 0.5% solution of furatsilin, 0.1-0.15% solutions of furadonin, furagin and furazolidone are used in endodontics.
To wash root canals in the treatment of periodontitis, aqueous solutions of quaternary ammonium compounds - 0.1% decamine solution and 0.15% decamethoxin solution, and as antiseptic dressings - 0.1% decamine solution or 0.08% decamethoxin solution.
Methods of drug treatment of canals:
— manual
- ultrasonic
— sound (EndoActivator)
— laser (the solution is activated by a laser)
— hydrodynamic (RinzEndo, EndoVac)
There are several methods of manual medicinal treatment of canals [1]:
- antiseptic treatment using a cotton wool wound on a thin root drill and moistened with a solution of a medicinal substance;
- antiseptic treatment using paper points moistened with a solution of the drug;
- washing the root canal with a solution of a medicinal substance from a syringe through a special endodontic needle.
Traditional irrigation methods using a syringe and endodontic needle provide satisfactory treatment of the coronal and middle third of the root canal, but are not sufficiently effective in terms of cleaning its walls in the apex area. For successful irrigation, it is necessary that the disinfectant solution be delivered to the entire working length of the root canal. This is not always possible to achieve with the help of classic endodontic syringes and needles, since in narrow root canals, due to surface tension, the irrigation solution does not reach the apex, leaving a so-called “air bubble”. As a result, the apical part of the root canal remains insufficiently processed.
There are a number of simple rules and techniques that can make syringe irrigation more effective and predictable. The effectiveness of this type of irrigation is limited to a distance of 3-4 mm from the tip of the needle. An important point is the movement of the needle during administration of the irrigation solution, as well as the position of the syringe. The irrigant should be withdrawn slowly, carefully, while the needle should make back-and-forth movements. It is recommended to press on the syringe piston with your index finger rather than your thumb, as this significantly improves tactile control. The depth of needle penetration, in turn, is determined by the size of the apical preparation, the taper of the canal and the diameter of the needle.
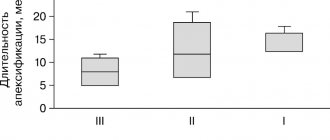
The optimal apical preparation size for effective irrigation should be 30, 40 ISO. The diameter of needles is usually measured in units called gauge. The most commonly used needle is size 27 (see table).
| In gauge | In millimeters |
| 23 | 0,57 |
| 25 | 0,45 |
| 27 | 0,36 |
| 29 | 0,28 |
| 30 | 0,25 |
Thin Endo-Eze Tips and NaviTip (“Ultradent”) needles have a diameter of 29 gauge (0.28 mm), which allows you to advance the needle as far as possible to the apex. Important characteristics are the flexibility of the needle and the ability to pre-bend it when working in a canal with pronounced curvature.
To increase the effectiveness of manual (performed with a syringe) irrigation, a gutta-percha pin can be used, which mechanically activates the irrigant in the pulp cavity and root canals.
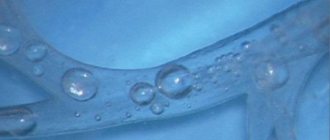
An effective method of activating the irrigation solution is the use of passive ultrasonation. In this case, a thin wire or a small file (ISO No. 15 or 20) is inserted into the root canal filled with solution. Ultrasonic vibrations and the energy of the file are transferred to the liquid, which causes the occurrence of so-called acoustic cavitation. In the cavitation region, powerful hydrodynamic micro-shock waves and micro-flows arise. In addition, the collapse of bubbles is accompanied by strong local heating of the liquid and the release of gas. If sodium hypochlorite is used as a solution during passive ultrasonic irrigation, its antibacterial effect is significantly enhanced. In addition, local temperature increases play an important role. Thanks to these effects, dentinal filings, pulp tissue and intracanal biofilm are removed.
In addition to ultrasonic energy, sound vibrations are also used to activate the irrigant solution in the root canal. Sound devices, compared to ultrasonic devices, generate vibrations of lower frequency but greater amplitude. As a result, the point contact of the sonic tip with the wall of the root canal does not actually affect the effectiveness of its operation, unlike ultrasonic tips.
To improve the quality of treatment of the apical third of the root, the RinsEndo system (Durr Dental, Germany) was also developed. RinsEndo is a handpiece that screws onto the turbine drive of the dental unit and uses compressed air pressure to propel the irrigant solution into the apical part of the root canal. A study conducted by V. Mauser et al demonstrated the high efficiency of cleaning the root canal walls using this system compared to traditional manual syringes. At the same time, this work showed that the use of the RinsEndo tip significantly increases the likelihood of the irrigation solution being removed beyond the apex (80% versus 13% when using a conventional syringe), which is especially dangerous when using sodium hypochlorite solution as an irrigant due to the possibility of serious complications. complications.
Another option for solving the problem of insufficient cleaning of the apical third of the root canal is the use of systems with simultaneous aspiration of the injected irrigant. An example of such a system is EndoVac (“Discus Denial”). The principle of operation of the EndoVac system is based on the movement of the irrigation solution by creating negative pressure in the root canal. One of the nozzles, which supplies the irrigation solution, is inserted into the tooth cavity to a shallow depth, while the other cannula, which performs aspiration, is inserted into the root canal to its entire working length. As a result, the supplied solution, due to negative pressure, penetrates the entire working length of the root canal without the risk of being carried beyond the apex.
A relatively new and interesting trend in root canal irrigation is photoactivated disinfection (PAD or POT). The essence of the method is the introduction of a special dye - a photosensitizer - into the root canal, followed by irradiation using low-power laser radiation with a certain wavelength. Light-sensitive dye molecules attach to or even penetrate the bacterial cell membrane. Then, under the influence of laser radiation with a certain wavelength, a chain of chemical reactions is started, which results in the formation of free radicals. These active radicals cause disruption of the integrity of the bacterial cell wall, inactivation of bacterial toxins, degradation of essential proteins and DNA molecules, resulting in the death of the bacterial cell. The key point of this technique is the direct contact of photosensitizer molecules with the bacterial cell and its penetration into the bacterial biofilm.
The second group is drugs used for antiseptic dressings.
An important role in the disinfection of canals is played by antiseptic dressings, which are left in the root canals for the period between visits. When the infected canal contents are removed, the remaining living microorganisms are deprived of a nutrient medium and become susceptible to mild, non-irritating medications. Such drugs create conditions unsuitable for the life of microorganisms, and thereby favor the action of the protective mechanisms of periapical tissues. Since a significant portion of microorganisms are removed during instrumental and medicinal treatment, the concentration of antiseptic in antiseptic dressings should not be too high. The purpose of antiseptic dressings is primarily to destroy or reduce the remaining bacterial flora of the main canal, deltoid zone and additional canals, actively act on the remains of the pulp, prevent or reduce pain, reduce the inflammatory process in the periodontium and stimulate its restoration.
Antiseptic dressings include essential oils, nonspecific medications, specific medications, mixtures of nonspecific medications with specific ones, and other medications.
The most widely used essential oil is eugenol, which is a chemical derivative of clove oil related to phenol. Apparently, this relationship explains the distinct irritant effect of eugenol on living tissues, in particular on periodontal tissue, accompanied by their infiltration by leukocytes and bone tissue resorption. At the same time, clove oil does not cause a pronounced pain reaction in the tissue.
Non-specific means. These are common protoplasmic poisons with variable antimicrobial properties. Most of them are liquids with relatively low surface tension. As the name suggests, they destroy a large number of bacteria and yeast-like fungi in accordance with the individual strength of the medicine. Typical representatives of nonspecific drugs that were widely used for endodontic treatment were drugs from the phenol group. Currently, they are not used separately, with the exception of camphorophenol. However, they should be mentioned due to the fact that most of these drugs (formocresol, camphor parachlorophenol, cresatine) are part of proprietary antimicrobial agents and mixtures with specific medications currently used.
Products based on camphor and thymol:
1. ANTISEPTINE (“Omega-Dent”).
Method of application: after removing the infected pulp, carefully widen the canal using chemical and endodontic methods. Dry the canal thoroughly by placing a turunda in it and leave for 1 - 3 days, hermetically closing the cavity with a temporary bandage. During the next visit, the patient can have a permanent filling installed.
2. CAMPHOPHENE (“Omega-Dent”).
After using the 'arsenic' paste and before using the 'camphorphene' liquid, the remaining arsenic anhydride should be neutralized with an aqueous solution of iodine for 30 seconds.
3. CRESODENT (“Rainbow-R”).
Dental liquid CRESODENT does not irritate periapical tissues provided it is not mixed with other substances. Due to the low coefficient of surface tension, the drug is volatile and quickly penetrates into the dental tubules, prolonging the bactericidal and fungicidal effect.
4. CRESOPHENE (“Septodont”).
Method of application: after thorough instrumental treatment, place a turunda inside the canal, moistened with a solution and wrung out well to avoid introducing excess amounts of the drug, seal with temporary cement for 3 to 5 days, if necessary, repeat the procedure after removing the contents of the canals and their instrumental treatment using classical methods.
5. CRESODENT-LIQUID (“VladMiVa”). Available in the form of a liquid and a ready-to-use paste on a single antiseptic base. To quickly and effectively reduce pain reactions, an active corticosteroid - dexamethasone (0.1%) was introduced into the liquid, which has a strong anti-inflammatory and anti-allergic effect. The drug does not irritate periapical tissues provided it is not mixed with other substances. Due to the low coefficient of surface tension, the drug is volatile and quickly penetrates into the dental tubules.
6. MEPACYL (“Pierre Rolland”).
Method of application: after the pulp cavity has been opened, place a cotton swab soaked in the preparation and well wrung out into it. Place a temporary filling made of sealed cement without pressure for 3-5 days. Repeat the procedure after passing and expanding the canals using appropriate tools.
Phenol-based products:
1. GUAYAFEN (“Omega-Dent”).
Indications:
— antiseptic treatment of root canals for complicated caries of the fourth degree, after removal of the canal contents.
— mummification of branched nerve fibers after devitalization with 'arsenic' paste.
— disinfection of root canals after a cyst, abscess, fistula.
— as a liquid for hardening paste based on zinc oxide for filling root canals.
2. ROCKLE'S (“Septodont”).
ROCKLE'S No. 4 is a solution with a high formaldehyde content. Antiseptic treatment of root canals for the conservative treatment of periodontitis, cystogranulomas, radicular cysts, abscesses in the form of a hardening paste based on zinc oxide for filling; mummification of nerve fiber branches after devitalization with arsenic anhydride.
ROCKLE'S No. 8 is a solution with low formaldehyde content. Antiseptic treatment of carious cavities with medium and deep caries, canals after amputation and pulp extirpation - in the form of a hardening paste based on zinc oxide for filling root canals.
3. OSOMOL 3, OSOMOL 4 (“Pierre Rolland”).
Method of application: after the pulp cavity has been opened, place a cotton swab soaked in the preparation and well wrung out into it. Place a temporary filling using sealed cement without pressure. Leave in the cavity for 3-5 days. Repeat the procedure if necessary.
The third group is means for chemical expansion of channels.
To facilitate the passage and expansion of narrow and obliterated root canals during instrumental treatment, complexons or so-called chelates with an affinity for alkaline earth metals are used. Expansion of the canal using chelates is based on their ability to form complex compounds with dentine calcium, as a result of which the latter goes into solution. As a result of this reaction, the walls of the root canal are decalcified and softened, which facilitates the process of instrumental treatment of the root canal. Complexones are non-toxic, easy to use, do not require special storage conditions, and remain active for a long period of time [4].
The pre-marked tool should be curved to facilitate passage. Then the instrument is lubricated with gel, inserted into the canal, and mechanical treatment is carried out with the prepared file. Alternately, you should irrigate the root canal with a solution of sodium hypochlorite and perform mechanical treatment of the canal with a file lubricated with gel. During irrigation with sodium hypochlorite, foam will form, which will help remove the contents of the canal. You cannot leave the gel in the canal until the next visit. Finally, it is necessary to thoroughly rinse with water and dry the canal with a liquid for drying and degreasing the root canals, after which you can begin filling.
Today, the range of EDTA-based products on the dental market is represented by the following drugs.
1. EDETAL (“Omega-Dent”)
2. Liquid for chemical expansion of root canals (“Omega-Dent”).
3. CANAL-DENT (“VladMiVa”), (gel).
4. KANAL-DENT (“VladMiVa”). A set of liquids for canal treatment.
The endodontic set of liquids KANAL-DENT includes:
- liquid for identifying the mouth of canals and chemical expansion of canals, which contains a salt of ethylenediaminetetraacetic acid;
- liquid for antiseptic treatment of canals containing glutaraldehyde.
5. ENDOGEL (“VladMiVa”).
The dental set "EndoGel" consists of: - gel No. 1 based on EDTA; — gel No. 2 containing EDTA and peroxide;
Gel with peroxide (10%) when used together with a sodium hypochlorite solution promotes foaming in the canal (active release of atomic oxygen), removal of living and necrotic, as well as infected pulp tissue, dentinal filings, improves the color and shine of teeth through whitening.
6. ENDOZHI (“VladMiVa”).
Liquid No. 2 for identifying the mouth of the canals and their expansion, contains a mixture of potassium and sodium salts of EDTA (17%) and centimonium bromide - a surface-active antiseptic that provides foaming, rapid penetration of the drug into the microtubules and prevents the settling of dentinal filings, which facilitates their removal from channel;
7. CHANNEL+ (“Septodont”).
8. LARGAL ULTRA (“Septodont”).
LARGAL ULTRA solution contains four-component ammonium with a strong bactericidal effect and a chelate compound that forms complexes with various oligo-elements responsible for the growth of bacterial flora, including them in compounds that cannot be assimilated by microorganisms.
9. EDTA 18% SOLUTION (“Ultradent”). 18% low viscosity, water-based chelate liquid (EDTA) solution contains a surfactant for better chemical expansion of channels.
10. File-Eze (“Ultradent”). Gel for expansion of channels. Available in 1.2 ml and 30 ml syringes.
11. EDETAT (“Pierre Rolland”).
Contains a quaternary ammonium compound for better wetting of the dentinal wall, as well as soapy properties to avoid the deposition of tartar at the apex of the tooth root, improving their removal from the canal.
12. RC-PREP (“Premier”).
RC-PREP is available in the form of a gel in a syringe of 9 g of the drug. The drug is harmless to inhalation, non-toxic, non-carcinogenic, non-volatile and non-flammable.
Conclusion
Concluding the characteristics of intracanal medications, it should be noted the need to remove the smear layer, which is formed when the endodontic instrument comes into contact with the wall of the root canal during instrumentation.
As shown by the results of electron microscopy [4], the removal of the smear layer leads to the opening of the dentinal tubules, the dissolution of the mineral components of intertubular dentin, giving its surface microretaining characteristics. The better the dentin surface is cleaned from the smear layer, the more dentinal tubules open, the more effective the penetration of medications into the dentinal tubules by direct contact with the walls of the root canal.
In light of the latest data on the smear layer and the importance of antiseptics in its removal, it seems that most traditionally used washing liquids should be abandoned, reducing this group to four solutions:
1) 3% sodium hypochlorite solution,
2) 15% EDTA solution,
3) 3% hydrogen peroxide solution,
4) distilled water.
Although a 15% EDTA solution belongs to the group of drugs for chemical expansion of root canals, it can safely be classified as a rinsing liquid, since without its joint participation with sodium hypochlorite, the smear layer cannot be removed. A 3% solution of hydrogen peroxide is usually used as an antiseptic with weak bactericidal properties and as a hemostatic agent. Distilled water is necessary at the final stage of rinsing the canal as a neutralizer for sodium hypochlorite.
At the same time, against the background of the combined use of sodium hypochlorite, EDTA and hydrogen peroxide, the role of intracanal antiseptic dressings in disinfection of the root canal and their therapeutic effect on periapical tissues increases significantly. This method of washing root canals opens up the possibility of fully carrying out the adhesive technique without the use of an etching gel.
Ruvinskaya G.R., Fazylova Yu.V., Yavgildina D.A.
Kazan State Medical University
Guzel Renatovna Ruvinskaya – Candidate of Medical Sciences, Assistant at the Department of Therapeutic Dentistry
Literature:
1. Bolyachin A.V., Belyaeva T.S. Basic principles and methods of irrigation of the root canal system in endodontics // Clinical endodontics. - 2008. -T.2, - No. 1-2. — P.45-51.
2. Cohen S., Burns R. Endodontics: Trans. from English - St. Petersburg, 2000.
3. Krammer I., Schlepper H. Guide to endodontics. User of endodontic instruments. Per. from German - M., 1999. - 96 p.
4. Makeeva I.M., Pimenov A.B. Root canal smear layer and removal Endodontics today. - 2002. - T.2, - No. 1-2. — P. 5-10.
5. Nikolaev A.I., Tsepov L.M. Practical therapeutic dentistry. - St. Petersburg, 2001. 390 p.
6. Pimenov A.B. Areas of root canals inaccessible for instrumentation // Endodontics today. - 2003. - T.3, - No. 1-2. - pp. 23-25.
7. Poltavsky V.P. Intracanal medicine: Modern methods. - M.: Medical Information Agency LLC, 2007. - 88 p.
8. Information materials from the companies VladMiVa, Omega-Dent, Raduga-R, Pierre Rolland, Septodont, Ultradent, Discus Denial, Durr Dental.
Temporary canal filling
If indicated, the doctor can fill the canals after depulpation not with filling material, but with a medicinal agent (antibacterial, anti-inflammatory). The drug remains in the tooth cavity for a certain time, after which it is removed, and the vacated canal is sealed.
The procedure can be prescribed:
- if there is a need to sanitize the canals if a deep infectious process is suspected;
- if the patient has acute periodontitis;
- for temporary sealing of the canal, if it is necessary to monitor the condition of the tooth cavity after removal of the inflamed pulp.
In addition, the procedure can be prescribed for tooth injuries, for example, a fracture of the crown or root.