Reasons for education
The causes of this disease include previous injuries and inflammatory diseases of various etiologies. There are frequent cases of mucocele due to obstruction of the salivary gland of the oral cavity by stones. In an infant, mucocele symptoms can occur due to a number of different pathologies, such as atresia of the salivary gland ducts.
Experts do not have a consensus regarding the reasons for the development of ranulas - for example, many dentists believe that the frequency of formation of this pathology of the salivary gland is caused by the peculiarities of its structure. Others believe that the likelihood of this pathology occurring is determined genetically or at the stage of embryo development.
One of the significant reasons for the appearance of mucocele of the salivary gland is the habit of constantly biting the lower lip or injuring it in any other way. These constant mechanical microtraumas lead to the creation of a focus of infection and infection. Much less often, a tumor appears, for example, on the inner surface of the cheeks, on the upper lip or on the tongue.
How dangerous is the disease?
If the mucocele is not removed, inflammatory and mechanical complications occur
Inflammatory complications
As a result of infection of the mucocele, pyocele develops with serious consequences:
- Inflammation spreads to adjacent tissues and sinuses, leading to the accumulation of pus
- In some situations, when a mucocele suppurates, an external fistula occurs
- High risk of purulent meningitis, meningoencephalitis
- In a severe situation, a brain abscess develops
Mechanical complications
Associated with the pressure of the mucocele on anatomically important structures, resulting in:
- Destruction of surrounding bone tissue
- Dystrophic changes in the sinuses
- Impaired blood supply to blood vessels
- Displacement of the eyeball or tear glands
- Visual impairment
- Neuralgia
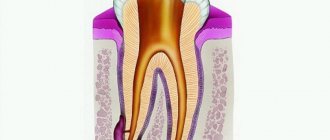
Classification of salivary gland mucocele
Based on the location of formation and the course of the pathological process, dentists distinguish cysts of the minor and major salivary glands. If a mucocele is located on the lower lip, due to its origin it is divided into true and extravasal. A true, or, as they are also called, retention cyst does not have its own membrane, but is always covered with a gland capsule on top. The capsule is formed due to the fact that the duct of the salivary gland is clogged, and mucus stagnates.
Extravasal or post-traumatic neoplasm on the lower lip occurs due to a violation of the integrity of the external capsule, which was accompanied by the release of secretions into the external tissues. Absolutely all neoplasms-cysts of the salivary gland, regardless of the nature of their origin, are divided into two main categories:
- A true formation, the shell of which has an epithelial lining. The most popular location for retention cysts is the parotid-masticatory and submandibular areas.
- A pseudocyst lacking an epithelial base. This subtype also includes mucoceles of the salivary glands. They are most often diagnosed on the mucous membrane of the lower lip and in the sublingual area.
Discussion
Typically, a mucocele is asymptomatic until it penetrates into adjacent structures. The clinical picture depends on the size of the mucocele, its location and the presence of complications. Initially, the formation occupies the cavity of the sinus or pneumatized cell, expanding it, then erosion of the bone walls and compression of nearby structures can be observed. Thus, regardless of the cause of the disease, mucocele has an osteolytic effect with bone resorption [18]. In the presented clinical case, the patient had a history of nasal trauma, and the conclusion of the cytological study noted the presence of siderophages in the contents of the formation. A possible mechanism for the formation of this pathology could be post-traumatic bleeding into the pneumatized perpendicular plate of the ethmoid bone with the formation of a hematoma and mucocele.
The most common symptoms in these cases are a feeling of pressure or pain in the facial area, hypoesthesia associated with compression of the branches of the trigeminal nerve, and nasal congestion. A fairly common complication of mucocele is infection with the formation of pyocele, which leads to chronic pain syndrome [19].
Despite the large size of the formation, in the presented clinical case the patient had no associated complications caused by compression of nearby structures. The main complaint that forced him to see a doctor was progressive difficulty in nasal breathing.
Before determining the extent and tactics of surgical treatment, mucocele of the nasal septum should be differentiated from some midline formations of the nasal cavity of mid-localization, such as encephalocele, meningocele, dermoid cyst, hematoma or abscess, benign neoplasms and tumor-like diseases of the nasal cavity [20].
Clinically, a mucocele differs from a cerebral hernia in the absence of tension, pulsation and changes in volume during breathing. Pressure on the encephalocele or meningocele is accompanied by symptoms of brain compression (slow pulse, convulsions). A dermoid cyst is distinguished by the presence of a thick wall and contents, including a fat-like or jelly-like mass with epidermal scales, hair, cholesterol crystals, bone inclusions, and teeth.
Studies such as CT, MRI, histological verification of the wall of the formation and cytological assessment of its contents can help in making a diagnosis. The classic MRI picture of a mucocele in T1 mode is presented as a hypointense lesion, in T2 mode - as hyperintense, although these views may vary depending on the water and protein content in the secretion (hyperintense signal in T1 with a high protein content) [16]. When performing a CT scan, typical signs of a mucocele are smooth, clear edges, and possible erosion of nearby bone walls [20].
The most effective way to treat this pathology is to create a large connection between the nasal cavity. In the presented clinical case, due to the large size of the mucocele, it was necessary to resect part of the perpendicular plate of the ethmoid bone that forms its capsule, with a immediate attempt to close the resulting defect in the nasal septum.
Diagnostics
The process of diagnosing this pathology includes a physical examination that reveals the presence of facial asymmetry, as well as a soft and elastic neoplasm that is painless on palpation.
Puncture of the salivary gland allows you to take a sample of its contents – a viscous yellowish liquid – for examination. Biochemical testing reveals an increase in salivary protein and amylase.
Ultrasound examination of the salivary gland is also used for diagnosis. It reveals the presence of a rounded neoplasm with smooth, clearly defined boundaries. To exclude the possibility of a false diagnosis (this is possible, since it is quite difficult to distinguish a true cyst from a pseudocyst), additional histological examination is recommended.
Recovery after surgery
No hospitalization
Since general anesthesia is not used in our Center, recovery is quick, post-narcotic complications and other troubles are excluded. There is no need to stay in hospital for 2-3 days 24/7. Modern equipment and safe sedation devices make it possible to organize a low-traumatic operation. You can return home 30-40 minutes after finishing.
For patients with cardiovascular and cardiovascular diseases, the Center has a postoperative ward. It is possible to recover within 2-3 hours under the supervision of our anesthesiologist-resuscitator.
Branded rehabilitation on the day of treatment
Our Center has developed an original method of accelerated rehabilitation for those who want to recover faster after surgery. The set of procedures is carried out on the day of surgery and, if necessary, repeated in bites. Aimed at minimizing hematomas, preventing swelling and pain:
Medicines to take home
Healing occurs within a week. You will receive a free complete package of necessary medications and instructions with rules of conduct during the rehabilitation period. We ask you to take your medications and follow the recommendations during the rehabilitation period to avoid complications.
The package contains the necessary medications and instructions with recommendations in the postoperative period
Treatment
The main treatment method for mucocele is surgery. The operation is performed by making two converging incisions to help isolate the cyst and quickly remove it. After the operation is completed, stitches and a special pressure bandage are applied.
However, this method is good when localizing a tumor on the lower lip. If it is located in the sublingual region, the operation may be somewhat more complicated and include “husking” or cystectomy of the salivary gland, or removal of the tumor directly along with the salivary gland.
Since the tumor is covered with a thin membrane, it is not always possible to perform surgery to remove it. Only complete removal of the tumor along with the salivary gland can be considered a fairly reliable remedy.
Stages of treatment
In our Center, all procedures are performed in one day, no hospital stay is required. During one visit we will carry out preparatory measures and the operation itself.
- Preparation Before any operation, hygienic brushing of teeth is required to maintain sterile conditions in the oral cavity and prevent the risk of infection of the operated area.
- Removal Performed in a sterile operating room of the ENT department. Lasts about an hour in a dream. Maxillofacial operates according to the selected protocol under the visual control of a microscope.
- Control A control computed tomography is performed to assess the quality of the operation performed - to ensure that the formation is completely removed and to assess the general condition of the maxillary sinus.
After the gums have healed and the sutures have been removed (after 10-14 days), the patient is invited for a follow-up examination. Next, preventive examinations are scheduled after 3 months, six months, a year to monitor the situation.
Symptoms
A mucous cyst (mucocele) is a thin sac filled with clear fluid. These formations are smooth in appearance and have a bluish-pink color. The size of the cyst can vary, but usually the width of the sac is about 5-8 millimeters.
A mucous cyst is usually not accompanied by any symptoms. There is no pain syndrome with mucocele.
Large mucoceles may interfere with chewing or speaking. There is also a chance that the cyst will burst, causing fluid to leak out of its cavity. In such a situation, infection cannot be ruled out.
Giant mucocele of the appendix
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
Mucocele is a cyst of the appendix containing mucus of varying consistency - from a jelly-like mass to a watery liquid, which in this case is regarded as hydrocele of the appendix, is a kind of rare neoplasm of the appendix and, according to various authors, occurs in 0.02-0.5% all appendectomies [3, 6, 9]. The pathogenesis of mucocele development is still unclear. Most authors believe that the cause of the formation of a mucoid cyst is chronic inflammation of the appendix with cicatricial narrowing of the base of the appendix, obliteration, compression or blockage of its lumen [4]. In this case, the outflow of mucus is disrupted while the secretory function of the epithelium of the mucous membrane of the appendix is preserved. Others believe that cysts and diverticula can be congenital or acquired, with the latter usually representing a hernia-like protrusion of the mucous membrane through the opening between the muscle fibers as a result of destruction of the wall of the appendix in acute appendicitis [8]. And finally, according to the nomenclature of tumors of the International Union Against Cancer (1965), mucocele develops from the remains of primitive mesenchyme and belongs to benign tumors, sometimes prone to malignancy.
There are complete cysts, which occupy the entire lumen of the process, with the exception of the base, where the lumen is obliterated, and incomplete ones, in which the cyst is located intramurally or occupies part of the lumen [3]. Cysts up to 3 cm in size are considered small, up to 6 cm - medium, and more than 9 cm - giant [3]. The following names for this pathological condition are found in the literature: appendix myxoma, mucous cyst, mucocele, myxoglobulosis.
Complications of mucoid cysts are inflammatory (peritonitis), mechanical in nature (volvulus or torsion of the process, intestinal obstruction), malignancy, breakthrough of mucous masses into the abdominal cavity with implantation and spread of mucus-forming cells throughout the peritoneum, massive contamination of the abdominal cavity and the formation of pseudomyxomatosis, which has a malignant course. Patients with pseudomyxomatosis die within 1-2 years [4, 7]. With the retrocecal location of the appendix with the development of a mucocele, the process may spread like pseudomyxomatosis into the retroperitoneal space with the formation of external fistulas [1]. Cases of fungal infection (cryptococcosis) of mucocele of the appendix have been described [10].
Clinically, mucocele usually occurs under the guise of chronic appendicitis or vague gastrointestinal discomfort, sometimes imitating ovarian cysts, abdominal or rectal tumors. The absence of pathognomonic clinical signs unique to appendiceal mucocele makes accurate preoperative recognition of this rare disease difficult [2, 3, 5, 6]. The diagnosis is established or clarified only during surgery. There are isolated reports in the literature on the preoperative diagnosis of appendiceal mucocele [11, 12].
We present our own observation of a giant myxoma of the appendix, mistaken for a neoplasm of the abdominal cavity. At the same time, we pay special attention to the image of appendix myxoma obtained using various radiological diagnostic methods, which we have not found in the available literature.
Patient K., born in 1936, was admitted to the abdominal department of the MRRC RAMS with a preliminary diagnosis of “abdominal neoplasm”. There are no complaints, the stomach is soft and symmetrical. Upon palpation, a volumetric formation with a diameter of up to 10 cm is determined in the right iliac region. X-ray of the chest organs reveals no focal changes. Excretory urography: the kidneys are without pathological formations, the ureters are located usually, not dilated, the bladder is of the correct shape, with clear contours. During irrigoscopy, no pathological changes in the large intestine were detected.
Computed tomography of the abdominal organs before and after intravenous administration of 40 ml of ultravist: in the right iliac region an irregularly shaped formation measuring 12.4 x 5.9 cm with smooth contours, density 33-35 units is determined, without change after the administration of a contrast agent (Fig. 1). The structure of the formation is heterogeneous, with the presence of point and stringy inclusions; a thin capsule can be traced, thickened and compacted in places, with the presence of calcification along the posterior wall. The upper pole of the formation is located in the ileocecal angle, in front it is adjacent to the anterior abdominal wall, medially - to the sigmoid colon, behind - to the m.iliacus and the right common iliac vessels, below - it descends in the form of a stalk into the small pelvis, tightly adjacent to the wall of the rectum and bladder. There were no signs of damage to these organs. The formation is mobile; when compared with the data of a previously performed CT study, a change in shape and position is noted. No enlarged lymph nodes were detected in the iliac region or retroperitoneum.
Rice. 1.
Mucocele of the appendix. Computer tomogram.
An ultrasound examination in the right iliac region reveals an L-shaped formation with clear contours, measuring 12.7 x 6.4 x 5.9 cm, mobile, at the beginning of the study the formation was located transversely, at the end of the study it moved upward and was located along the ascending section large intestine and the initial third of the transverse colon. The structure of the formation is heterogeneous due to the correct alternation of zones of increased and decreased echogenicity with a thickness of 2-6 mm. Symptoms of dorsal amplification of sound and lateral acoustic shadows are clearly visible (Fig. 2). No free fluid in the abdominal cavity or pathologically enlarged lymph nodes were detected. Liver, kidneys - without focal changes. Conclusion: cystic formation of the abdominal cavity.
Rice. 2.
Mucocele of the appendix. Echograms of the right iliac region in the longitudinal and transverse planes.
During surgery, a mobile formation measuring 14x8x6 cm, closely adjacent to the wall of the cecum, was revealed in the right iliac region. No pathological changes were detected in the liver and lymph nodes; a typical appendectomy was performed.
Macroscopic specimen: appendix 14 cm long with a racemose extension up to 8 cm over 11 cm and the presence of jelly-like contents. The wall thickness in different areas is from 0.3 to 0.6 cm (Fig. 3).
Rice. 3.
Mucocele of the appendix.
Macropreparation: a
— mucous contents of the cyst;
b
— cyst wall.
Histological examination: mucous cyst (mucocele). The cyst wall is represented by fibrous tissue, replacing all layers of the appendix wall, with focal lymphocytic infiltrates. The lumen is filled with mucus, colored pinkish by mucicarmine. Over a larger area, the lining is absent; only in a small area at the base of the cyst is a wall lined with cubic and columnar mucus-forming epithelium, as well as with the presence of mucus-forming cells among the mucus (Fig. 4).
Rice. 4.
A section of the wall of an appendix cyst at its base with a lining of cubic and columnar mucus-forming epithelium with mucus-forming cells in the lumen of the cyst among the mucus. Magnification x 280.
The postoperative course is smooth. A control ultrasound examination after 1 year revealed no pathological changes in the area of the appendix and cecum.
Literature
- Vladimirtseva A.L., Chattalos M.G., Poletaev V.A. Pseudomyxoma of a retrocecally located appendix with invasion into the retroperitoneal space and external fistulas // Pathology Archives. - 1989. - vol. 51. - N9. — P. 74-76.
- Dmitrievsky V.N. Appendiceal cyst simulating a retroperitoneal tumor // Bulletin of surgery. - 1981. - N2. - pp. 83-84.
- Imnaishvili B.E., Korkelia A.A., Dzhvebenava A.G. Giant mucocele of the appendix // Surgery. - 1973. - N1. — pp. 133-138.
- Korenev N.N., Kasherenkov V.F. Myxoma of the vermiform appendix // Surgery. - 1975. - N7. -WITH. 105-106.
- Kokhnyuk V.T. Mucocele of the appendix // Issues of oncology. - 1988. - N1. - pp. 87-88.
- Kuzmin V.I., Yashin N.P., Egorova T.M. Myxoma of the retrocecally located vermiform appendix // Surgery. - 1985. - N3. — pp. 117-118.
- Markov S.N. Mucocele of the appendix due to its torsion // Surgery. - 1980. - N7. — P. 92.
- Rusakov A.A. Guide to surgery. — M.: Medicine. - 1960. - vol. 7. - P. 465.
- Tazhimetov B.T., Ibragimov R.I., Utaev B.A. Strangulation of myxoma of the appendix in the umbilical hernia // Surgery. - 1989. - N2. — P. 124-125.
- Chekareva G.A., Gorbunova V.V. Cryptococcosis mucocele of the appendix // Pathology Archives. - 1976. - vol. 38. - N11. - pp. 71-73.
- Athey R.A., Nasken J.V., Estrada R. Sonographic appearance of mucocele of the appendix // J. Clin. Ultrasound. - 1984. - Vol. 12. - N6. — pp. 333-337.
- Horgan JG, Chow PP, Richter JO etc. CT and sonography in the recognition of mucocele of the appendix // Amer. J. Roentgenol. - 1984. - Vol. 143. - N5. - pp.959-962.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.