The condition of the oral mucosa serves as an indicator of the condition of the body: teeth, gums, and internal organs. Therefore, a visit to the dentist is an integral part of a medical examination, which should be carried out at least once a year. Thanks to a visit to a dental specialist, cancer, leukoplakia, stomatitis and other dangerous diseases can be detected in the early stages.
Dentists not only treat teeth, but also carry out sanitation of the oral cavity to identify various diseases that can develop on the oral mucosa.
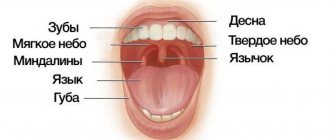
An oral examination should include:
- careful visual examination of the lips, buccal mucosa, gums, anterior part of the tongue, floor of the mouth and palate;
- examination of the throat (pharynx), including tonsils, root of the tongue;
- palpation of the jaw and neck to detect nodes, tumors, any abnormalities or abnormalities.
During the examination, it is possible to promptly detect foci of inflammation of the oral mucosa (OM), including erosions, ulcers, compactions, and also pay attention to the condition of the lymph nodes.
Among the most popular diseases of the oral cavity is stomatitis. Stomatitis is an inflammation of the oral mucosa. This disease is characterized by all the signs of an inflammatory process: redness, pain, swelling, dysfunction, increased local and general body temperature. Acute herpetic stomatitis accounts for 85% of all diseases of the oral mucosa; chronic recurrent aphthous stomatitis is also common.
Aphthous stomatitis is a disease in which one or more round ulcerations appear on the oral mucosa, which are covered with a necrotic coating of a gray or yellowish tint. Such ulcers (aphthae) are not the result of acute infections and are therefore not contagious.
In addition to these oral diseases, the following are gaining popularity: leukoplakia, candidiasis, and lichen planus.
Leukoplakia looks like a red border of the lips of foci of keratosis in the form of whitish compactions. With candidiasis, spots of white plaque of a loose consistency appear on the oral mucosa, which are easily removed with a spatula. With repeated bacterial infection and erosion, the plaque may have a brownish tint. Gray-white spots are a sign of lichen planus of the oral mucosa. They form on the tongue, gums and on the inside of the cheeks. This disease is similar to others, namely leukoplakia, so a visual examination is not enough.
Current trends, according to dentists, are extremely negative. Due to alcohol consumption and smoking, the number of cancer cases is only increasing. Therefore, examination of the oral mucosa is very important, as it helps to detect cancer in the early stages and begin treatment that will not be too aggressive for the body.
Types of pathologies of the oral mucosa
- Mechanical damage that can occur when the mucous membrane is exposed to poorly installed fillings, dentures and other solid objects, including solid food. The damage appears as scratches and may bleed.
- Thermal injuries occur when eating very hot food or drinks. A whitish spot appears at the burn site, from which the skin begins to peel off.
- Chemical injuries occur when eating hot, spicy foods, or when taking certain medications.
Standards for a healthy oral cavity
Home / Articles / Standards for a healthy oral cavity
How is oral health determined? A healthy oral cavity is the absence of diseases, inflammations and pathologies. Orthodontist Farida Yusifovna Gasimova talks about the health standards of the oral cavity and dental system.
— Farida Yusifovna, how is dental health determined?
— Disorders in the dental system provoke malfunctions in the joints and muscles. Fixation of the lower jaw is carried out with the help of the muscles of the head and neck; the chewing process occurs when the temporal and masticatory muscles work. If the chewing apparatus is functioning correctly and the joints and muscles are anatomically normal, there is a distance (2 mm) between the teeth of the upper and lower jaws. Disturbances in the bite occur with excessive muscle tone in a calm state, which affects not only the teeth, but also general well-being: the patient complains of frequent headaches, pain in the neck muscles, in the back, there is pinching of the facial muscles, teeth are subject to wear, chips appear at the ends, and a wedge-shaped defect is often diagnosed. Disturbances in the dental system can be of a different nature; based on external symptoms, one can more or less understand that it is necessary to consult an orthodontist. If the patient notices stiffness when moving the lower jaw, jamming of the jaw, characteristic clicks when it moves (crunching, clicking) - this indicates problems with the temporomandibular joint. The action of the TMJ (temporomandibular joint) is aimed at ensuring normal movement of the lower jaw. The temporomandibular joint looks like a dimple with a head, with an articular disc placed between them. The absence of disturbances is manifested in the form of the location of the head in the fossa (resting state). When the jaw moves, the head is displaced by the articular disc. If there are disorders, the articular disc is displaced, the bite is disturbed and the jaw moves incorrectly. Dysfunction of the TMJ (temporomandibular joint) requires complex treatment from doctors of various specialties, including a gnathologist, an orthodontist, and a neuromuscular dentist. The condition of the dental system is significantly influenced by the patient’s spine and posture. If posture is impaired, the muscles of the face, neck, and back cannot work correctly, and this fact, in turn, affects the normal functioning of the lower jaw. The displacement of the lower jaw causes disruptions not only in the functioning of the dental system, but also in the body as a whole. An anatomically correct bite is not an indicator of a healthy dental system, as many patients think. Just like white, straight teeth. The dentofacial system generally cannot be characterized by any one of its organs, since, as I have already said, a violation in any of its components affects the entire system. The condition of the dental system is directly related to the work of the ear organs, temporomandibular joints, neck and head muscles. The psycho-emotional state of the patient also plays an important role. If pain in the neck and back periodically appears, this already indicates an existing disorder, including in the dental system. Therefore, only a dentist orthodontist in Anapa can determine its condition.
— What is the dental system?
— The dentofacial system is a complex apparatus in which the organs are anatomically united. The organs included in the dental system are bones (palatine, zygomatic, nasal, jaw), teeth, temporomandibular joints (temporomandibular joints, lips, cheeks, tongue, soft and hard palate, salivary glands, masticatory and facial muscles. Functioning separately and together, all these organs give us the opportunity to breathe, talk and eat food. I want to emphasize that in the dental system there are no “important” and “minor” organs, each individual component of the system plays its role. The growth and formation of the dental system begins in changes in the womb and throughout a person’s life. From childhood to final adulthood, modifications of the dental system are clearly noticeable, since during this period the bite changes, individual features of the cheekbones, tongue, and lips are formed. Then the changes are little noticeable, but they continue to occur. When there is a process of active formation (childhood), the Anapa orthodontist dentist can quickly correct the incorrect growth trend to an anatomically correct one, direct the growth of teeth and bones, so to speak, in the right direction. You should not wait until the jaw is fully formed (adulthood) for orthodontic treatment; in children, therapy is faster, easier, and cheaper. Dentistry Millennium Anapa Mayakovsky offers patients orthodontic services. It is also important to note the fact that a disorder in one organ inevitably affects the functioning of the entire system, therefore, if the pathology is not corrected during the period of formation and growth of the jaws, it can develop into a severe disorder in adulthood. It is necessary to undergo an examination by an orthodontist during the period of 5-7 years, which will exclude or identify a tendency to disrupt the development of the dentofacial system. A pediatric orthodontist in Anapa conducts a visual examination and diagnosis using special equipment. I repeat, it is much easier to carry out correction in a child than long-term therapy in an adult patient.
— Farida Yusifovna, how are teeth treated today?
— Treatment of the dental system must be carried out comprehensively, with mandatory visits to specialized specialists. Anapa Mayakovsky Dentistry Millennium dental treatment, in the clinic you can get a consultation with one of the best dental specialists in the city and undergo a full diagnosis of the dental system. Depending on the patient’s clinical picture, the orthodontist in Anapa prescribes consultations with doctors and computed tomography. Therapy of the dental system is always carried out according to an individual program; in case of violations, it is impossible to treat everyone according to the same scheme. Electromyography (myography) is used to identify dysfunction of the masticatory and temporal muscles and determine the affected nerve areas. Using electromyography, it is possible to determine the causes of paralysis of an individual muscle. The principle of operation of the myograph is that it records changes in the bioelectrical activity of muscles using special sensors attached to the facial muscles and connected to the myograph. Therapy of the dental system includes treatment with an occlusal guard and a splint (a removable device for correcting the bite). With the help of a mouthguard, pain in the TMJ, pinching of the lower jaw, headaches and other disorders are eliminated, the action of the occlusal splint is aimed at restoring the natural position of the muscles during the functioning of the jaw, with the help of the splint the symmetry of the face and anatomically correct muscle tone are restored. Another technique that deserves attention is electrical neurostimulation (TENS), the effect of which is aimed at relaxing the masticatory muscles that are in hypertonicity. This method effectively eliminates muscle spasms, saturates tissue cells with oxygen, ensures the correct position of the lower jaw, removes lactic acid, and restores proper muscle function. TENS therapy is carried out using a current that is passed through the patient's skin; the entire procedure takes about one hour. The facebow is used to accurately analyze the individual position of the jaws in three dimensions in order to then produce a prosthetic structure (veneers, dentures or crowns). The use of this mechanical device in dentistry can significantly reduce errors in the design of orthopedic devices. Making a structure for the dental system is a rather complex task that requires maximum attention, experience and professionalism; not only the individual characteristics of the position of the bones are taken into account, but also the dynamics of movement. When making orthopedic structures, it is very important to match the central occlusion and jaw relationship. When conducting therapy, dentists set themselves the priority tasks of restoring proper functionality, and only then the aesthetic factor. Of course, most patients are primarily interested in the beauty of a smile, but if beautiful teeth are not capable of fully chewing food, then, of course, it is much more important to recreate functionality.
Comprehensive hygiene for 2500 rubles! Air Flow 1000p for patients with braces!
A unique promotion for our regular patients! A set of hygienic procedures (removal of tartar and plaque using Air Flow and ultrasound , scaling, polishing, fluoridation) for regular patients once every 6 months for RUB 3,000!
Air Flow and polishing for only RUR 1,500 for patients with braces!
Diseases characteristic of the oral cavity
- A viral infection that includes herpes. This disease affects up to 90% of the world's population. The herpes virus can be present in the human body in a latent form for a long time and only appear if the person is under stress or has a cold.
- An infectious and inflammatory disease, which includes pharyngitis - inflammation of the pharyngeal mucosa. The disease can be triggered by inhaling tobacco smoke or any chemicals. Stomatitis. This disease can be caused by mechanical damage to the mucous membrane, after which ulcers appear on it.
- Fungal diseases. The causative agent is a fungus that can be present in the body for a long time and become active only when the immune system is weakened. Fungal diseases include thrush, which manifests itself as whitish spots on the mucous membranes and lips. Atrophic candidiasis is the most common type of fungal disease. The patient feels dry, and redness appears in the oral cavity and a burning sensation may begin.
Other diseases include disc bacteriosis of the oral cavity. It can occur after long-term use of antibiotics.
Medical Internet conferences
Scientific supervisors: associate, Ph.D. Petrova A.P., ass. Venatovskaya N.V.
Relevance. All over the world, there is an annual increase in the number of people suffering from diseases of the gastrointestinal tract and hepatobiliary system [5]. The overall morbidity rate of the population of the Russian Federation in the class “Diseases of the digestive organs” increased from 99 per 1000 population in 1996 to 112 per 1000 population in 2010 [2,8]. At the same time, early diagnosis of these diseases is currently a priority medical and social task due to the fact that in the absence of timely treatment they often develop into more severe, chronic, incurable forms. Therefore, assessment of the general patterns of structural and functional reorganization of various parts of the digestive tract when pathological processes occur in them has great diagnostic and prognostic significance [1,6,13]. As you know, the oral cavity is a kind of mirror of the body. Changes in it reflect the patterns of the pathogenesis of systemic pathology and are caused by the etiological, pathogenetic, morphological and functional integration of all systems of the human body [14]. The results of numerous clinical studies in this area indicate that when the function of the gastrointestinal tract organs is impaired, damage to the oral mucosa is simultaneously observed, and there is also a risk of an unfavorable course of the existing chronic inflammatory process [4,10,18]. This relationship is explained by their anatomical and physiological proximity, common innervation and humoral regulation [11]. Therefore, knowledge of the characteristic pattern of manifestations of certain general somatic diseases in the oral cavity, in particular gastrointestinal diseases, and the ability to diagnose pathology is the most important professional quality of a dentist. This would greatly help in identifying systemic diseases at their earliest stages so that the patient can be referred immediately to an appropriate specialist.
Purpose: to find out whether there is a correlation between diseases of the gastrointestinal tract and their indirect manifestations on the oral mucosa.
Tasks:
1) study the anatomical and physiological structure of the oral mucosa, as well as identify similarities with the structure of the mucous membrane of the gastrointestinal tract;
2) determine which symptoms are more often observed in the oral cavity in patients with concomitant pathology of the digestive organs;
3) establish the relationship between changes in the oral cavity and specific gastrointestinal diseases;
4) identify the complex of morpho-functional disorders in the oral cavity characteristic of gastritis and gastric ulcer.
Materials and methods. An examination of the oral cavity of patients from the gastroenterology department who were undergoing treatment at the Road Clinical Hospital in the city of Saratov was carried out. The study involved a group of people with gastritis and gastric ulcer, consisting of 19 people aged from 43 to 66 years, of which 15 were men and 4 women. A literary review of periodicals, scientific papers, and library sources in Russian and English on the topic of diagnosing pathology of the gastrointestinal tract in the oral cavity was also carried out, and some clinical studies in this area were analyzed.
Results and discussion. The oral mucosa is a complexly organized system that has its own distinctive features. It consists of the following components:
1) multilayered squamous epithelium, in which several layers are distinguished: basal, spinous and, in the area of the hard palate, gums, cheeks along the line of closure of the teeth, granular and horny;
2) own layer;
3) submucosa (with the exception of the mucous membrane of the tongue, gums and hard palate).
The blood supply to the oral cavity is carried out mainly by the maxillary artery, which gives off the following branches: the inferior alveolar artery, the buccal artery, the posterior superior alveolar artery, the infraorbital, and the descending palatine. The veins accompany the arteries and flow into the internal jugular vein system. The outflow of lymph is carried out into the regional lymph nodes: mental and submandibular. Innervation of the oral cavity is provided by the II and III branches of the trigeminal nerve, as well as by the branches of the nasopalatine, buccal, lingual, glossopharyngeal and vagus nerves.
SOPR functions:
1) secretory;
2) buffer;
3) barrier (the ability of the epithelium of the oral mucosa to keratinize, immune protection of the mucous membrane);
4) reflexogenic;
5) selective permeability;
6) regenerative.
Most often, changes in the mucous membranes are nothing more than a reflection of the internal problems of the whole organism. The oral mucosa shows early signs of many infectious and non-infectious, acute and chronic, specific and nonspecific processes [12]. Quite pronounced changes in the oral cavity are observed, in particular, in pathologies of the gastrointestinal tract. In patients with diseases of the oral mucosa, diseases of the digestive organs are diagnosed in 75% of cases [15]. It is worth noting that the relationships studied in this article are due to the morphofunctional similarity between the oral mucosa and the gastrointestinal tract.
It is known that the receptor field of the mucous membrane reflexively affects the underlying parts of the digestive tract. However, there is also an inverse relationship. The oral mucosa is an effector field of the reverse influence of “pathological” reflexes from a number of internal organs [9]. At the same time, symptoms in the oral cavity allow for early diagnosis of this pathology even before the development of severe manifest forms. Studies of the initial part of the digestive tract with concomitant gastrointestinal pathology conducted by clinicians have shown that changes in the oral mucosa, as well as their severity, are closely related to the form, severity and duration of the underlying disease [7,16]. Moreover, certain pathological changes can be observed in almost all structures of the oral cavity. Patients with concomitant pathology of the gastrointestinal tract may complain of pain, itching and burning of the tongue, dysgeusia in the form of a sour or bitter taste in the mouth. Objective symptoms include: 1) coating on the tongue; 2) violation of the relief of the tongue; 3) swelling of the mucous membranes and tongue; 4) paresthesia; 5) ulcerative lesions of the oral mucosa; 6) change in color of the mucous membrane.
Tongue disorders rank first in terms of occurrence in gastrointestinal pathologies. Often these changes are noticed by patients themselves. The appearance of the tongue has significant diagnostic value, since it may indicate a hidden gastrointestinal pathology. Most often, plaque is found on the tongue, the severity of which depends on various reasons. The state of the language matters here. Normally, as well as with hypertrophy of the papillae of the tongue, the plaque is dense and quite pronounced. With papillary atrophy, on the contrary, it is absent or insignificant. The reason for the formation of plaque is a disruption of the physiological process of keratinization and desquamation of the epithelium of the oral mucosa, which is observed in pathologies of the gastrointestinal tract. In addition, the severity of self-cleaning processes, the composition of the microbial flora and the hygienic status of the oral cavity undoubtedly also play a role.
Plaque on the tongue is usually found with gastritis, gastric and duodenal ulcers, enterocolitis, and gastric neoplasms. Moreover, during an exacerbation, it is pronounced and covers the entire back of the tongue or mainly its posterior sections. The color of the plaque is grayish-white, but under the influence of pigment-forming microorganisms, food chromogens, and medications, it can take on a different color. However, during the period of remission or during the treatment of the underlying disease, it is possible to completely free the tongue from plaque. Subjective sensations are often not observed, but with an abundant, dense coating, patients note a feeling of awkwardness and dullness of taste perception. It should be noted that plaque can also be detected in other diseases, in particular infectious ones, as well as in healthy people in the morning.
The second most common symptom of diseases of the digestive system is a disorder in the papillary apparatus of the tongue. In persons with hyperacid gastritis, hyperplastic glossitis is observed, in which the papillae are well defined, the tongue is covered with a dense coating and is somewhat swollen. In patients with gastric and duodenal ulcers, only the fungiform papillae hypertrophy, which rise above the surface in the form of bright red dotted formations. Hypoplastic glossitis is manifested by atrophic changes in the papillae, absence of plaque, and the size of the tongue is slightly smaller than average. With pronounced atrophy of the papillae, the tongue takes on a “varnished” appearance, which is often observed with gastritis, peptic ulcers and gastroenteritis. In this case, atrophy of the papillae of the tongue causes a number of subjective sensations in the patient: burning, tingling, feeling of awkwardness, pain when eating. Along with trophic disorders, impaired absorption of vitamins, their breakdown in the intestines, as well as reduced synthesis of vitamins B1, B2 and PP play a significant role in the pathogenesis of the described changes.
Also, with gastrointestinal diseases, patients experience swelling of the tongue and mucous membranes. This condition often does not cause suffering to the patient and is diagnosed by a doctor accidentally during a routine examination of the oral cavity. However, with severe swelling, patients note a feeling of awkwardness, an increase in the size of the tongue, and biting of the cheeks and tongue. Upon examination, tooth marks are revealed on the mucous membranes of the cheeks and tongue. In patients with concomitant pathology of the gastrointestinal tract, edema is confirmed by the McClure-Aldrich blister test, which also helps to identify sick individuals without visible edematous changes in the mucous membranes and tongue and makes it possible to establish the presence of hidden edema, which can serve as an important diagnostic sign in early stages of the disease. Swelling of the tongue and mucous membranes is a characteristic symptom of chronic intestinal pathology: colitis, enterocolitis and is detected in more than 80% of cases. This condition is determined by a violation of the absorption and barrier functions of the intestinal epithelium. In addition, water imbalance also plays a certain role.
Paresthesia of the tongue often occurs in patients with pathology of the gastrointestinal tract. Sometimes a burning sensation and tingling sensation can be observed without visual changes in the tongue. The taste buds of the tongue perform a sensory function and are the effector, end link of the gastrolingual reflex. It is known that normally their number is in correlation with the functional state of the digestive tract. The maximum activity of the receptors is observed on an empty stomach, and after eating, their demobilization is observed. This occurs as a result of centrifugal impulses from the interoreceptors of the stomach to the exteroreceptor apparatus of the tongue and is realized as a normal reaction in healthy people. Some disturbances in taste sensitivity are observed in almost all diseases of the gastrointestinal tract. Thus, with peptic ulcers, several types of functional mobility impairment are noted: there is no demobilization of taste buds after eating; there is a perverse reaction - an increase in the level of mobilization of taste buds after eating; a reaction similar to that observed in practically healthy people [3]. The described disorders are a consequence of changes in the normal reflex relationships of the receptor fields of the tongue and stomach as a result of disorders of the secretory and motor functions of the stomach, which is characteristic of peptic ulcer disease. Decreased taste sensitivity to bitter and sweet is often characteristic of stomach cancer.
Ulcerative lesions of the oral mucosa are nothing more than the result of trophic disorders that occur as a result of pathology of the gastrointestinal tract. This position is confirmed by numerous clinical observations indicating a combination of aphthous stomatitis with diseases of the large intestine, as well as experimental studies on its modeling. With experimental gastritis and enterocolitis, predominantly desquamative and then erosive-ulcerative glossitis develops. And irritation of the large intestine provokes the development of aphthae-like changes in the mucous membranes.
A change in the color of the mucous membrane also indicates gastrointestinal diseases. It has been established that the color of the mucous membrane depends to a certain extent on the type, duration and severity of the underlying disease. Catarrhal stomatitis, manifested in the form of areas of hyperemia or cyanosis, is observed with gastric ulcers, colitis, enterocolitis. In case of complications of gastric ulcer by bleeding, pallor of the mucous membranes is noted.
In our study, we examined a group of patients from the gastroenterology department of the Road Clinical Hospital in the city of Saratov, consisting of 19 male and female people aged from 43 to 66 years with gastritis (6 patients) and gastric ulcers (13 patients). The following results were obtained: patients with gastric ulcer (in the acute phase) complain of burning - 69%, tingling of the tongue - 54%, impaired taste perception - 69%. Objectively: hyperemia of the mucous membranes - 85%, the tongue is covered with a whitish-gray coating - 100%, hypertrophic changes in the fungiform papillae of the tongue are noted - 92%, as well as changes like rhombic glossitis - 15%. According to literary sources, all identified changes in the organs of the oral cavity are in one way or another characteristic of gastric ulcer in the acute phase. Patients with hyperacid gastritis complain of distortion of taste sensations - 33%, the presence of a metallic taste in the mouth - 16%. Objectively: swollen, hyperemic mucosa of the vestibule and the oral cavity itself - 83%, there is a change in the relief of the tongue like a “varnished” type in some patients - 33% and like hyperplastic glossitis in others - 50%, a grayish coating on the back of the tongue - 83% ( Table 1). Note that all the identified changes in the oral cavity of patients with gastritis, with the exception of rhombic glossitis, are also characteristic of this pathology and were described above based on data from a literature review. However, in our study, the sample consists of only 19 people, so it is not possible to transfer the results obtained to the general population and talk about a direct relationship between the identified changes in the oral cavity and a specific pathology due to the low representativeness of the sample. Moreover, at the moment, in the available literature sources, no reliable information has been found on a strict correlation between certain changes in the morpho-functional state of the oral cavity and specific diseases of the gastrointestinal tract. However, in the literature there is a lot of information that there are manifestations in the oral cavity that are more or less characteristic of certain gastrointestinal diseases, which is confirmed by the results of our study.
It should also be remembered that changes in the mucous membranes often reflect the essence not of “pure” pathology of the gastrointestinal tract, but of other disorders of the body that have developed secondarily [17]. Therefore, determining the primary etiological factor that caused the development of certain changes in the oral cavity is one of the key points in the professional activity of a dentist in relation to the diagnosis of the disease.
Prevention of oral diseases
- visit the dental office at least once a year;
- organize a special diet, in which lean meats, fish, fresh vegetables and fruits should predominate;
- rinse your mouth with special compositions after each meal;
- Strengthen your immune system and avoid colds.
To avoid any problems with teeth and oral cavity, you need to regularly visit the dentist and carry out preventive maintenance.
Prevention and treatment of diseases of the oral mucosa
The relevance of the prevention and treatment of diseases of the oral mucosa is due to the high prevalence of this pathology. Depending on the location of the source of inflammation, stomatitis, glossitis, gingivitis, periodontitis, etc. are distinguished.A combination of pathological processes is often observed. The most common diseases of the oral cavity are stomatitis, gingivitis and periodontitis.
Stomatitis
The clinical picture of stomatitis varies depending on the form of the disease.
Allergic stomatitis
characterized by severe hyperemia and moderate swelling of the oral mucosa. Frequently observed itching, burning or dryness may be due to hypersensitivity to a food product or lipstick.
Acute ulcerative-necrotizing gingivitis
, or Vincent's disease, manifests itself as ulcerative-necrotic lesions of the gingival papillae.
For candidiasis
(thrush), caused by the yeast-like fungus
C. albicans
, a white “curdled” coating is observed, rising above the hyperemic mucous membrane. As the disease progresses, the process may spread to the palate, gums, tonsils, larynx, and gastrointestinal tract (GIT). Candidiasis occurs in weakened children and patients with immunodeficiency states, long-term use of antibiotics, corticosteroids and antitumor drugs.
Aphthous stomatitis
, as a rule, is an indicator of gastrointestinal diseases. Factors that predispose to the development of stomatitis are deficiency of iron, vitamin B12, and folic acid. The disease can be triggered by stress or local trauma, and is characterized by the presence of oval erosions (aphthae).
Herpetic stomatitis
manifests itself as painful blistering rashes on the mucous membrane of the mouth and lips. Primary acute herpetic infection develops mainly in children aged 1 to 3 years (70% of children at this age experience acute herpetic stomatitis in one form or another).
For systemic diseases
The following changes in the oral mucosa may be observed: Koplik spots (measles), blisters (erythema multiforme exudative), hemorrhagic lesions (scurvy, platelet pathology), “raspberry” tongue (scarlet fever), hyperemia of the lips and oral mucosa (cutaneous-mucosal lymphadenopathy – Kawasaki disease), etc.
Gingivitis and periodontitis
Inflammatory or destructive changes in the tissues surrounding and supporting the teeth, i.e. Periodontal disease (gums, alveolar processes, cementum) usually begins with gingivitis (inflammation of the gums), which progresses to periodontitis (severe inflammation of the gums up to destruction of the bone tissue of the interdental septa). Periodontitis is the most common cause of tooth loss in adults. It is believed that the cause of this disease is poor oral hygiene.
, resulting in the formation of dental plaque (colonies of microorganisms tightly bound to the surface of the tooth);
local factors: bite pathology, tartar, incorrectly applied fillings, impaired oral breathing
.
Gingivitis often develops due to endocrine changes
in adolescents and pregnant women. In addition, gingivitis, especially in adolescents, may be an early sign of latent diabetes mellitus.
Characteristic changes in the gums with gingivitis include hyperemia, swelling and bleeding with minimal trauma. The inflammation is usually chronic, and without treatment, gingivitis progresses to periodontitis
, signs of which are deepening of the gum pockets, an increase in the amount of tartar, bad breath, weakening of the supporting apparatus of the tooth and the beginning of bone destruction. Reduction of bone tissue is accompanied by loosening of teeth and gum atrophy. Late stages of the disease are characterized by tooth loss.
Treatment
If the underlying lesion of the oral mucosa is a systemic disease, specific therapy is prescribed. It is necessary to eliminate local and general predisposing factors
.
In all cases, careful hygiene and sanitation of the oral cavity
.
For candidiasis, antifungal agents
(for example, nystatin suspension), and for bacterial infections,
antibiotics
.
For extensive painful lesions, rinsing the mouth with a 1-2% lidocaine solution or soda solution
.
Sometimes medical intervention
: removal of tartar, replacement of fillings, surgical plastic surgery of the oral vestibule and frenulum.
One of the local drugs effective in the treatment and prevention of this pathology is Imudon
– immunostimulant of bacterial origin.
Imudon is a polyvalent antigenic complex (lyophilized mixture of dry bacteria), the composition of which corresponds to the pathogens that most often cause pathogenic processes in the oral cavity. Imudon contains the following microorganisms: Lactobacillus acidophilus, Lactobacillus fermentatum, Lactobacillus helveticus, Lactobacillus lactis, Streptococcus pyogenes, Enterococcus faecalis, Streptococcus sanguis, Staphylococcus aureus, Klebsiella pneumoniae, Corynebacterium pseudodiphteriticum, Fusiformis fusiformis, Candida al bicans.
By influencing the immune link of the pathological process, Imudon has the following therapeutic effects:
•
increased phagocytic activity of macrophages;
•
increase in lysozyme content in saliva;
•
stimulation and increase in the number of immunocompetent cells responsible for the production of antibodies;
•
an increase in the content of secretory immunoglobulin A (IgA) in saliva;
•
slowing down the oxidative metabolism of polymorphonuclear cells.
Thanks to its ability to activate the formation of antibodies and stimulate the defenses of the oral mucosa, Imudon enhances the fight against infection and alleviates the patient’s condition.
Imudon acts locally in the oral cavity; there is currently no data on its systemic absorption. Imudon has both therapeutic and preventive effects. Imudon can be used for the prevention and treatment of infectious complications after tooth extraction and implantation of artificial dental roots.
The tablets should be completely dissolved in the mouth. For acute inflammatory diseases of the oral cavity, the drug is taken 8 tablets per day; The duration of treatment is 10 days. For chronic inflammatory diseases of the oral cavity, Imudon is prescribed 6 tablets per day for 20 days. It is recommended to carry out course therapy 2-3 times a year.
When using the drug according to indications in recommended doses, side effects and cases of overdose are currently not described. It should be noted that, if necessary, you can rinse your mouth no earlier than 1 hour after using Imudon. When prescribing the drug to patients on a salt-free or low-salt diet, it should be taken into account that one tablet contains 15 mg of sodium. In women during pregnancy or breastfeeding, the drug can be used according to indications.
In a recent study conducted at the Department of Pediatric Therapeutic Dentistry of Moscow State Medical University (headed by Prof. V.M. Elizarova), Imudon was used in 30 children aged 1 to 3 years with acute herpetic stomatitis. Imudon was prescribed on the day the child visited the doctor, 6–8 tablets per day (the tablet was kept in the mouth until it was completely dissolved), and antiviral therapy was also used at the same time.
Imudon reduced symptoms such as pain, inflammation, and bleeding from the gums. The duration of the course of treatment depended on the severity of the disease: for mild - up to 5-7 days, for moderate - 8-10 days, for severe - 15 days. We confirmed objective clinical observations indicating positive dynamics in the development of acute herpetic stomatitis by examining the content of lysozyme and secretory IgA in saliva.
Thus, in the treatment of acute herpetic stomatitis in children, along with antiviral drugs, it is advisable to use Imudon, which significantly improves the condition of patients.
Imudon can be used along with drugs from other groups without special precautions, since it only acts in the oral cavity and does not interact with other drugs.
Immunostimulant of bacterial origin:
Imudon (trade name)
(SOLVAY PHARMA)
Appendices to the article
| Periodontitis is the most common cause of tooth loss in adults |
The oral cavity, its mucous membrane and lymphatic tissues of the maxillofacial area play a vital role in the interaction of the human body with the environment.
Microorganisms living in the oral cavity, on the one hand, contribute to the digestion of food and the synthesis of vitamins, on the other hand, they form products that damage dental tissue.
A practicing doctor must be fluent in the technique of examining dental patients and, first of all, the oral cavity and teeth. A complete examination of the patient makes it possible to establish not only the localization and nature of the pathological process, i.e., to substantiate the diagnosis, but also to foresee the further course of the disease and its probable outcome. Based on the results of the examination of the patient, the doctor chooses treatment tactics, establishes indications and contraindications for certain therapeutic measures.
Research methods in clinical dentistry include interviewing the patient, examination (both external and oral), examination of the oral cavity and teeth, as well as perimaxillary soft tissues, probing, percussion, and palpation. Methods based on the use of radiography, electroodontometry, laboratory and others are additional, since sometimes the diagnosis can be made without their use. For diseases of the mucous membrane and periodontium, special research methods are used.
SURVEY IN DENTISTRY
Questioning a patient in dentistry is one of the important stages of examining a patient. When interviewing the patient, passport data is clarified and the history of the present disease is clarified. The dentist must listen to the patient, guiding his story in such a way as to find out the most important of his complaints. By asking additional questions, the doctor finds out the nature of the pain, the cause of its occurrence, the duration of the pain, localization, prevalence, and so on.
It is also important to find out living conditions, dietary habits, profession, concomitant diseases, for what reason the missing tooth was removed, and how often you went to the dentist. When communicating, the doctor must carefully monitor the patient’s facial expressions, pay attention to the configuration of the face, how the patient’s mouth opens, whether there is bad breath or taste disturbances. For example, a taste disturbance may occur due to pathology of the central nervous system. All examination data are entered into the dental patient’s medical record.
INSPECTION
After a thorough questioning, the doctor begins the examination, observing the rules of deontology. The examination begins with an external examination of the face and surrounding areas. Facial deformation often indicates the presence of a pathological process not only on the face, but also in the oral cavity. During the examination, the general condition of the patient, the position of the head, skin color, and sclera are also determined. Thus, a yellowish coloration of the sclera can occur with periostitis, acute periodontitis, and necrotizing stomatitis. When conducting an examination, the doctor must pay attention to the patient’s manner of speaking, since a change in speech may occur due to some pathological processes. After a general examination, the dentist examines the oral cavity, carefully examining the contours and corners of the lips (with jaws and lips closed). Then the vestibule of the oral cavity is examined using a spatula. The oral cavity itself is examined using a dental mirror. At the same time, attention is paid to the condition of the salivary glands, hard palate, tongue, and floor of the mouth. After this, they begin to examine the teeth. This study uses a dental mirror, a probe (usually angular), and tweezers. When examining the teeth, the state of the bite, the number of teeth, their color, condition, their shape, size, the presence of periodontal pockets and the condition of the periodontal tissues are determined.
Thus, multiple caries can be a symptom of general disorders in the body, vitamin deficiency, and mineral metabolism disorders. Identification of dental plaque allows us to judge the function of chewing and oral hygiene. Tartar deposits indicate a violation of mineral metabolism.
Examination of the oral mucosa is carried out in natural light. The condition of the oral mucosa is affected by many pathological processes of the oral cavity and internal organs. Based on certain elements of the lesion, the first symptoms of diseases of the gastrointestinal tract, blood diseases, and malignant diseases can be established. Healthy oral mucosa is pale pink. Congestion and cyanosis indicate a chronic inflammatory process; sharp hyperemia of the mucous membrane is observed in many infectious diseases - measles, scarlet fever, diphtheria, trauma, inflammation, and general diseases. Blue coloration of the lips, mucous membrane of the cheeks, and sublingual area indicates a lack of cardiac function. vascular system. Swelling of the oral mucosa is observed in diseases of the heart, kidneys, and in the presence of scars. Enlarged or atrophied papillae on the tongue indicate the possibility of pathological changes in the gastrointestinal tract. These are important diagnostic signs. During the examination, attention is paid to the presence of bleeding of the oral mucosa, which can occur with periodontal diseases, stomatitis, blood diseases, vitamin deficiencies, endocrine disorders, hemorrhagic diathesis, as well as with chronic trauma with a crown, dental plaque, filling, and so on. The examination data is entered into the dental patient’s medical record or special records. When filling out the documentation, anomalies, deformations, pathological changes, elements of the lesion and their location are carefully described. The normal state is not described. Filling out a dental formula is mandatory.
PALPATION
After the examination, palpation and palpation of the maxillofacial area (superficial, deep, extraoral and intraoral) are performed. This study determines: tissue consistency, turgor, mobility, relief, pain. Palpation is carried out with both hands, starting from the healthy side. Apply superficial and then deep palpation. Palpation of the lymph nodes is also carried out with both hands, giving the head the appropriate position. At the same time, their soreness, adhesion to soft tissues or bone tissue, and mobility are determined.
The teeth can be palpated with fingers or tweezers.
When palpating the tissues of the oral cavity, they fix the tissues and organs with one hand, and with the other they feel every part of the palate, tongue, cheeks, and sublingual area. Palpation determines the condition of the salivary glands and ducts.
PERCUSSION
Percussion is tapping on the tooth with the handle of a probe or tweezers. Percussion can be vertical or horizontal. Vertical percussion is painful if there is an inflammatory process in the area of the apex of the tooth. Horizontal percussion determines the condition of the marginal periodontium. Percussion is carried out carefully. Percussion begins with a healthy tooth, moving to the diseased one. Percussion can be weakly positive, positive and sharply positive. Movements should be light and uniform. During this examination, the patient himself determines which tooth hurts by comparing his sensations.
PROBING
This study is performed using a probe (usually angular), which is held in the right hand, and a dental mirror is held in the left hand. Probing determines the presence of a carious cavity, softening in it, the depth of the carious cavity, the pain of the bottom of the carious cavity, as well as the sensitivity of the enamel - hyperesthesia. Probing is performed very carefully.
ADDITIONAL INVESTIGATION METHODS
- Thermometric research methods
- Electrometric examination (electroodontodiagnosis)
- Histological and histochemical research methods
- Cytological examination
- Bacteriological research
- Blood and hematopoiesis research
- Urine examination
- X-ray examination
- Serological study
- Specific studies