Gum inflammation is one of the most common dental problems. The cause of inflammatory processes is often poor oral care and non-compliance with rules and regulations of hygiene, as well as injuries to the mucous membranes, accompanied by a violation of their integrity. It happens that inflammation begins after treatment at the dentist. If a patient’s gums become inflamed after going to the doctor, they should visit the dental office again, since this symptom almost always indicates the need for repeated medical intervention.
Slight soreness and swelling of the gums may be normal after complex dental treatment (for example, depulpation), but these signs should not be of high intensity or last more than 24 hours. Inflammation following extraction should also resolve within 48-72 hours after surgery. In all other cases, it is necessary to find out the cause of inflammation and take timely measures to prevent complications.
The gums became inflamed after dental treatment
Causes of edema
Swelling of the gums is a consequence of penetration of pathogenic bacteria into the soft tissues, causing infection.
Provoking factors:
- tartar formed due to poor oral hygiene;
- advanced form of caries;
- untreated stomatitis;
- infectious diseases of the throat;
- mechanical damage to soft tissues;
- difficult teething;
- immunodeficiency;
- vitamin deficiency (mostly severe lack of vitamin C);
- herpes virus activity;
- allergies to dental drugs or materials;
- development of purulent processes inside the tooth;
- the presence of tumors on the tooth root;
- gum diseases.
Before making a diagnosis, the dentist will definitely prescribe diagnostics to determine the internal state of the tissues, which will more clearly define the clinical picture and identify the main cause of the pathology.
What does a doctor do
If more than 3 days have passed after filling the canals, and the pain in the gums only increases, and other unpleasant symptoms appear, you should immediately consult a specialist. The doctor conducts a clinical examination, X-ray examination and, if necessary, decides on the issue of re-treatment of the tooth canals with his own hands.
The video in this article shows how to properly fill canals and restore a damaged tooth crown.
When performing secondary endodontics, all the same steps are performed as during previous visits. Treatment is supported by pharmacotherapy. The instructions must be followed exactly by the patient.
When re-treating canals against the background of mistakes made in a previous intervention, it is important to accurately obstruct the lumen.
Associated symptoms
Often gum swelling is accompanied by other symptoms:
- swelling of the cheek;
- fistula formation;
- tooth pain;
- bleeding gums;
- sensation of a metallic bite;
- redness of the gums;
- discharge of pus from the carious cavity;
- loosening of the crown;
- the appearance of ulcers;
- increase in general body temperature;
- the appearance of white plaque on the gums.
If there are signs of a purulent process, then contacting a dentist should be done immediately. Complications can lead to serious consequences not only for the oral cavity, but also for the entire body.
Swollen gums in an adult: other clinical cases
- Injury to the gums. Thermal and chemical burns lead to tissue damage around the element of the dental system. Symptoms can be expressed in increased bleeding, redness, and plaque.
- Poor quality canal sanitation. Poor canal filling can lead to periodontal abscess and result in swelling of the gums and cheeks.
- Extraction of a dental unit. After tooth extraction, in some cases the gums become swollen. This is especially observed after extraction of the figure eight. Swelling for 2-3 days is considered normal. However, if pain persists for more than three days, you should immediately consult a doctor.
The gums may swell not only after tooth extraction, but also due to an allergic reaction to pharmaceuticals and orthopedic structures. When any pathological process is detected, an immediate search for the problem and its elimination is required. If you do not receive qualified help, this can lead to loose teeth, abscess, otitis media and even the development of a tumor.
Possible dental diseases
In 90% of cases, swelling of the soft tissues around the tooth appears with the development of periodontitis, gingivitis, periodontitis or an abscess. Other possible causes are extremely rare.
Periodontitis
With the development of periodontitis, the inflammatory process affects the bone tissue of the jaw. The cause of the pathology is the penetration of infection of the dental root canals and its spread. Swelling of soft tissues during periodontitis is caused by the accumulation of pus. If left untreated, pus may be released through the resulting fistula. The swelling subsides during this period, but the inflammation cannot be eliminated on its own. Treatment is mandatory.
Gingivitis
A distinctive feature of gingivitis from periodontitis is the development of an infectious and inflammatory process in the soft tissues surrounding the tooth. Swelling of the gums with gingivitis mainly occurs during the period of exacerbation. The swelling of the gums can be so severe that the tissue covers the tooth.
Periodontitis
The development of periodontitis occurs against the background of advanced periodontitis. Lack of treatment provokes a purulent process with a localized abscess area. With a periodontal abscess, a cavity forms under the gum in which pus accumulates. Externally, in addition to edema, a pronounced swelling in the form of a semicircle up to 1–2 cm in size appears on the soft tissue. Treatment is carried out surgically.
Swelling of the gums due to periodontitis -
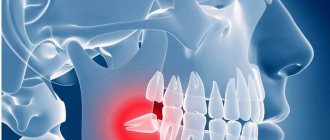
In case of poor-quality root canal treatment, due to tooth trauma, or in the absence of timely treatment of caries and pulpitis, inflammation occurs at the apex of the tooth root, which dentists call “periodontitis.” Sometimes the terms “granuloma” or “cyst” are used to refer to periodontitis, which you may well have heard. Such names are due to the fact that the focus of inflammation at the apex of the tooth root in these cases has the appearance of a purulent sac.
Symptoms - usually periodontitis has a chronic asymptomatic course, or there is only slight pain when biting on this tooth. But sometimes periods of exacerbation of inflammation occur, and in this case, acute pain may first occur in the causative tooth (especially when biting on it), and a little later, swelling of the gums usually appears in the projection of the causative tooth. But sometimes pain may be completely absent, and patients complain solely that the gums near the tooth are swollen (Fig. 1-3, 7-9).
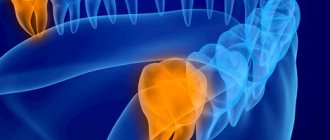
Please note that with periodontitis, the source of inflammation is located at the apex of the tooth root, i.e. quite deep in the bone tissue. Therefore, swelling of the gums during periodontitis usually develops not just in the projection of the causative tooth, but most often in the projection of the apex of the root of the causative tooth. And in multi-rooted chewing teeth - no less often in the projection of the bone interradicular septum. But periodontitis is not characterized by swelling of the interdental papilla or the gingival margin adjacent to the neck of the tooth.
In general, if you have swelling on the gum in one of your teeth, pain occurs when you bite on it, and there is a crown, filling or carious destruction on the tooth, and also if, in addition to swelling on your gums, you also have swelling of soft tissues face (again in the projection of the causative tooth) - you can definitely make a diagnosis of “Exacerbation of chronic periodontitis.” An X-ray of this tooth will allow you to accurately determine the cause of periodontitis and the required amount of treatment.
What treatment may be required -
As we said above, if the gums are swollen and painful, then in most cases the reasons are poor-quality filling of the canals, or the lack of timely treatment of dental caries and pulpitis. Only according to official statistics, root canal fillings are performed poorly by dentists in at least 60-70% of cases. The main errors during treatment are underfilling of root canals, poor obturation of root canals with filling substances, breakage of instruments, perforation of the tooth root...
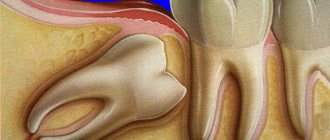
As a result of this treatment, a focus of purulent inflammation appears at the apex of the tooth root. Moreover, in the absence of timely treatment of the tooth for caries and pulpitis, exactly the same focus of inflammation will appear at the apex of the tooth root, but only against the background of unsealed root canals. In Fig. 10-12 you can see how the inflammation at the apex of the tooth root looks like during periodontitis (on the diagram, x-ray and on the root of the extracted tooth) -
Below we describe several treatment options that may be possible for patients with gum swelling due to dental periodontitis. In any case, the doctor will first be forced to take an x-ray. The image will allow us to determine whether this tooth can be saved at all, the size of the inflammatory focus at the apex of the root, and whether root canals have been filled in this tooth previously. The treatment tactics will depend on the latter, and below we will tell you how to cure a tooth and remove swelling from the gums so that it does not appear again.
1) If the channels are not sealed -
If root canal treatment has not previously been carried out on this tooth, then standard treatment of periodontitis is carried out with mechanical treatment of the root canals and treatment of the source of inflammation behind the root apex. On your first visit, they will open your tooth, expand the root canals to allow pus to drain out through them, and leave the tooth open for several days, prescribing antibiotics and anti-inflammatory therapy.
If necessary, your dentist may then refer you to an oral surgeon to make a small incision in the gum to allow additional drainage of pus. After about 3-5 days, the doctor makes an appointment for a second appointment and, if the inflammation subsides, completes the mechanical treatment of the root canals and seals them - either first with a temporary medicinal paste, or immediately with gutta-percha (the latter depends on the size of the source of inflammation at the apex of the tooth root). You can read more about the treatment of periodontitis at the link above.
How the gum incision is made - significant swelling of the gums, or if your gums and cheek are swollen at the same time - indicates the formation of a large purulent abscess, which will require not only opening the root canals of the causative tooth, but also making an incision in the gums to release the pus. The incision is made under local anesthesia, the wound is then washed with antiseptics and a drain is inserted into it (see video below).
2) If the channels are sealed poorly -
If an x-ray shows that canal treatment has already been carried out previously and the cause of inflammation was incomplete filling of the root canals to the apex of the tooth root, then there are 2 treatment options: either standard conservative therapeutic treatment, or an option associated with resection of the root apex.
- Conservative therapeutic treatment - on the first visit, the filling/artificial crown is removed from the tooth, poorly filled root canals are unsealed, washed with antiseptics, and antibiotics are prescribed.
If necessary, the patient is referred to a dental surgeon to make an incision along the gum. Thus, to the treatment we described in the previous section, only 1 point was added here (unsealing the root canals). Then everything is the same - after the inflammation subsides, temporary or permanent filling of the root canals is carried out. If the source of inflammation is small, the canals are usually filled immediately and permanently with gutta-percha, and a permanent filling is placed at the next visit. If the inflammation is large, the canals are sealed with temporary medicinal paste for 1-3 months, and a temporary filling is placed. And only after this time the canals are filled with gutta-percha + a permanent filling or crown is placed. - Resection of the root apex (Fig. 13) –
This surgical method is much simpler and much cheaper than conventional therapeutic treatment, and it allows you to avoid removing the crown from the causative tooth in order to unfill and reseal the root canals.
However, this method is only suitable for those teeth in which the root canal was poorly filled only at the very apex of the root (and throughout the rest of the length the canal should be filled normally). This simple surgical operation is carried out within 25-35 minutes and consists of cutting off the apex of the root with the unfilled part of the root canal using a drill. To do this, an incision is made along the gum and a flap of the mucous membrane is moved back to give access to the bone tissue in the projection of the apex of the tooth root. Next, a small hole is made in the bone with a drill, through which the apex of the root is cut off and removed from the wound along with the granuloma/cyst at the apex. The wound is sutured and antibiotics are prescribed. Pros: cheap, simple, no need to remove the crown and re-treat the tooth.→ How is root resection surgery performed?
Treatment methods
Depending on the cause of gum swelling and accompanying pathological processes, the doctor may prescribe conservative treatment, or resort to surgical manipulation or tooth extraction. The clinical picture is determined by the results of examination and radiography.
Conservative therapy
When visiting a dental clinic, a specialist eliminates the cause of gum swelling and then begins to eliminate inflammation, symptoms and associated pathological processes.
The patient may be prescribed drug therapy, including:
- antiviral;
- painkillers;
- antibiotics;
- antihistamines.
Local therapy that has an antiseptic effect is required. The dentist may recommend the use of special ointments or gels, rinsing the mouth with medications or herbal decoctions.
Surgery
The help of surgical dentistry is necessary for certain indications. The need for surgical intervention arises with the development of a purulent process. The specialist will need to open the gum, fistula or root canal to release the pathological fluid. Next, the affected cavity is cleaned, treated with an antiseptic, and treatment of the underlying disease begins. Swelling of the gums can be a sign of a serious pathology that requires tooth extraction. The need for extraction or the possibility of saving the tooth is assessed by the doctor.
First aid for inflammation
It is better to use any medications to combat pathological symptoms after consulting a doctor, since all medications in this group have different compositions and a list of contraindications. At home, you can use various rinses as first aid before going to the dental clinic. They are not recommended for use for more than two days, since the absence of qualified assistance for a long period of time can worsen the patient’s condition and lead to the progression of the pathology.
Calendula decoction with salt
Calendula flowers have a disinfectant, antimicrobial and healing effect
Calendula is one of the most famous medicinal plants. Calendula flowers (marigolds) have a disinfectant, antimicrobial and healing effect, so a decoction of this plant helps to quickly cope with inflammation and speed up the healing of soft tissues. If you add salt to the decoction, you can improve the condition of the gums during purulent inflammation, since any salt perfectly draws out pus and ensures the outflow of exudate.
To prepare a medicine to treat inflammation, you must:
- Pour 100 g of calendula flowers into 700 ml of boiling water and put on low heat;
- cook for 15-20 minutes;
- add a tablespoon of salt and cook for another 5 minutes;
- leave for an hour and strain.
You should rinse your mouth with this decoction 3 to 10 times a day (depending on the degree of inflammation). Symptoms usually become less noticeable on the second day of use.
Bread crumb infusion
Bread crumb infusion is a simple and effective remedy for treating gum inflammation.
If you don’t have medicinal plants at hand, you can use a very simple but effective recipe and prepare an infusion from bread pulp. You can use any type of bread made from rye or peeled flour, as they contain a large amount of minerals and vitamins that have a positive effect on the condition and health of the gums.
Preparing the infusion is very simple:
- break one piece of bread (approximately 50-70 g) into small pieces and place in a shallow container;
- pour 300 ml of boiling water and add half a spoon of salt;
- leave for 5-7 minutes and cool.
You should rinse your mouth with this infusion 3-5 times a day. The product perfectly helps with any inflammatory processes, pain after treatment and tooth extraction, as well as at the initial stage of purulent-infectious processes.
Video - How to treat gum disease
- How to deal with unpleasant odors in the home of a seriously ill person
Tooth hurts after nerve removal and filling
Only a dentist after an examination will help you figure out why a tooth hurts after removing a nerve and filling its canals. Treating teeth on your own without a diagnosis is highly discouraged.
In dental practice, the procedure for treating tooth canals by removing a nerve is a rather complex manipulation. Cases of medical error are common. They are fraught with various complications, in which the filled tooth continues to hurt.
The main reason why a “dead tooth” (without a nerve) is bothersome is:
- removal of the filling material beyond the apex of the tooth - this occurs due to incorrect definition
- working tooth length;
- the doctor filled the canal incorrectly;
- a tool broke off in the canal;
- root perforation of the tooth;
- If your tooth aches, you may be allergic to the filling material.
It is worth considering that a tooth under a filling can hurt even without a nerve. After all, during the extraction procedure, only a small part of it is removed from the root canal, which branches off from the main nerve trunk. In addition, when removing and filling canals, dental tissues are damaged. When an anesthetic is applied to a tooth, pain is not felt; it begins to be felt after the anesthesia wears off. Such painful sensations are called post-filling.
After removal of a nerve, neighboring teeth can often be bothered, but it seems as if it is the treated tooth that is hurting. An experienced doctor will examine the dentition to identify and eliminate this problem. However, it is worth sounding the alarm when the nerve has been removed for a long time, and the tooth continues to hurt - this symptom may signal the development of chronic pulpitis or periodontitis.
The gums are swollen and very painful: the main reasons
If, with mild manifestations of pathological processes in the oral cavity, you do not seek medical help, this leads to serious complications:
- Periodontitis is an inflammatory-destructive disease in which all the symptoms of gingivitis are observed, but the damage extends much deeper than the mucous layer - it extends to the jaw bone. Symptomatically, this is expressed in changes in color, texture, and shape of the gingival margin. Soreness, bleeding, fever, and deterioration in general health appear.
- Periodontitis is a variety of lesions of the periodontium, that is, the space between the tooth socket and the root. Granulating can lead to the formation of a fistula with purulent discharge, and granulomatous can lead to the formation of a granuloma or cyst.
- Periodontal abscess or flux, as the disease is commonly called, is accompanied by a local accumulation of inflammatory exudate in the soft tissues. The focus may be located under the gum or periosteum, but swelling occurs not only in the immediate epicenter, but also around it. Collateral edema often deforms the shape of the face, disrupts its symmetry, and interferes with eating and opening the mouth.
Acute processes always have more rapidly developing and vivid manifestations, and during exacerbation of chronic ones they are less disturbing. But this is not a reason to wait for the disease to become chronic, because in this case not only bones continue to deteriorate, but also general sensitization of the body develops, immunity deteriorates, and the changes become irreversible.
Self-medication is often complicated not only by chronic illness, but also by loss of teeth, severe intoxication, and damage to internal organs.
Pain after complex surgery
One of the most common reasons that the gums hurt where the tooth has long been extracted is incorrect or incomplete extraction. Dental defects leading to this:
- crooked roots: it may not be completely removed, part of it remains and eventually begins to rot;
- fragile tooth: if a tooth falls into pieces when touched with a surgical instrument, one of them may remain in the gum and lead to inflammation;
- the tooth has no outer part left: this situation requires complex surgical intervention; simple extraction is not enough;
- The tooth is embedded deep in the gum tissue.
In all these cases, you can get rid of the pain only by extracting the remains of the tooth from the gums. To do this, usually an incision is made in the tissue, and the gums at the site of inflammation are peeled off from the jaw bone. After this, the remaining teeth are cut out using a drill or divided into parts and removed.
How to get rid of pain at home
If you suddenly begin to experience pain in a place where a tooth is no longer present, it is not recommended to apply warm compresses, wrap the area of inflammation with a warm cloth, or take warm decoctions. Due to heating, suppuration most often occurs, which causes unpleasant consequences.
Cooling the inflamed area helps relieve pain. In this case, you can use ice compresses or just a cool cloth.
A cold compress will help relieve pain and swelling
Folk recipes help relieve inflammation of the flesh at the site of an extracted or dead tooth: a decoction of chamomile, oak bark. You should not intensively rinse the sore spot, as there is a chance to wash out the newly formed blood clot. It's better to just keep the decoction in your mouth for a while.
No folk remedies will help with advanced inflammatory process. Self-medication makes sense only in the initial stages of the disease.
Pain due to hematoma
If the gums hurt for a long time after removal, the body temperature rises, the gums swell and suppuration begins in the place where the dead tooth was, then this indicates a hematoma. A characteristic sign is the bluish color of the gums in the place where the tooth was.
Why a hematoma occurs: an incorrectly performed operation, during which the doctor damaged a blood vessel, general ailments of the body. For example, a hematoma often appears in people with diabetes or hypertension. A weakened immune system increases the risk of hematoma.
The only way to get rid of toothache due to a hematoma is surgery. During this process, an incision is made in the gum flesh and the accumulated pus is released. After this, the wound is washed and a course of drug treatment is prescribed, which includes rinsing with dental antiseptics and taking antibiotics.
How babies teeth cut: timing and development factors
The foundation of baby and permanent teeth is laid during pregnancy: their health is directly affected by the lifestyle and health of the mother.
After the birth of a child, minerals accumulate in his body, which will become building materials for teeth. The first of them appears when the baby is six months old - this happens in most situations.
But there are many cases where a child was born with a pair of ready-made teeth, or vice versa, when teeth appeared after the first year of life. This is normal: the process is influenced by many factors - from food to place of residence, when exactly teeth are cut.
In total, nature plans 20 milk teeth. They appear in pairs, so teething in infants is usually divided into 10 stages:
- First (medial) lower incisors - 6-10 months.
- First (medial) upper incisors - 8-12 months.
- Second (lateral) upper incisors - 9-13 months.
- Second (lateral) lower incisors - 10-16 months.
- First upper molars - 13-19 months.
- First lower molars - 14-18 months.
- Upper canines - 16-22 months.
- Lower canines - 17-23 months.
- Second lower molars - 23-31 months.
- Second upper molars - 23-31 months.
From 3 to 6 years old, a temporary bite forms in the child’s mouth: it changes when the baby teeth begin to fall out. A temporary bite has a huge impact on a permanent one, and a person’s smile, which will be with him all his life, depends on its correctness.
Along with 20 milk teeth, the roots of 16 permanent teeth appear. The rest grow up at a later age.
We emphasize once again that deviations from the schedule are normal, even within a few months. To be sure, consult your pediatric dentist.