- What is keratoplasty?
- Corneal pathology
- Causes of corneal diseases
- History of corneal transplantation
- How do you prepare for the operation?
- What types of keratoplasty are there?
- Postoperative period
Every day in our practice we see that every fourth patient comes to an appointment with a corneal disease. More than 10 million people worldwide suffer from corneal diseases. Pathology of the cornea is one of the main causes of decreased vision, blindness and low vision.
Indications
The list of indications includes pathologies that are not amenable to conservative therapy. Keratoplasty is indicated for patients with:
- corneal dystrophy (including those with minimal thickness);
- keratoconus (both in the early stages and in the late stages, including progressive ones);
- keratoglobus;
- Fuchs' dystrophy;
- the presence of scars on the surface of the cornea;
- damage to the cornea of various types;
- ulcers (wounds) of the cornea of any origin;
- eyesores of various natures, affecting visual acuity;
- bullous keratopathy associated with cataract surgery;
- congenital or acquired anomalies of the structure of the eye;
- defects of a traumatic nature.
Each indication for surgery for a particular patient is determined by the doctor.
Corneal pathology
The cornea is a unique optically transparent lens, the first to encounter an aggressive environment, conducts and refracts rays in a special way, and participates in maintaining the shape of the eyeball. Despite the high regenerative potential of corneal epithelial cells, it is an absolutely transparent structure, which is achieved by passive nutrition of this organ, which does not have its own vessels.
It is this amazing organ that is often susceptible to a huge range of diseases, risks and dangers associated with the loss of this unprecedented transparency: here is a wide variety of hereditary forms of corneal dystrophies, senile degenerations, injuries, burns, post-inflammatory changes, consequences of iatrogenic interventions, keratoconus, etc. The result of the listed diseases and their consequences is a violation of transparency, and, as a consequence, a persistent decrease in visual functions with absolutely healthy other optical environments and a well-functioning retina.
When keratoplasty is contraindicated
The list of contraindications includes:
- pregnancy;
- lactation period;
- inflammatory lesions of different parts of the eye (such as the cornea, sclera, conjunctiva) of an infectious nature: uveitis, keratitis, scleritis;
- ingrowth of blood vessels into the cornea (in normal conditions, the cornea of the eye and all its tissues are deprived of blood supply);
- chronic diseases in acute stages (complete remission should be expected);
- acute infections (you need to wait one to two weeks after the patient has completely recovered);
- autoimmune diseases.
Important! All contraindications and possible complications are identified during diagnosis.
Varieties
There are the following types of keratoplasty:
- End-to-end (penetrating) operation
. In this type, all layers of the patient's cornea are replaced, including the epithelium, stroma, and endothelium (the back layer of the epithelium adjacent to the chamber of the eye). Penetrating keratoplasty is indicated for pathological processes affecting cells of all tissues of the cornea. - Layered
. With the layer-by-layer technique, only individual sections of the cornea are transplanted. Not the entire tissue is transplanted, but a separate layer or two (unlike penetrating keratoplasty, in which the cornea is separated completely).
There are two types of lamellar keratoplasty:
- Front
. Layered anterior keratoplasty involves cutting and subsequent transplantation of the upper epithelium (the first layer), as well as in some cases the main layer - the stroma. The posterior lining epithelial membrane usually remains intact. - Posterior with excision of the posterior endothelium
. The method is more complex, but has fewer complications.
Depending on the purpose of the procedure, the following types of keratoplasty are distinguished:
- Therapeutic surgery is necessary to restore the structure and improve the condition of the cornea, often performed in conjunction with other interventions (for example, lens replacement).
- Refractive (optical), necessary to restore the functions of the patient’s cornea and to normalize refraction - the natural refraction of light rays passing through the cornea of the eye.
- Plastic transplantation allows you to restore the cornea locally or completely if there are defects on it, but while maintaining its function and structure.
- Cosmetic transplant. The operation is optional, but is performed to transplant a transparent cornea when the patient’s natural one is cloudy (this happens with complete blindness).
For your information! Separately, keratoprosthetics is distinguished. This is a transplant of a combined material made from donor tissue and rigid plastic material in the central part. Such operations are usually performed to strengthen the cornea as much as possible, for example, after previous unsuccessful keratoplasties.
Interventions are carried out in two ways: traditional surgical and more modern and laser. The first option requires high professionalism and experience of the doctor working with the instruments. The laser method is characterized by maximum precision, therefore it allows for manipulations of any complexity, cutting out areas according to the given individual parameters of the patient.
Features and benefits of keratolytics
A keratolytic is a softener for the skin of the feet based on chemical components. When applied to the skin, the product actively exfoliates keratinized particles of the epidermis, after which they can be easily removed with a nail file.
The main feature of the “liquid pedicure” is that the procedure does not require soaking your feet in water or using cutting tools. Keratolytics act effectively on dry skin, do not injure it and restore smoothness with minimal time.
Liquid pedicure helps to cope with problems such as:
- corns;
- dry calluses;
- cracks;
- rough keratinized skin;
- hyperkeratosis.
| Liquid pedicure is a safe procedure. The action of the active substances is aimed only at rough areas and does not affect healthy skin. When used correctly, keratolytics do not cause irritation or allergic reactions. But if you are individually intolerant to the components of the product and have skin damage, you should pay special attention to the procedure. |
Preparatory activities
Preparation for refractive layer-by-layer or through-and-through surgery includes examining the patient to assess the condition of his eyes and body. Indications and contraindications, the type of transplantation (end-to-end or layer-by-layer) are determined. For diagnostic purposes, the doctor prescribes specialized procedures: biomicroscopy to check all structures of the eye, pachymetry to measure thickness, scraping and biopsy of the membrane for subsequent microbiological and bacteriological studies. A blood test (general, for infections), examinations by a therapist and other specialists are also prescribed.
At the patient preparation stage, the affected areas of the cornea of the eye, their diameter, shape, volume and other parameters are also determined. This is necessary for the subsequent formation of a graft of the required size. If a patient is counting on donor tissue, he is put on a waiting list. The waiting period depends on the desired characteristics of the graft. When choosing artificial material, the wait is usually less long.
Your doctor will give you detailed recommendations for preparation. If the patient is taking blood thinners, they may be temporarily stopped or changed. You should not eat food on the day of surgery. Preliminary hospitalization in a hospital is not required.
Types of keratolytics
Heel softeners vary in the presence of active ingredients in the composition and can be:
- alkaline;
- acidic;
- with urea.
Let's take a closer look at each type.
Alkaline keratolytics
This is the most active softener that can easily cope with rough skin, old calluses, and corns on the feet. The alkali quickly dissolves the proteins and lipids that make up the epidermis, the surface of the skin becomes loose and dead particles can be easily removed with a pedicure file.
Alkaline keratolytics are quite active, so they should be used with caution and preference should be given to trusted manufacturers. Lotion for removing calluses and corns “Liquid Pedicure” from ARAVIA Professional is a product that quickly copes with foot problems, restoring the skin smoothness, softness and well-groomed appearance.
Acid keratolytics
Acid-based keratolytics
, as a rule, used for peeling.
- Fruit acid renews and moisturizes the skin.
- Salicylic acid has an antimicrobial effect.
- Dairy helps reduce the manifestations of hyperkeratosis.
But acids act only on the surface of the epidermis; they are not able to penetrate deeper layers and will not be able to cope with too rough skin.
Urea-based keratolytics
Products with urea
cause protein denaturation, that is, under the influence of the active substance, intercellular connections are broken and stretched. The stratum corneum of the epidermis softens greatly, but to remove it, you will have to make some effort by actively treating the skin with a file.
It is important to consider that when using a keratolytic with a high urea content (above 20%), the skin will quickly lose moisture and become very dry. Therefore, this product should only be applied to problem areas of the skin with severe roughness and it is better to entrust this to a professional.
Materials for transplantation
End-to-end or layer-by-layer surgery is carried out using either donor tissue or synthetic materials (artificial). The latter option began to be used relatively recently, only in the 21st century. It has a higher survival rate and minimal risk of rejection.
Tissue is collected from the donor either posthumously within 24 hours, or after brain death is determined while cardiac activity is preserved. Healthy patients without serious illnesses are eligible to receive a donor transplant. Tissues from infants and elderly people over 70 years of age are not used.
Progress of the operation
Refractive transplantation (both end-to-end and layer-by-layer) is more complex than other areas of ophthalmic surgery. The operation, which can be viewed on video, includes the following steps:
- The patient sits on a chair or lies down on a couch, fixes his head on a special holder;
- Anesthesia is administered. Local anesthetic drops are usually used, but at the patient’s request (or if there is a direct indication), the surgeon can perform the operation under general anesthesia;
- An eyelid expander is installed;
- The doctor begins the operation and begins performing manipulations. With refractive laser keratoplasty, the actions are performed with a laser beam. With the traditional surgical method, incisions are made with a thin scalpel or a special vacuum or manual trephine. Penetrating keratoplasty involves cutting through the cornea of the eye. With layer-by-layer plastic surgery, the cornea is cut into half or three-quarters, then exfoliated with a keratome;
- Then the excised area is removed, and donor or synthetic material is transplanted;
- Synthetic delicate cross-shaped continuous sutures are applied along the edges with a strong thread;
- Sometimes a special treatment lens is installed to protect the eye;
- A local antibiotic is instilled.
Duration ranges from 40-60 minutes to several hours (depending on complexity). The operation can be performed on an outpatient basis without hospitalization. In this case, after assessing the results and condition, if there are no problems (if everything went easily and without complications), the patient can go home. If the intervention was complex, the person operated on remains in the hospital for some time.
Rehabilitation
The rehabilitation period is quite difficult and long. The timing and speed of restoration of the patient’s visual functions depend on the initial pathology of the organ, the success of engraftment, the doctor’s experience, general health and other factors. Complete healing occurs within a year. The stitches are removed no earlier than six months later. In the first months, vision may deteriorate, which is gradually restored.
During rehabilitation, some restrictions apply:
- In the first 7-14 days, you should not get your eyes wet.
- Avoid any contamination.
- Mechanical influences must be excluded.
- UV protection when going outside.
- Reducing eye strain. You should read less, work on the computer, and use gadgets.
- Limit any activity in the first month, and heavy physical activity until complete healing (for a year).
- Regular visits to the doctor.
- Refusal to visit baths, swimming pools, saunas for a year.
- Refractive correction method with glasses.
The surgeon will give you more detailed and clear instructions.
Is there a possible complication?
Complications can occur, and their development is usually caused by medical errors, non-compliance with the recommendations given by the surgeon, as well as the individual characteristics of the human body.
One or more of the following complications may occur:
- rejection of the material, accompanied by pain, swelling, turbidity, discharge (occurs rarely - in 5-25% of cases, usually within the first month, less often - for six months);
- long-term healing and recovery;
- increased intraocular pressure (up to glaucoma);
- bacterial or fungal infections;
- cataract;
- keratoconus;
- failure, suture divergence;
- inflammation of different parts of the eye;
- iris prolapse, lens displacement.
If any complication occurs, you must immediately show the operated eye to the surgeon. So, in case of rejection, glucocorticosteroids should be applied topically every day, as prescribed by a doctor, several times. In case of infection, antibacterial drops are prescribed. Sometimes repeated intervention is required.
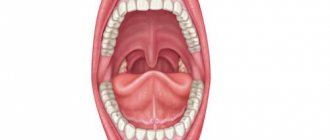
Medicines for the treatment of diseases of the mucous membrane of the mouth, tongue and lips
Diagnosis, treatment and prevention of diseases of the mucous membrane (OM) of the mouth, tongue and lips remain an important problem in clinical medicine. Changes in the CO of the mouth, tongue and lips in many systemic diseases occur long before the appearance of general clinical symptoms. Therefore, the correct interpretation of such changes and the choice of appropriate medications are of great importance not only for dentists, but also for other specialists.
When presenting the material, we used the classification of diseases of the oral cavity by E.V. Borovsky and A.L. Mashkilleyson [7], which provides for the identification of 9 groups of this pathology, taking into account etiological and pathogenetic factors, which, due to the impossibility of citing them, will be omitted in this publication. We limited ourselves only to issues of medical tactics, drug treatment of major diseases of the oral mucosa, tongue and lips.
The authors have made every effort to ensure the accuracy of the information presented, including drug dosages. Aware of our responsibility associated with the preparation of the publication, and taking into account the constant changes occurring in medical science, we recommend that the dosage of medications be updated according to the appropriate instructions.
Basic principles of treatment of diseases of the mucous membrane of the mouth, lips and tongue:
- Rational treatment requires contact between the dentist and other dental and non-dental specialists.
- Treatment must be carried out in compliance with the principles of bioethics, these diseases must be considered from the standpoint of the state of the whole organism, therefore in most cases one cannot limit oneself to local influences only.
- An axiom for the dentist should be the elimination of all unfavorable irritating factors in the oral cavity in the patient, which can support and provoke the development of the pathological process. It is unacceptable to use so-called cauterizing agents and long-term use of the same mouthwashes.
- Treatment should begin only after at least a preliminary diagnosis has been established and meet the following requirements: be comprehensive; provide a pathogenetic approach; do not disturb the anatomical and physiological characteristics of the oral mucosa; eliminate the pain factor; promote rapid epithelization of lesions; provide for the active involvement of the patient in performing medical procedures at home.
Traumatic lesions
Medical tactics for traumatic lesions of the mucous membrane due to the action of mechanical factors, high and low temperatures, radiation, unfavorable meteorological factors, and chemicals boils down, first of all, to eliminating the effect of the traumatic factor, which not only facilitates differential diagnosis, but is also a therapeutic intervention.
Decubital ulcer
Heals, as a rule, 10-12 days after eliminating the mechanical cause. The surface of the ulcer is treated with oxygen-containing antiseptics (hydrogen peroxide, potassium permanganate, sodium hypochlorite), and after cleaning its surface from necrotic plaque, keratoplasty agents are used. It should be remembered that with prolonged existence (more than 2-3 months), especially in older people, a decubital ulcer can become malignant.
Chemical injury CO
It occurs as a result of its immediate immediate contact with concentrated solutions of acids, alkalis, some medications and agents sometimes used by dentists (silver nitrate, arsenic paste, resorcinol-formalin mixture). In case of acute chemical injury, the CO drug that caused the burn is immediately neutralized (in the absence of a neutralizer, the mouth is washed with water). Subsequently, the affected areas are treated with anesthetic substances, weak antiseptic solutions, proteolytic enzymes, and then keratoplasty agents are applied.
Physical trauma CO
It can also be acute and chronic. Painkillers, antiseptics, and drugs that promote tissue regeneration are used. In some cases, it is necessary to resort to excision of the affected area.
Leukoplakia
A fairly common disease of the oral mucosa and red border of the lips, pathomorphologically characterized by chronic inflammation with pronounced hyperplasia and keratinization of the epithelium.
The scope of treatment measures is determined both by the form of the disease and the size of the lesion and the speed of development of the process. Among the medications for flat form of leukoplakia, applications are made to the lesion and vitamin A is prescribed orally (3.4% oil solution of retinol acetate or 5.5% retinol palmitate, 10 drops 2-3 times a day for 1. 5-2 months). Courses are repeated 2-3 times a year. For verrucous and erosive forms, the same is done within one month, and in the absence of positive dynamics, the lesion is excised, followed by mandatory histological examination, which determines further medical tactics.
The manifestations and severity of changes in the mucous membranes of the mouth, tongue and lips during infectious diseases depend both on the type of pathogen and on the individual characteristics of the patient’s body, which determines the dentist’s tactics.
Adenoviral diseases
In case of influenza and adenoviral diseases, the lesions of the mucosa are not specific; after a few days from the onset of the disease, hyperemia with “granular” rashes on the mucous membrane is replaced by petechial rashes, and by the 7-9th day the pathological changes disappear.
Chronic recurrent herpes
It appears at any age in persons previously infected with the herpes simplex virus.
Medical tactics for viral infections include the use of drugs from several groups that affect various parts of the etiology and pathogenesis of diseases: antivirals, immunocorrectors and immunomodulators, vaccines, interferons and their inducers. The most pronounced therapeutic effect is observed with the combined use of 2-3 drugs of general and local action with different mechanisms of antiviral effect.
Ointment and cream are started to be used when the first signs of infection activation appear and continue until the erosions are epithelialized. Early treatment can prevent the development of vesicles. A large group of antiviral drugs includes nucleoside analogues, similar in structure to intermediate products of DNA and RNA biosynthesis (iododeoxyuridine, chlordeoxyuridine, fluorodeoxyuridine), effective against generalized forms of herpes and herpes zoster. An effective antiviral agent is acyclovir (Zovirax, Virolex). In addition to acyclovir, the group of abnormal nucleosides includes: valacyclovir (Valtrex) in tablets of 500 mg; take 2 times a day for 5-7 days; famciclovir (famvir) tablets 250 mg; take 3 times a day for 7 days.
It should be noted that the therapeutic effect of antiviral drugs is most effective when prescribed in the first hours and days of development of the lesion elements and in the prodromal period of the viral disease.
Local antiviral drugs include: adimal, bonafton, florenal, riodoxol in the form of ointments and liniments (gossypol). Ointment and cream are started to be used when the first signs of infection activation appear and continue until the erosions are epithelialized. Moreover, early treatment can prevent the development of vesicles.
The leading role in the development of antiherpetic immunity belongs to interferon. The antiviral drug "Infagel" (it includes recombinant interferon alpha-2) has a wide spectrum of antiviral activity, bacteriostatic and anti-inflammatory effects, as well as antitumor and immunomodulatory activity. It is used in the form of applications to the lesions 2 times a day with an interval of 12 hours and dried for 10-15 minutes to form a protective film [10].
Interferon inducers (poludan, larifan) and antiviral vaccines (in the form of a cycle of intradermal injections to prevent relapses and during remission of the disease) have found widespread use in dental practice. The therapeutic effectiveness of the vaccine increases significantly when combined with poludanum or other interferon inducers.
In addition to these drugs, salicylates, analgesics, antihistamines and antiseptic solutions, multivitamins, EF radiation and helium-neon laser radiation are used in the treatment of herpes infection. To stimulate the processes of regeneration of the mucous membrane of the mouth and the red border of the lips, applications of oil solutions of vitamins A, E, ointment and jelly of solcoseryl and Actovegin, aerosols “Livian”, “Spedian”, “Gipozol” are used. After eliminating the elements of the lesion, sanitation of foci of chronic infection is mandatory.
In case of herpes zoster, along with the measures mentioned above, the doctor’s task includes eliminating the pain syndrome and preventing postherpetic neuralgia. For this purpose, analgesics, ganglerone, and B vitamins are prescribed.
Vincent's ulcerative-necrotizing gingivostomatitis (YANGS)
This is an inflammatory disease of the mouth, characterized by necrotic decay of the affected areas. Medical tactics for YANGS in some cases (especially in severe cases) include hospitalization of the patient, local and general measures, and medical examination.
Local treatment is important and begins with the patient’s first visit to the doctor, and then is carried out daily and in stages:
- Pain relief (applications, oral baths).
- Treating the mouth with antiseptic solutions (more effective - those that release atomic oxygen and chlorine-containing preparations: hydrogen peroxide, potassium permanganate, hypochlorite).
- Mechanical (and after application of proteolytic enzyme solutions to the lesion) removal of necrotic tissue, removal of mineralized dental deposits and elimination of other local traumatic factors.
- After cleansing the lesions from necrotic plaque, it is possible and advisable to use (in the form of applications) keratoplasty agents and preparations that promote tissue regeneration (oxycort aerosol, methyluracil ointment, oil solutions of vitamins A and E).
- It is better to postpone the removal of damaged teeth and roots, treatment of chronic forms of pulpitis and periodontitis until the ulcers are completely epithelialized.
- Subsequently, final sanitation of the oral cavity (planned treatment of caries, its complications, periodontal and mucosal diseases).
General treatment (especially for severe disease) involves the use of antimicrobial drugs. Orally prescribed: metronidazole (Flagyl, Klion) 0.25 g 2 times a day for 7-10 days, in some cases it is necessary to use broad-spectrum antibiotics. General strengthening and stimulating therapy is also carried out: ascorutin, vitamin C in large doses (up to 3.0 g per day), and antihistamines are prescribed. The nutrition of patients with YANGS should be complete and balanced.
Fungal infections of CO
Fungal infections of the mouth (oral mycoses) are most often caused by fungi of the genus Candida albicans.
General treatment includes:
- Ingestion of antifungal drugs for 10 days: diflucan (capsules) 50-100 mg 1 time per day; the use of polyene antifungal drugs (nystatin, levorin, amphotericin B) is traditionally included in general treatment, although it is known [11] that polyenes are practically not absorbed in the gastrointestinal tract, thus exerting a local effect on oral mucosa, and therefore It is recommended to dissolve the tablets in the mouth after meals (nystatin 1 tablet 500,000 units every 6-8 hours, levorin 1 tablet 500,000 units every 8-12 hours); Amphotericin B preparations are used mainly for severe systemic mycoses due to their high toxicity [11].
- Vitamins C, PP, group B taken inside.
- Use of antihistamines.
- Treatment together with other specialists of concomitant and background diseases.
Local treatment includes:
- Antifungal drugs for application and lubrication of lesions: 0.5% decamine ointment, 1% ointment and clotrimazole solution (canesten); 1% pimafucin ointment; for yeast infections and cheilitis, it is advisable to use 5% levorin ointment.
- Aqueous solutions of aniline dyes: 1-2% solution of gentian violet, 2% solution of methylene blue.
- Agents that alkalize the oral cavity: rinse with a 2% sodium bicarbonate solution; applications and lubrication of lesions with a 20% solution of borax in glycerin.
- A decoction of wild rosemary for mouth rinsing and oral baths.
Lesions of the oral mucosa are observed in all periods of syphilis, and dentists with similar manifestations have become much more common. Treatment of patients with syphilis is carried out in specialized venereological institutions. Dental interventions are usually associated with the sanitation of the oral cavity and are carried out in strict compliance with the disinfection and sterilization regime in health care facilities.
Treatment of fixed and widespread allergic and toxic-allergic diseases includes the “exclusion” of the allergen, for example, a drug, the use of painkillers, antiseptics, desensitizing and keratoplasty agents, if necessary. Sanitation of odontogenic foci of chronic infection is mandatory.
Erythema multiforme exudative
A fairly common dermatosis affecting the oral mucosa, observed mainly in young and middle-aged people. Stevens-Johnson syndrome is a severe variant of exudative erythema multiforme (also called acute mucocutaneous-ocular syndrome).
Medical tactics depend on the severity of the disease. In some cases, patients need to be hospitalized.
General treatment is usually prescribed by other specialists (dermatologist, immunologist) and includes:
- Detoxification therapy: drinking plenty of fluids or infusion therapy if it is impossible to take liquids orally.
- Taking glucocorticoids: prednisolone in an initial dose of 20-60 mg per day orally for 5-7 days (the dose depends on the severity of the process and the form of the disease, with Stevens-Johnson syndrome higher dosages are required), then the dose of prednisolone is reduced by 5 mg every 2 —3 days before complete withdrawal of the drug.
- Immunomodulatory therapy: for example, Lavomax (Tilorone) is prescribed 125 mg (1 tablet) orally in the first two days, then 125 mg after 48 hours. The dose of the drug per course is 2.5 g [15].
- Prescription of antihistamines, B vitamins, ascorutin.
- Antibiotics are prescribed when there is a threat of purulent-inflammatory complications and the doctor is confident that there is no connection between the development of the disease and the use of these antibacterial agents.
Local treatment is aimed at relieving inflammation and accelerating epithelization of the affected areas of the mucous membrane of the mouth and lips. It includes:
- The use of painkillers (1-2% solutions of trimecaine, lidocaine, anesthetics in aerosols) before each manipulation in the oral cavity (baths, rinses, applications) and before meals.
- Antiseptic treatment of the mouth (solutions of hydrogen peroxide, potassium permanganate, chloramine).
- To improve the rejection of necrotic tissues, apply solutions of proteolytic enzymes (trypsin, chymotrypsin) to the lesions.
- After cleaning the eroded surfaces from purulent-fibrinous plaque, use keratoplasty preparations (sea buckthorn and rosehip oil, oil solutions of vitamins A and E, the drug “Gipozol”).
- EF irradiation of the oral mucosa.
After the elimination of acute phenomena, the foci of infection are sanitized. In the inter-relapse period - specific desensitizing therapy.
Chronic recurrent aphthous stomatitis
One of the most common diseases with an autoimmune component of pathogenesis, it is characterized by periods of remission and exacerbation with the formation of aphthae (a superficial painful defect of the mucous membrane of a round or oval shape, covered with fibrinous plaque and surrounded by a bright inflammatory rim).
General treatment is prescribed after consultation with an immunologist:
- Immunocorrective and immunomodulatory therapy with thymogen, levamisole.
- Metabolic drugs for 10 days (calcium pantothenate orally 0.1 g 4 times a day; potassium orotate 0.5 g 3 times a day an hour before meals, lipamide 0.025 g 3 times a day after meals).
- Sedatives and adaptogens.
- Exclusion from the diet of hot, spicy foods, prohibition of smoking and drinking alcohol.
- In the inter-relapse period - specific and nonspecific desensitizing therapy.
- Vitamins: C, group B.
Local treatment:
- If there are aphthae, apply painkillers to the aphthae.
- Injections under the base of the aphthae with a mixture of 0.1 ml of 0.1% atropine sulfate and 1 ml of 0.25-0.5% solution of novocaine or trimecaine.
- Applications to aphthae of biopolymer soluble films (for example, oblekol films).
- Applications to aphthae of oil solutions of vitamins A, E, Oblekol, “Aevita”.
Pemphigus
Among the pathological processes of the oral mucosa with the formation of blisters (vesical dermatoses), the central place is occupied by pemphigus - an autoimmune process in which intraepithelial blisters appear on the skin and mucous membranes.
Treatment is coordinated with a dermatologist and begins in the hospital. Glucocorticoid therapy (first in shock and then in minimal, maintenance doses) interrupts the progression of pemphigus and leads to the disappearance of clinical symptoms of the disease. It should be remembered that local use of glucocorticoid drugs is ineffective. Sometimes cytostatics (mainly methotrexate) are also used to treat pemphigus.
Local treatment is aimed at preventing secondary infection of erosions and ulcers. Non-irritating CO solutions of antiseptics and keratoplastics are used.
Lichen planus
Mucocutaneous reaction - lichen planus occurs in 1-2% of the population. When treating lichen planus, an integrated approach is required, the basis of which is psychotherapy, especially at the initial stage, supplemented by the prescription of tranquilizers, sedatives, adaptogens, desensitizing agents, vitamins (A, PP). An effect was detected when prescribing the anxiolytic “Tenoten” (from 1 to 4 tablets per day for 3-6 weeks) and the antioxidant “Kudesan” [9].
Smoking and taking allergenic products is prohibited. It is necessary to exclude dissimilar metals in orthopedic structures and replace metal fillings. With exudative-hyperemic and erosive-ulcerative forms, it is sometimes necessary to resort to steroids (prednisolone) and drugs such as delagil.
Local events include:
- Local anesthetics.
- Applications of 1% emulsion of dibunol, vitamins A, E, Solcoseryl ointment.
- Irradiation of lesions with a helium-neon laser in combination with oral administration of tigazone capsules (10 mg 3 times a day for a course of up to 6-8 weeks).
- Electrophoresis of vitamin PP from dimexide medium.
In his medical practice, the dentist must proceed from the fact that lichen planus can become malignant.
Changes in the mucosa of the mouth and the red border of the lips often occur in pathologies of various organs and systems of the body and metabolic disorders.
It should be noted that in most cases, the manifestation of systemic diseases in the oral cavity is not specific, however, some changes in the oral cavity clearly indicate one or another type of organ or systemic disorder and are of great clinical significance.
Vitamin A deficiency
Causes disturbances in the epithelial structures of the skin and oral mucosa. Retinol is prescribed (in the form of a concentrate or pill) up to 50,000-100,000 IU per day.
Vitamin B1 deficiency
Accompanied by hyperplasia of the fungiform papillae of the tongue, paresthesia and allergic reactions of the oral mucosa. For treatment, preparations of thiamine chloride and thiamine bromide are used in courses of up to 30 days. It is unacceptable to mix a solution of vitamin B1 with other B vitamins in one syringe or to administer them sequentially through one needle.
Vitamin B2 deficiency
It manifests itself as a peculiar change in the skin, red border of the lips, ulceration in the corners of the mouth (angular stomatitis), weeping, maceration of the epithelium. For medicinal purposes, riboflavin is prescribed orally at a dose of 0.01 g 3 times a day for 4-6 weeks.
Vitamin B6 deficiency
With a deficiency of vitamin B6, symptoms of disorders of the nervous system (polyneuritis) and gastrointestinal tract, angular stomatitis, cheilitis, and glossitis are observed. The daily therapeutic dose of pyridoxine for adults, administered primarily parenterally, is 0.05-0.1 g.
Vitamin B12 deficiency
Accompanied by neurological disorders, changes in hematopoiesis (B12-deficiency anemia). Hunter-Meller glossitis is characteristic. For therapeutic purposes, 1000 mcg of vitamin B12 is administered intramuscularly daily until hematological disorders are completely eliminated, during the same time (4-6 weeks) manifestations in the oral cavity are stopped. Subsequently, lifelong maintenance therapy is prescribed (one injection of vitamin B12 per month).
Vitamin PP deficiency
Severe PP (nicotinic acid) deficiency is described as “pellagra,” which is characterized by a triad of symptoms: dementia, dermatitis, diarrhea. Treatment consists of taking nicotinic acid orally after meals (0.1 g 2-3 times a day for a course of 2-3 weeks). At the same time, thiamine, riboflavin and pyridoxine are usually prescribed, since in most cases polyhypovitaminosis occurs.
Vitamin C deficiency
It manifests itself as hemorrhagic syndrome (petechial hemorrhages in various parts of the oral mucosa, swelling and bleeding of the gums) and complications caused by the addition of a secondary infection (ulcerative necrotizing gingivitis). For therapeutic purposes, ascorbic acid is prescribed up to 1.5 g per day (after meals) with simultaneous intake of rutin (50-100 mg 2-3 times a day).
Most diseases of the blood and hematopoietic organs have typical manifestations in the oral cavity: changes in the color of the mucous membrane, the phenomenon of hemorrhagic diathesis, paresthesia, ulcerative-necrotic processes. The mucous membrane of the mouth in acute leukemia is almost constantly affected. In more than half of the patients, changes in the mucosa are ulcerative-necrotic and hemorrhagic in nature.
The dentist’s task when treating such patients (usually in a hematology hospital) remains pain relief, proper professional antiseptic treatment of the oral cavity, careful removal of necrotic plaque (mechanically and with the help of proteolytic enzymes), and stimulation of epithelization of lesions.
Salivary dysfunction
Disorders of this kind are of great clinical significance, especially associated with a decrease in the secretion of the salivary glands, up to hyposialia or even xerostomia.
Medical tactics:
- Distinction between “subjective” (i.e., developing against the background of somatic pathology without the death of the glandular epithelium) and “objective”, in which, due to the death of salivary gland tissue, there is a decrease in the secretory activity of the salivary glands.
- Identification and elimination of organ disorders; correction of disorders of “general” and “local” immunity.
- Elimination of foci of chronic odontogenic infection.
- Rational prosthetics.
- Medications include vitamins A, E, C, group B, and antidepressants.
- To stimulate salivation - orally (2-4 drops 15 minutes before meals) 1% solution of pilocarpine; galvanization of the salivary glands.
The doctor’s tactics for neurogenic diseases of the tongue, lips and mucus (glossalgia, glossodynia, stomalgia, burning mouth syndrome) include:
- Sanitation of the mouth to eliminate irritating factors (galvanism phenomena, defects in fillings and prosthetics) and eliminate chronic odontogenic infection; treatment of fungal infections of the mouth and tongue.
- Treatment of somatic diseases.
- Normalization of the function of the central and autonomic nervous systems; for somatized depression - antidepressants (for example, amitriptyline according to the scheme starting with one-fourth tablet at night, increasing weekly by one-fourth tablet, leading to a whole tablet per day by the end of the month).
- B vitamins.
- Vasoactive drugs and vegetotropic drugs.
- Applications of local anesthetics.
- Galvanization of the upper cervical sympathetic nodes, in some cases - ultratonotherapy, ozone therapy, etc.
If conservative treatment of erosive and ulcerative lesions (for example, in chronic trauma, leukoplakia, lichen planus) within 10-14 days is ineffective and there is no tendency to their healing, surgical or cryosurgical excision of the lesion with mandatory histological examination should be used.
It must be remembered that all precancerous conditions must be treated surgically. There is no need for wait-and-see tactics and long-term drug therapy. This is permissible, as mentioned above, only in cases of damage to the mucosa of the mouth, tongue, and lips, where reverse development of the pathological process is possible under the influence of only therapeutic treatment.
This article is intended both for practicing dentists and for students, interns, residents, and young teachers of medical universities. However, it will be a shame if the reader only absorbs some of the information and concepts presented in it. To expand your own knowledge and for the benefit of our patients, it is advisable to read other publications on this issue [1-8, 12-14, 16-18].
LITERATURE
- 1. Banchenko G.V. Combined diseases of the oral mucosa and internal organs. - M.: Medicine, 1979. - 190 p.
- Banchenko G.V., Maksimovsky Yu.M., Grinin V.M. Language is the “mirror” of the body: Clinical guide for doctors. - M., 2000. - 408 p.
- Borovsky E. V., Danilevsky N. F. Atlas of diseases of the oral mucosa. — 2nd ed., revised. and additional - M.: Medicine, 1991. - 320 p.
- Danilevsky N. F., Leontyev V. K., Nesin A. F., Rakhniy Zh. I. Diseases of the oral mucosa. - M., 2001. - 271 p.
- Diagnosis, treatment and prevention of dental diseases / V. I. Yakovleva, E. K. Trofimova, T. P. Davidovich, G. P. Prosveryak. — 2nd ed., revised and supplemented. - Mn.: Higher. school, 1994. - 494 p.
- Dmitrieva L. A., Glybina N. A., Glybina T. A. et al. Experimental substantiation of the use of a new antioxidant drug in the treatment of erosive and ulcerative lesions // Periodontology. — 2012, No. 3 (64). - pp. 52-58.
- Diseases of the mucous membrane of the mouth and lips / Ed. prof. E. V. Borovsky, prof. A. L. Mashkilleyson. - M.: Medicine, 1984. - 400 p.
- Diseases of the oral mucosa: Textbook / Ed. L. M. Lukinykh. - N. Novgorod: Publishing House of NGMI, 1983. - 212 p.
- Karakov K. G., Vlasova T. N., Oganyan A. V., Pisarev G. Yu. Optimization of complex therapy of lichen planus of the oral mucosa // Dentist-practitioner. - 2012, No. 1. - P. 35-37.
- Karakov K. G., Vlasova T. N., Oganyan A. V., Polyakova O. V. The role of complex therapy in the treatment of herpetic infection of the dental system // Practitioner dentist. - 2012, No. 2. - P. 48-49.
- Practical guide to anti-infective chemotherapy / Ed. L. S. Strachunsky, Yu. B. Belousov, S. N. Kozlov. - M.: Borges, 2002. - 384 p.
- Rybakov A. I., Banchenko G. V. Diseases of the oral mucosa. - M.: Medicine, 1978. - 232 p.
- Therapeutic dentistry: textbook: 3 hours / ed. G. M. Barera. - M.: GEOTAR-Media, 2055. - Part 3. - 288 p.
- Tretyakovich A. G., Borisenko L. G., Pishchinsky I. A. Differential diagnosis and principles of treatment of diseases of the oral mucosa: educational method. allowance. — 2nd ed., revised. and additional - Mn.: BSMU, 2005. - 66 p.
- Udzhukhu V. Yu., Minatulaeva M. A., Kubylinsky A. A. Pathogenetic rationale and clinical effectiveness of the use of Lavomax in patients with exudative erythema multiforme // Farmateka. - 2008, No. 9. - P. 60-62.
- Tsepov L. M., Nikolaev A. I. Medical tactics for erosive and ulcerative lesions of the mucous membrane of the mouth, tongue and lips (Training manual). - Smolensk: SGMA, 2005. - 16 p.
A complete list of references is in the editorial office.
Where is keratoplasty performed?
The refractive correction method through keratoplasty is carried out in special ophthalmological centers located in Moscow and other Russian cities. And it is important to choose a clinic with an impeccable reputation, numerous positive reviews, and a license to carry out medical activities. The center must also be equipped with modern new equipment.
Pay attention to the choice of surgeon:
he must have a lot of experience, high qualifications and the necessary skills in keratoplasty techniques. Not all doctors perform such complex operations.
Our equipped modern clinic accepts patients with any eye diseases. We employ experienced and talented professionals. The center is equipped with all necessary equipment. You can make an appointment and receive advice, as well as qualified assistance.
Keratoplasty surgery allows you to restore the structure of the cornea of the eye or even restore vision. If you have corneal pathologies, contact the clinic: you may need a transplant.
Oral care for children
Children should follow the recommendations in this material. They should also adhere to the recommendations below.
- Use fluoride toothpaste. If your child is 2 years old or younger, consult your dentist or doctor before using fluoride toothpaste.
- If your child's teeth have not yet grown, use a terry cloth, wet wipe, or sponge to clean the gums after meals and before bed.
- If a child has a stable immune system, he should be taken to the dentist every 6 months for routine monitoring.
- Contact Child Life Services to learn how to help your child cope with pain. You can contact them at 833-675-5437 (833-MSK-KIDS).
to come back to the beginning