- A little about the paranasal sinuses
- What to do if pathological changes are detected in the images?
- Which is better: radiography or CT of the paranasal sinuses?
- Prices for x-ray of the nose
- The clinic is located a three-minute walk from the Ulitsa 1905 Goda metro station
X-ray of the paranasal sinuses is a diagnostic procedure that is often prescribed by ENT doctors. First of all, it is carried out in order to diagnose the inflammatory process in the paranasal sinuses - sinusitis. But other pathologies can also be identified, because the photographs show the adjacent bones of the skull and the dental system of the upper jaw. The advantages of radiography are that it is a fast, affordable and non-invasive diagnostic method. In the images, the doctor can immediately see pathological changes and prescribe further examination and treatment for the patient. The quality of diagnostics depends on how modern the model of the device is used in the clinic, and how clear the images it allows to obtain. At the ProfMedLab clinic you can undergo testing using good equipment and quickly receive an accurate diagnosis.
A little about the paranasal sinuses
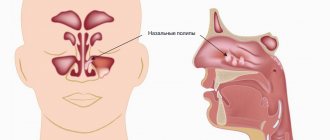
The paranasal sinuses, or sinuses, are located in the bones of the skull. They are lined with mucous membrane and communicate with the nasal cavity. These formations perform many useful functions: they reduce the mass of the skull bones, warm and moisturize the inhaled air, soften blows to the face, participate in the formation of the timbre of the voice, and help to sense changes in environmental pressure.
Humans have four types of paranasal sinuses:
- The most famous are the maxillary ones. As the name suggests, they are found in the upper jaw. These sinuses are also called maxillary sinuses, and inflammation in them is called sinusitis.
- The frontal sinuses are located in the frontal bone, just above the bridge of the nose. When inflammation develops in them, frontal sinusitis is diagnosed.
- Inside the skull, in the thickness of the ethmoid bone, there is a ethmoid labyrinth. Inflammation in its cells is ethmoiditis.
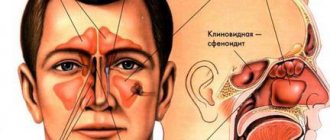
- The sphenoid sinus is the only unpaired sinus. It is located in the bone of the same name, which is located deep in the very center of the skull. Only its wings protrude outward. The inflammatory process in the sphenoid sinus is called “sphenoiditis”.
The general term for inflammation in any of the paranasal sinuses is “sinusitis.”
Briefly about sinusitis
Sinusitis is inflammation of the mucous membrane in the maxillary sinuses. Nathaniel Gaymore was the first to describe these sinuses: the name came from his name. And Leonardo da Vinci was the first to draw the maxillary sinuses.
Essentially, sinusitis is sinusitis caused by various reasons, which are associated with infection in the sinuses and the accumulation of pus in them. It can be rhinogenic, odontogenic, traumatic, allergic.
Rhinogenic occurs due to untreated rhinitis, when the infection penetrates from the nasal cavity into the sinuses. Odontogenic sinusitis develops as a result of infection through a diseased tooth and inflamed tissue around it.
Traumatic rhinitis is a consequence of damage to the nasal septum, maxillary sinus or jaw.
Finally, allergic rhinitis occurs due to allergies to pollen, animal dander, dust mites, medications and other allergens.
Acute sinusitis lasts less than 3 months, recurrent acute sinusitis occurs up to 4 times a year, chronic sinusitis lasts from 3 months or more. An exacerbation of chronic sinusitis is also possible, when new symptoms are added to existing ones.
In what cases is radiography of the paranasal sinuses necessary?
Most often, the reason for prescribing radiography of the paranasal sinuses is a suspicion of sinusitis. Symptoms of this disease: constant nasal congestion, pain in the forehead, upper jaw, swelling in the affected sinuses, discharge of yellow or green mucus from the nose, increased body temperature. Sinusitis can manifest itself in the form of toothache and bad breath.
Also, radiography of the paranasal sinuses is prescribed for injuries to the nasal area, suspected hemorrhage, benign and malignant tumors, and other pathological formations. In dentistry, this study is usually carried out before surgical interventions on the upper jaw. In addition, radiography of the paranasal sinuses helps clarify the diagnosis for the following symptoms and conditions:
- Chronic headache. If it is persistent and cannot be treated, the neurologist may refer the patient for a consultation with an ENT doctor.
- Chronic cough.
- Secretory otitis media. With this disease, mucus accumulates in the tympanic cavity, the ventilation of the middle ear is disrupted and hearing deteriorates.
- Chronic pharyngitis is an inflammation of the pharyngeal mucosa.
- Dacryocystitis is an inflammatory process in the lacrimal sac of the eye.
- Hypertrophy (pathological enlargement) of the nasal turbinates.
- Deviation of the nasal septum.
After sinus surgery, radiography is used to monitor the results of treatment.
Lesions on MRI of the brain: what does it mean?
The result of magnetic resonance imaging is a series of layer-by-layer images of the area under study. In the images, healthy tissue appears as alternating light and dark areas, depending on the concentration of fluid in it and the pulse sequence used. Based on the sections, the radiologist evaluates:
- development and position of individual structures;
- compliance of the MR signal intensity with the norm;
- condition of the gyri and grooves;
- size and structure of the ventricular system and subarachnoid space;
- parameters of the ear canals, orbits, accessory sinuses;
- structure of the vascular bed;
- structure of cranial nerves and cerebral membranes;
- the presence of signs of pathology (focal changes, swelling, inflammation, damage to the walls of arteries and veins).
Lipoma of the quadrigeminal cistern on MRI (circled)
MRI is prescribed if the patient has neurological abnormalities due to damage to brain tissue. Symptoms may include:
- headache;
- impaired coordination of movements;
- dysfunction of the organs of hearing or vision;
- disturbances in concentration;
- memory disorders;
- sleep problems;
- psychoemotional disorders;
- paresis/paralysis of the limbs and/or facial muscles;
- sensory disorders;
- seizures, etc.
Magnetic resonance imaging of the head allows the doctor to accurately determine the location of focal changes and find out the nature of the patient’s poor health. At the Magnit DC, specialists are armed with the latest MR scanning devices, which allow them to conduct research with high reliability.
Study safety and contraindications
X-ray radiation is ionizing and can damage cells and genetic material. However, its doses, especially in modern digital devices, are very small and do not cause harm. If you have to undergo x-rays again and you are worried about the possible risks, you can keep a list of all the procedures and show the doctor when he prescribes the examination.
Any diagnostic methods using x-rays are contraindicated during pregnancy (especially in the first trimester) and breastfeeding.
Preparation for the procedure
Before starting the procedure, you must remove your outer clothing, metal and other jewelry, earrings, piercings, and remove dentures. Next, you need to tell the doctor whether similar procedures have been performed previously, whether there are dental implants, fractures of the nose or facial bone.
During the diagnosis, the patient must stand still and not move. He should rest his nose and chin on the stand of the X-ray machine, which has been previously adjusted to the patient’s height. After this, the doctor will take several pictures from another room and give further instructions to the patient. During the procedure, the patient will sometimes need to hold their breath for a few seconds (no more than 10 seconds). The radiologist will take pictures in two projections, and sometimes while lying down.
The whole procedure will take about 10 minutes.
Which is better: radiography or CT of the paranasal sinuses?
Computed tomography is more informative, and it is used when pathological changes cannot be identified and comprehensively studied using radiography. But this is not always necessary. In addition, CT scans are more expensive and involve higher radiation exposure to the body.
Modern digital X-ray machines allow you to obtain very clear, detailed images, which are often enough to establish an accurate diagnosis and prescribe the correct treatment. This is exactly the device that is used in the ProfMedLab clinic. In our clinic, based on the results of the study, you can get a consultation with one of the leading ENT doctors.
Types of lesions on MRI of the head
The color of the resulting image of normal brain structures and pathological changes depends on the program used. When scanning in angio mode, including using contrast, a branched network of arteries and veins appears on the images. Focal changes are of several types; based on their characteristics, the doctor can guess the nature of the foci.
With pathology of the medulla, the properties of the affected foci are disrupted, which is manifested by a sharp change in the MR signal compared to healthy areas. The use of certain sequences (diffusion-weighted, FLAIR, etc.) or contrast allows for more clear visualization of local changes. That is, if a radiologist sees a single lesion on the MRI results, different scanning modes or contrast will be used to study it in more detail.
When comparing changes with healthy areas of the brain, hyper-, hypo- and isointense zones are identified (bright, dark, and the same color as adjacent structures, respectively).
Brain abscess on MRI (indicated by arrow)
Hyperintense lesions
Identification of hyperintense, i.e. foci that clearly stand out on MR scans makes the specialist suspect a brain tumor, including of metastatic origin, hematoma (at a certain moment from the onset of hemorrhage), ischemia, edema, vascular pathologies (cavernomas, arteriovenous malformations, etc.), abscesses , metabolic disorders, etc.
Brain tumor on MRI (indicated by arrow)
Subcortical lesions
Damage to the white matter of the brain is usually characterized as changes in subcortical structures. Subcortical lesions identified by MRI indicate that the damage is localized just under the cortex. If multiple juxtacortical lesions are detected, it makes sense to suspect a demyelinating process (eg, multiple sclerosis). With this pathology, destructive changes occur in various areas of the white matter, including directly under the cerebral cortex. Periventricular and lacunar lesions are usually detected during ischemic processes.
Foci of gliosis
When brain tissue is damaged, compensatory mechanisms are activated. Destroyed cells are replaced by glial structures. The latter ensures the transmission of nerve impulses and is involved in metabolic processes. Due to the structures described, the brain recovers from injuries.
Identification of glial foci indicates previous destruction of the cerebral substance due to:
- birth trauma;
- hypoxic processes;
- hereditary pathologies;
- hypertension;
- epilepsy;
- encephalitis;
- intoxication of the body;
- sclerotic changes, etc.
By the number and size of altered areas, one can judge the extent of brain damage. Dynamic observation allows you to assess the rate of progression of the pathology. However, by studying the zones of gliosis, it is impossible to accurately determine the cause of the destruction of nerve cells.
Foci of demyelination
Some diseases of the nervous system are accompanied by damage to the glial membrane of the long processes of neurons. As a result of pathological changes, the conduction of impulses is disrupted. This condition is accompanied by neurological symptoms of varying degrees of intensity. Demyelination of nerve fibers can be caused by:
- multifocal leukoencephalopathy;
- multiple sclerosis;
- dissimulating encephalomyelitis;
- Marburg's disease, Devic's disease and many others.
Typically, demyelination lesions appear as multiple small areas of hyperintense MR signal located in one or more parts of the brain. Based on the degree of their prevalence, duration and simultaneity of occurrence, the doctor judges the scale of development of the disease.
Focus of demyelination on MRI
Focus of vascular origin
Cerebrovascular insufficiency causes ischemia of the cerebral substance, which leads to changes in the structure and loss of function of the latter. Early diagnosis of vascular pathologies can prevent stroke. Focal changes of discirculatory origin are found in most patients over 50 years of age. Subsequently, such zones can cause degenerative processes in the brain tissue.
Lacunar cerebral infarction on MRI (indicated by arrow)
Cerebral circulation disorders can be suspected by focal changes in the perivascular Virchow-Robin spaces. The latter are small cavities around the cerebral vessels, filled with fluid, through which tissue trophism and immunoregulatory processes occur (blood-brain barrier). The appearance of a hyperintense MR signal indicates expansion of the perivascular spaces, since they are normally not visible.
Sometimes an MRI of the brain reveals multiple lesions in the frontal lobe or in the deep parts of the hemispheres, which may indicate damage to the cerebral vessels. The situation is often clarified by MR scanning in angio mode.
Foci of ischemia on MRI
Foci of ischemia
Cerebral circulation disorders lead to oxygen starvation of tissues, which can provoke necrosis (infarction). Ischemic lesions on T2-weighted sequences appear as areas with moderately hyperintense signal of irregular shape. At a later stage, when performing MRI in T2 VI or FLAIR mode, a single lesion takes on the appearance of a light spot, which indicates a worsening of destructive processes.
Prices for x-ray of the nose
| Name of service | Price |
| X-ray of the nasopharynx | 1900 |
| X-ray of the lower jaw joints | 1700 |
| Printing an x-ray image on film | 500 |
| Consultation of radiographs, interpretation of studies performed in another health care facility | 700 |
| X-ray of the paranasal sinuses in the naso-mental projection with the mouth open (1 projection) | 1500 |
| X-ray of the nasal bones (2 projections) | 1700 |
| Interpretation of radiographs (from other health care facilities) | 1200 |
What does sinusitis look like in the picture?
Healthy paranasal sinuses in the picture are similar in shade to the eye sockets. If inflammation develops, they acquire a darker shade with whitish, “milky” contents. The usually smooth edges of the sinus may be curved, and thickening may be observed locally or along the entire edge of the sinus. This picture indicates that pathology has developed in the sinuses.
An otolaryngologist and a radiologist interpret the X-ray. Photos of the sinuses highlight potential abnormalities and darkened areas. The analysis can determine: the presence of potentially affected areas - darkened or sub-darkened areas, whether there is sinusitis - lightened areas of the sinuses.
After treating a runny nose and congestion, the doctor can also determine the nature of the disease - sluggish, stopped, chronic, acute, the presence of tumors or cysts.