How chickenpox begins and develops Chickenpox is an acute infectious disease characterized by a profuse itchy rash on the skin and surface of the mucous membranes. It does not appear instantly: the incubation period can range from 10 days to 3 weeks.
Chickenpox is highly contagious. The virus is transmitted through direct contact with a carrier. Children often get sick in entire groups (groups in kindergarten or classes at school). We will tell you how to recognize the disease in the shortest possible time to prevent its spread.
What causes chickenpox?
The causative agent of this disease is human herpesvirus type 3. It belongs to the subfamily of alphaherpesviruses, which have the following features:
- a wide range of hosts (humans and animals);
- short reproductive cycle;
- rapid reproduction;
- volatility;
- rapid decay of affected cells;
- death under the influence of UV rays.
When the chickenpox virus enters the human body, for the first three to four days it is contained within blisters covering the skin. On the eighth day it ceases to be detected. Outside a living organism, type 3 herpesvirus dies in 15 minutes.
The rash usually appears 48 hours after infection. The carrier remains infectious for another five days. Infection occurs by airborne droplets. Contact-household infection is also possible.
How to recognize chickenpox?
To get sick, two conditions are enough: to be near someone with chickenpox and not have a history of it. Everyone gets infected with it, regardless of age and immunity strength. Nothing can be done during the incubation period. All we have to do is wait for the first signs:
- temperature rise to 38-39 degrees;
- general malaise;
- decreased appetite;
- the appearance of a characteristic rash.
At first, the rash is rare and looks like spots or pimples. Under no circumstances should you squeeze them out: the scar will be very deep. The volume of the rash gradually increases, covering all parts of the body.
In the early stages, chickenpox can be mistaken for an allergic reaction. But contact dermatitis rarely spreads throughout the body and never develops into blisters.
In this case, the person feels severe itching. Scratching chickenpox is also not advisable. This will not bring relief, but there is a risk of getting a lot of scars on the skin or causing a secondary infection.
Main symptoms of the disease:
- pain, itching, dryness;
- sensation of a lump or foreign body in the throat;
- swelling of the mucous membranes of the throat and pharynx;
- attacks of coughing and sneezing;
- nasal congestion (runny nose);
- discharge of mucous formations from the oropharynx;
- itching in the eyes (especially when combined with conjunctivitis), sore throat, nasal passages;
- the back wall of the larynx becomes red or even purple;
- weakening of the voice (hoarseness, hoarseness);
- feeling of “heat” in the throat area.
Fever is an uncharacteristic sign of the disease, which usually indicates the addition of a secondary infection.
The pathology is considered dangerous due to the possibility of pharyngitis turning into otitis media, sinusitis, and tonsillitis. Otolaryngologists at MedicCity, using the most advanced treatment methods and modern equipment, will be able to diagnose, treat you and relieve you of unpleasant symptoms. Don't develop allergic pharyngitis and don't let it ruin your life!
The acute form occurs with long-term or short-term exposure to allergens on the body. It usually goes away quickly. The long course of the disease and possible complications appear with prolonged contact with allergens. Inflammation can affect not only the throat, but also the respiratory tract, as well as the entire body.
Periods of chickenpox
Quite a long time passes between infection with the herpes virus and complete recovery. There are four periods:
- incubation (up to three weeks);
- prodromal (up to two days before the appearance of rashes);
- rashes (several waves for two to five days);
- crust formation.
During the prodromal period, the patient experiences general malaise. It is expressed in weakness, nausea, headache. Sometimes the temperature rises to 38-39 degrees, and vomiting occurs. In some patients, there is no prodromal period, and rashes immediately appear some time after infection.
Chickenpox in adults causes severe complications. They do not appear immediately. Some appear after the tenth day of the disease, others after a month.
Mononucleosis: myths and reality
Common myths about mononucleosis.
The article was prepared by Elena Kolganova, a pediatrician at the DocDeti clinic.
Mononucleosis is a viral disease caused by the Epstein-Barr virus (EBV).
Transmission of this virus occurs through close contact. For example, through saliva on shared utensils or during a kiss - this is what another name for this disease is associated with - “kissing disease”.
The symptoms are:
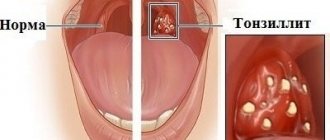
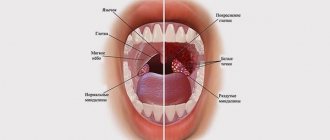
1. Tonsils affected by a white coating, as with a sore throat.
2. Enlarged liver and spleen
3. Enlarged lymph nodes in the neck, in some cases to such an extent that they can prevent the head from turning.
4. Adenoids - difficult nasal breathing, snoring.
As a result of a general blood test (CBC), special cells are identified - monocytes (a type of leukocyte) - mononuclear cells.
A number of nonspecific symptoms of intoxication in mononucleosis:
- High fever that lasts for a long time (2-3 weeks).
- Weakness.
- Lethargy.
- Decreased appetite.
- Drowsy state.
In most cases, the course of this disease is not accompanied by symptoms, and by the age of 5, in 50% of cases, children already have antibodies to EBV.
If we talk about the adult population, then in 90-95% of cases, the body has protective titers of antibodies against mononucleosis, because they suffered this infection at an early age.
As stated earlier, mononucleosis is a viral infection, so there is no specific treatment. It is necessary to eliminate the symptoms that interfere with life.
To combat the symptoms of infectious mononucleosis, your pediatrician may prescribe the antibiotic amoxicillin/ampicillin. In children who receive these drugs, in 85% of cases, a rash appears on the body, which is accompanied by spots and itching. This rash can linger for a long time (up to three months).
Even after complete recovery, EBV may appear in saliva for a couple of months. Throughout life, without any symptoms or clinical changes, EBV can be isolated from a person. This causes transmission of the virus.
If EBV is found in the saliva of a healthy person, then no therapeutic action is necessary!
Common myths:
1. If you have suffered from mononucleosis, then you can forget about a vacation at sea.
2. Previously, there was an opinion that EBV, under the influence of UV rays, takes on oncogenic activity and increases the possible risks of developing blood cancers - leukemia. But such a connection has not been confirmed in modern clinical studies. The possible involvement of EBV in the development of Burkett's lymphoma, nasopharyngeal carcinoma and certain types of gastric cancer has been noted. But these are independent diseases, and not a manifestation of mononucleosis. They can develop in people who have a predisposition to this and concomitant severe pathology: AIDS, malaria, primary immunodeficiencies. Burkett's lymphoma is common in Africa, and nasopharyngeal carcinoma is common in China.
3. Rupture of the spleen, as a result of its enlargement, is possible, but only in very extreme cases. For safety reasons, you should avoid blows to the abdominal area for three weeks from the moment of recovery.
4. Another common misconception is that you should avoid visiting children’s groups and vaccination is contraindicated within 6-12 months. These tips have not been confirmed in international studies, and therefore have no justification. Previous mononucleosis is not a contraindication to vaccinations, and you can be in children’s groups immediately after the child’s well-being improves.
5. A big misconception is chronic mononucleosis, which a child suffers from for several years and can only be cured with a complex regimen of immunomodulators. Infectious mononucleosis is an acute infection that lasts 3-4 weeks. After the illness, a condition similar to chronic fatigue (lethargy, pallor, drowsiness, lack of interest in games, apathy) may be observed for 3-4 months. There is no need to treat this condition, you just need to survive it.
How does chickenpox occur in children?
Chickenpox is considered a childhood disease, since it mainly affects children of preschool and primary school age. In children, the illness period is relatively short (about 10 days), while in adults it can last three weeks or more.
During this time, the rash goes through several stages:
- erythematous spots;
- nodular rash (papule);
- ulcers (pustules);
- crusts.
Recovery occurs when all the scabs fall off. Until this point, the person is still contagious and can pass the chickenpox virus to others. The first wave of rashes usually passes quickly, but it is replaced by several more.
As a rule, there are no complications in children. The main thing is that the baby does not scratch the rash to avoid secondary infection and scar formation. Severe disease occurs in newborns. When the first signs of chickenpox appear in an infant, you should immediately call a doctor.
Scarlet fever - symptoms and treatment
Early complications
In the case of a severe course with a toxic form, a terrible complication develops - toxic shock .
Purulent-septic complications may occur: peritonsillar (next to the palatine tonsil) abscess, neck phlegmon, purulent otitis and mastoiditis (inflammation of the mastoid process of the temporal bone), sinusitis and sepsis. In these cases, immediate resuscitation and surgical actions are needed. But the most disabling complications are associated with autoimmune reactions when acute rheumatic fever . The full picture includes five symptoms: inflammation of the tissues of the heart, migratory polyarthritis, chorea, annular erythema and rheumatic nodules on the skin. It develops more often in children 7-15 years old, this is due to the epidemiology of scarlet fever and streptococcal infections. In adults, chronic forms are more often detected. According to the State Statistical Report in Russia in 2014, the prevalence of rheumatic fever is:
- 1.8 per 100 thousand children from 0 to 14 years - acute forms;
- 11.8 per 100 thousand children and 118.4 per 100 thousand of the total population are chronic forms [12].
Late complications
Late complications include diseases that are not directly related to the pathogen and are caused by impaired immune response: carditis, arthritis, chorea and glomerulonephritis.
Carditis occurs with inflammation of the heart valves, the mitral and aortic valves are most often affected, valvular insufficiency and regurgitation develop (backflow of blood through the valves). On examination, an organic systolic murmur is heard. Treatment with anti-inflammatory drugs does not always lead to improvement, and in some cases chronic heart disease develops. Against the background of blood volume overload, the symptoms of heart failure intensify. Then the patient requires surgical treatment with valve surgery.
Arthritis is an inflammation of mainly large joints, accompanied by pain, swelling, and stiffness in movement. It is characterized by damage to several joints, most often the knees and ankles, and migratory inflammation. Good response to anti-inflammatory therapy. In case of inadequate treatment and genetic predisposition, a chronic course of arthritis develops with repeated attacks and joint deformation.
Chorea sometimes occurs after 6 months. A person develops gait disturbances, involuntary, uncontrolled movements of the arms, legs, body, and facial expressions, which are usually excessively expressed. From the outside, the condition resembles dancing, hence the name. On examination, muscle tone is reduced, reflexes are animated, sweating is pronounced, temperature is unstable, and excessive emotionality is present. Long-term antibiotics, anti-inflammatory and anticonvulsant drugs are effective in treatment.
PANDAS syndrome stands for Pediatric Neuropsychiatric Autoimmune Disorder. The complication was discovered relatively recently, at the end of the 20th century. The characteristic symptoms of this disorder are obsessive-convulsive seizures. The patient develops obsessive thoughts and movements, motor or vocal tics, emotionality and memory impairment may appear. With antibacterial and immune therapy, improvement occurs, but with repeated streptococcal infection or a stressful situation, the symptoms return.
Glomerulonephritis is an autoimmune kidney disease. Characteristic symptoms are edema, dysuria (impaired urination), hematuria (blood in the urine), increased blood pressure, and renal failure. Assessing a general urinalysis helps in diagnosis, especially with mild symptoms. In therapy, water and salt are limited, antibiotics, diuretics, antihypertensive, anti-inflammatory drugs are used, and in case of renal failure - dialysis [12][13].
Atypical forms of chickenpox in adults
In adults, chickenpox is accompanied by symptoms of intoxication of the body. Atypical clinical forms are also possible:
- Rudimentary. The rash is either absent or does not develop beyond the blotchy stage.
- Hemorrhagic. A bloody impurity appears in the blisters, and small hemorrhages appear on unaffected areas of the skin. Black crusts form.
- Bullous. Along with the usual chickenpox, other blisters appear. They are filled with a cloudy yellowish liquid and take a long time to dry. If such blisters burst prematurely, the area of skin underneath them becomes wet for a long time and does not heal.
- Gangrenous. The tissues inside the blisters die, and ulcers form underneath them. Cleaning of pus is often required.
The generalized form of chickenpox is considered separately. It is characterized by damage to internal organs. It is difficult to tolerate and there are deaths. At risk are patients taking steroid hormones.
Enterovirus infection in children and adults: signs, treatment
14.06.2017
Enterovirus infection in children and adults: signs, treatment
Acute infectious diseases caused by intestinal viruses belong to the group of enteroviral infections.
The pathology affects various human organs and is manifested by fever and a wide range of clinical signs. Enterovirus infection is characterized by outbreaks of mass diseases, especially in children's organized groups and families. The risk group includes people with reduced immunity - children, the elderly, people with chronic pathologies. Enterovirus infection is characterized by high susceptibility of the population and seasonality - an increase in incidence in the summer-autumn season. A feature of enteroviruses is the ability to cause clinical symptoms of varying intensity: from mild discomfort to the development of paralysis and paresis.
Etiology
The causative agents of enterovirus infection are RNA-containing Coxsackie viruses, ECHO viruses, and polioviruses. Microbes have relatively high resistance to physical factors - cooling and heating, as well as some disinfectants. Prolonged boiling, disinfectants with chlorine, formaldehyde and ultraviolet radiation have a detrimental effect on viruses.
Enteroviruses remain viable in the external environment for quite a long time. High air temperatures and high humidity increase the lifespan of the virus.
Sources of infection are patients and virus carriers.
Infection occurs through:
- Dirty hands, water, vegetables and fruits
- When talking, coughing, sneezing.
- When the pathogen is transmitted from a sick mother to the fetus.
Microbes multiply on the mucous membrane of the pharynx and accumulate in nasopharyngeal discharge, feces, and cerebrospinal fluid.
During the incubation period, the virus is released into the environment in small quantities. Patients remain dangerous to others for a month, and in some cases longer. Microbes enter the mucous membrane of the esophagus and upper respiratory tract, multiply and cause local inflammation, which occurs in the form of respiratory disease, pharyngitis, sore throat and intestinal upset. The period of reproduction and accumulation of viruses coincides with incubation and ranges from one to three days. Pathogenic biological agents enter the cervical and submandibular lymph nodes. At this time, patients develop pharyngitis and diarrhea. With the blood flow, microbes spread throughout the body, affecting internal organs with the development of another pathology and the appearance of corresponding symptoms.
Symptoms
Enterovirus infection often occurs without any characteristic symptoms and resembles a common cold. Viruses, affecting various organs and systems, usually cause herpangina, hemorrhagic inflammation of the conjunctiva, fever, gastroenteritis, and in rare cases, severe diseases: inflammation of the brain, liver, myocardium.
Symptoms of enterovirus infection:
Increased body temperature, feeling hot Thirst, dry mouth, weakness. The appearance of a characteristic rash Inflammation of the respiratory system, redness and inflammation of the oral mucosa. Frequent loose stools, abdominal pain.
Persons with strong immunity and a relatively healthy body rarely suffer from severe enteroviral diseases. Their infection is usually asymptomatic. Newborns, small children, elderly people and those weakened by chronic diseases are more susceptible to the development of enteroviral meningoencephalitis, hepatitis, myocarditis, and paralysis. Herpetic tonsillitis, acute respiratory infections and pharyngitis are less severe, but are accompanied by a persistent, painful cough.
Herpangina is one of the most frequently occurring forms of enterovirus infection. Its causative agents are Coxsackie viruses. The disease manifests itself with symptoms of intoxication and catarrhal syndromes.
Herpetic (herpetic) sore throat
Herpangina begins acutely. The body temperature of patients rises to 40 degrees, nausea, malaise, and headache occur.
Around the second day, signs of catarrhal inflammation of the pharynx appear.
After a couple of days, papules form on the tonsils, arches, tongue and palate, which eventually turn into red blisters. They burst, forming erosions on the mucous membrane, covered with plaque, which resolve without a trace in 5 days.
Lymph nodes are slightly enlarged.
Sore throat with herpangina is often absent or appears only during the formation of erosions.
acute respiratory infections
The respiratory form of enterovirus infection is manifested by symptoms similar to ARVI of any other etiology. Patients complain of fever, sore throat, hoarseness, dry cough, runny nose and nasal congestion. Usually these signs are combined with symptoms of indigestion.
The temperature remains high for 4-5 days and then gradually decreases. Other signs of the disease remain for another 2-3 weeks.
The catarrhal form is more common than others and occurs as pharyngitis, laryngitis, rhinitis or combined pathology. In young children, a symptom occurs that requires special attention. This is a barking, dry cough that makes it difficult for a child to breathe, especially at night. Attacks of “false croup” pose a great danger to children's health.
The cold-like form of enterovirus infection usually does not last long and is rarely accompanied by complications.
Enteroviral exanthema
In patients with enterovirus infection, from about 2-3 days of pathology, a rash appears on the skin in the form of pink spots and papules, often with hemorrhages. For two to three days, the rash remains on the body, and then gradually disappears without a trace. Exanthema is often combined with herpangina, stomatitis and meningitis.
Rare clinical manifestations of enterovirus infection:
Anicteric hepatitis, Meningoencephalitis, Inflammation of the optic nerve, Inflammation of the myocardium and pericardium, Lymphadenitis, Nephritis, Paralysis and paresis.
Complications
Inflammation of the brain and peripheral nerves are the most common and dangerous complications of enterovirus infection.
Patients who consult a doctor late and have a severe form of pathology may develop life-threatening diseases - cerebral edema, respiratory and cardiac arrest.
In young children, ARVI of enteroviral etiology is often complicated by the development of “false croup,” and in adults, by secondary bacterial infection with the development of bronchopneumonia.
Features of pathology in children
Enterovirus infection in children occurs in the form of sporadic diseases, but more often in the form of epidemic outbreaks in organized children's groups. The incidence increases in the warm season. For children of preschool and primary school age, the fecal-oral mechanism of transmission of the pathogen is characteristic.
Enterovirus infection in children usually occurs in the form of sore throat, serous inflammation of the meninges, and paralysis.
The pathology clinic is developing rapidly. The temperature rises sharply, chills, dizziness and headache appear, sleep and appetite are disturbed. Against the background of severe intoxication, characteristic signs begin to appear - tonsillitis, catarrhal inflammation of the nasopharynx, myalgia, stool disorder, enteroviral exanthema.
Enteroviral stomatitis
Enteroviral stomatitis develops in children aged 1-2 years after enteroviruses enter the body.
Symptoms of the disease are:
- Pain when swallowing
- Increased salivation
- Low-grade fever,
- Arthralgia and myalgia,
- Runny nose,
- Sore throat,
- Chills,
- Malaise,
- Swelling of soft tissues in the mouth.
The child becomes lethargic, restless, and capricious.
Typical vesicles with a characteristic red rim appear on the skin and mucous membranes. The rashes hurt and itch. These symptoms intensify with the appearance of new lesions. The disease develops quickly: blisters appear on the third day of infection, and on the seventh day the patient recovers.
Typically, enteroviral stomatitis is combined with exanthema, gastroenteritis, fever, and sore throat. In more rare cases, stomatitis is asymptomatic.
Diagnostics
Diagnosis of enterovirus infection is based on characteristic clinical symptoms, patient examination data, epidemiological history and laboratory test results.
Material for research - a swab from the throat, discharge from oral ulcers, feces, cerebrospinal fluid, blood.
Virological testing is the main diagnostic method. To detect enteroviruses, the following are used: PCR, serodiagnosis, molecular biological method, immunohistochemistry.
All of these methods are rarely used in mass examination of patients, since they are lengthy, complex and do not have high diagnostic value, which is associated with a large number of asymptomatic carriers of enteroviruses.
Treatment is prescribed by a doctor!
Treatment of enterovirus infection includes:
- Compliance with the regime
- Balanced and rational nutrition,
- Taking multivitamins,
- Etiotropic and pathogenetic therapy.
Regimen and diet
Mild and moderate forms of pathology are treated at home with strict bed rest. Patients with severe forms, prolonged fever and complications are hospitalized.
Patients are prescribed a diet that reduces intoxication, increases immunity, and spares the digestive organs. The patient's diet should contain sufficient amounts of protein, vitamins, and minerals. Drinking plenty of fluids is recommended to detoxify the sick body.
Pregnant women and children should be under the supervision of a specialist throughout the entire illness. Only a doctor, after making a diagnosis, should prescribe medications and their dosages allowed for a certain period of pregnancy and age group.
Self-medication of enterovirus infection is strictly prohibited. This is due to the nonspecificity of the symptoms of the disease, the possibility of confusing the pathology and being treated incorrectly.
Prevention
Specific prevention for enterovirus infection has not been developed.
Main events:
- Isolation of the patient
- Disinfection of the premises,
- Regular ventilation
- Compliance with hygiene standards and rules,
- Observation of contacts for 2 weeks,
- Use of Grippferon or Interferon drops for prophylactic purposes,
- Conducting hygiene education for children and adolescents,
- Maintaining personal hygiene rules
- Avoid hypothermia and drafts,
- Take vitamin complexes twice a year,
- Handle food correctly
How to help with chickenpox?
There is currently no cure for chickenpox. Usually the disease goes away on its own, and therapy is limited to smearing the rash with aniline dyes with bactericidal properties. A solution of brilliant green (“zelenka”) is usually used. You can take an antipyretic to relieve your general condition.
To relieve itching use:
- solution of iodine tincture (2-3%);
- solution of potassium permanganate (1:5000);
- hydrogen peroxide (3%);
- glycerol.
In some cases, antihistamines can help relieve itching. But you should not take them uncontrollably: it is better to call a doctor at home and determine acceptable medications. Showering is allowed, but without a washcloth to avoid damaging the bubbles. The same applies to the use of towels - after water procedures, you need to carefully pat your body dry with a cloth.
Akriderm GK preparations for hand allergies
Depending on the form of the disease and the severity of the course, both ointment and Akriderm GK cream are used. They have a similar composition; the main difference is that the cream has a softer texture, so it is absorbed faster by the skin. It is more appropriate to use it for the treatment of acute and subacute conditions, as well as for weeping and thin areas of the skin. In turn, the ointment stays on the skin longer and has a high penetrating ability, therefore it is suitable for chronic inflammation accompanied by severe dryness and flaking.[10]
When Akriderm GK is applied to damaged skin, the preparations soften and cool the affected area, relieving itching and redness. The active substances not only improve symptoms, but also help eliminate pathogenic microorganisms. Thanks to the combined composition, which includes several active substances and auxiliary components, the treatment brings a noticeable and long-lasting effect.[11]
Complications of chickenpox
In most cases, this disease is not dangerous; children tolerate it easily. The only threat is infection of the wound when combing with dirty hands. In such cases, staphylococci or streptococci may be ingested and a purulent infection may develop.
The chickenpox virus does not disappear from the body after recovery. Temporarily neutralized, it is localized in the spinal cord. As years pass, it can become more active and cause shingles.
In adults, complications may include:
- stomatitis (if a rash appears in the mouth);
- conjunctivitis (on the eyelids);
- inflammation of the middle ear.
The greatest danger is chickenpox pneumonia with a mortality rate of 40%. The consequences of infection with the chickenpox virus can manifest themselves in the form of neurological disorders, heart disease, and joint damage. A month after recovery, there is a risk of developing retinal inflammation and cranial nerve palsy.
Causes of allergic pharyngitis:
- strong odors (perfumes and chemical sprays, cigarette smoke and exhaust fumes);
- flowering period;
- book and house dust;
- pet hair;
- Food;
- medicines.
The development of the disease is often influenced by heredity, weak immunity, and chronic foci of infection. Allergic pharyngitis can also be triggered by hypothermia, smoking, etc. People who work in the production of chemicals are often at risk.
What is chickenpox pneumonia?
This is a lung lesion that occurs in 16% of cases of chickenpox and in almost all cases if the disease occurs in a generalized form. The first symptoms may appear simultaneously with the rash:
- dyspnea;
- chest pain;
- cough with sputum (often with blood);
- bluishness of the skin.
Multiple focal nodules spread in the lungs, which on x-ray look like tuberculosis. Antibiotics do not help in this case. Against the background of chickenpox pneumonia, bronchitis often develops; in severe cases, pulmonary edema is possible.
Pneumonia that develops in the later stages of chickenpox is considered separately. It is caused by a secondary coccal infection and is a common pneumonia. The disease is treated according to the standard regimen - penicillin.
Rashes on the hands: the most common diseases
In order to choose the right treatment, it is important to distinguish one type of allergic dermatosis from another. Therefore, let’s look at the symptoms of skin diseases in more detail:
- With atopic dermatitis (neurodermatitis), a rash often appears on the skin of the fingers and hands. The acute period of the disease is characterized by severe itching, redness and swelling of the skin. Itchy spots can come in different shapes and sizes. Without proper treatment, crusts may form at the site of the rash. In the chronic form, symptoms such as dry skin and flaking are observed.[3]
- Urticaria is divided into several types: immunological, physical, drug and idiopathic. The development of the first two is based on the body’s reaction to external stimuli, including food and household allergens, as well as high or low temperatures, sunlight and other factors. Taking certain medications can trigger drug-induced urticaria. Idiopathic is a rash whose cause cannot be determined.[4] All types of hives present more or less the same way: redness, swelling of the skin and the appearance of itchy blisters.
- Contact dermatitis often affects the skin on the fingers, especially when coming into contact with harmful substances such as rubber and metal products, household chemicals, cosmetics and perfumes, topical medications, certain plants and insects.[5] The disease can occur in both acute and chronic forms. The acute course is characterized by redness of the skin and the appearance of itchy blisters. The chronic form is accompanied by dryness and flaking of the skin, increased skin pattern.
- Eczema is an acute and chronic inflammatory disease that affects both the upper and lower extremities. It may also affect various parts of the body. As a rule, eczema rashes are symmetrical, accompanied by redness and limited swelling of the skin. Small blisters filled with clear liquid often appear on affected surfaces.[6]
Neurological complications of chickenpox
The consequence of infection with a herpes virus in an adult can be secondary encephalitis. Inflammation develops from the fifth to tenth day of the rash, sometimes even after recovery. The pathological process can be localized in different places:
- membranes of the brain (meningitis form);
- cerebellum (atactic form);
- spinal cord (myelitic form).
- Combined damage to the brain and spinal cord (encephalomyelitis, meningoencephalitis) is also possible.
In mild cases, damage to the central nervous system by the chickenpox virus leads to loss of coordination, involuntary eye movements, hand tremors, and dizziness. In more severe cases, vision suffers (up to its complete loss). The most dangerous complication is paralysis. Mental damage, even mental retardation, is also possible.