Stomatitis, which occurs in the human oral cavity, is considered primarily a childhood disease, but in fact, more than 20% of adults periodically face a similar problem. This disease manifests itself in the form of yellowish-gray ulcers on the upper or lower palate, throat or tongue of a person.
Stomatitis ulcers that form in the throat cause significant discomfort to an adult or child. Therefore, it is necessary to begin treatment for this disease as soon as possible and take measures to eliminate the symptoms of stomatitis in the mouth. LeaderStom dentistry will tell you about the causes of stomatitis ulcers in the throat and how to cure this disease and avoid possible complications.
What is stomatitis?
Stomatitis is an inflammatory disease of the oral mucosa. It occurs for various reasons - due to bacterial, viral or fungal infections, due to injuries, biting the tongue or cheek, rubbing the gums with a prosthesis, etc. If we keep in mind the various causes of occurrence, different localization and nature of the course, then we can even say that stomatitis is not one disease, but a whole group with similar symptoms.
Many people are interested in whether stomatitis is contagious. No, it itself is not contagious, but if you consider that it can be caused by a viral or bacterial infection, then contact with the patient must be limited - no kissing or drinking from the same cup. This is especially true for children, since they are more direct in expressing feelings and tend to often forget about hygiene requirements.
Considering the question of how stomatitis is transmitted, we emphasize once again that stomatitis as an inflammation of the mucous membrane is not transmitted to other people. But if it is caused by a herpes virus, streptococcal or candida infection, then the patient may well transmit this infection to others through close contact (for example, parents often try baby drink by drinking from the child’s cup - this cannot be done with stomatitis). Whether this infection will lead to a similar disease in the infected person largely depends on his individual immunity.
Sometimes they ask how long it takes for stomatitis to go away. It is important to understand that this directly depends on the cause of the disease, the stability of the immune system and the treatment methods used. If acute stomatitis is caused by injury (for example, a burn from a hot drink or injury to the mucous membrane by a sharp edge of a tooth), and the immune system is strong enough, then the disease can go away in 3-4 days. If the cause is infection, but the patient strictly follows the doctor’s recommendations, then treatment of the acute phase of the disease may take 10-14 days. With reduced immunity (diabetes mellitus, HIV and other problems), treatment of stomatitis may be delayed indefinitely.
In the mouth, stomatitis can have different localizations. Simply put, the lesion can affect various places on the tongue, gums, roof of the mouth, lips and even the throat. As a rule, this does not affect the treatment method, but it can simplify, or, on the contrary, complicate treatment (if the damage affects hard-to-reach or constantly exposed areas).
Stomatitis on the lip occurs almost most often. Often it is the herpes virus that causes painful swelling, pimples or sores on the lips. At the same time, damage to the mucous membrane of the lips may be a symptom not of stomatitis, but of a lack of B vitamins.
Stomatitis on the palate is also one of the characteristic signs of herpetic stomatitis. But it can also be caused by other reasons.
Stomatitis on the tongue often occurs as a result of biting, injury from a chipped tooth with a sharp edge, or a burn. If the tongue is covered with a white cheesy coating, then it may be candidal stomatitis.
Stomatitis on the gums can be the result of tooth extraction, damage from a toothbrush with too hard bristles, or pieces of hard food.
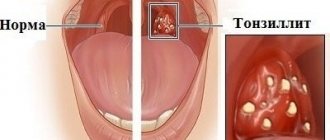
Stomatitis in the throat is sometimes confused with sore throat. The symptoms are similar - sore throat, especially when swallowing, redness, increased salivation. But if a careful examination reveals blisters and ulcers, then this is most likely stomatitis.
You need to know that the location of ulcers, redness and swelling in a particular place is not an unambiguous sign of a particular type of stomatitis. The reasons must be determined by a doctor based on examination and test results.
Stages of stomatitis
According to the clinical picture, three types of stomatitis are distinguished.
Catarrhal stomatitis
The most common type of stomatitis, caused by poor oral hygiene, tartar and dental diseases. The mucous membranes become inflamed, red and swollen, but there are no ulcers or deep defects. Accompanied by bad breath, increased salivation, dryness and soreness of the mucous membranes.
For catarrhal stomatitis in the mouth in adults, treatment is first of all aimed at relieving inflammation, for which antiseptic solutions, rinses, lozenges, etc. are used. A gentle diet is required to avoid further injury to the mucous membranes.
After eliminating the symptoms of stomatitis, you can treat your teeth and carry out professional hygiene to get rid of tartar and prevent the occurrence of stomatitis in the future.
Ulcerative stomatitis
As a rule, this is the next stage of catarrhal stomatitis. The smell from the mouth intensifies, ulcers with a gray coating appear, eating is accompanied by pain. In some cases, the temperature rises and the lymph nodes become enlarged.
At this stage, only the doctor decides how to treat severe stomatitis and what combination of drugs is suitable in this case: they usually combine painkillers, antihistamines, vitamins, healing agents with antibiotics and treatment of rashes.
Aphthous stomatitis
At this stage, aphthae gradually form - round or oval erosive surfaces 3-5 mm in diameter with a red border and a gray-yellow coating. Aphthae can be single rashes or massively cover the inside of the cheeks and lips, the sides of the tongue, and the palate. Methods for treating stomatitis on the palate in adults depend on the severity of the stage and cause of the disease.
Types and forms of stomatitis
What types of stomatitis are there? Depending on what is taken as the basis for the classification, various forms and varieties of this disease can be distinguished. For example, according to the degree of damage to the mucous membrane, a distinction is made between catarrhal (superficial) stomatitis and ulcerative stomatitis.
According to the causes of occurrence, traumatic stomatitis, bacterial, candida, viral, prosthetic, drug, allergic and radiation are distinguished. The nature of the course of the disease and the presence of relapses make it possible to determine such forms of stomatitis as acute and chronic stomatitis.
To accurately determine the type of stomatitis in a particular case, it is necessary not only to carefully examine the oral cavity, but also to conduct tests for the presence of certain pathogens, and also take into account the presence of allergic reactions in the patient, chronic diseases (such as diabetes or gastritis) , pathologies of the immune system.
Chronic
Chronic stomatitis usually occurs as a continuation of advanced acute stomatitis and is characterized by a long course with periodic remissions and exacerbations. By origin, this is most often viral (herpetic) stomatitis. After treatment, the virus remains in the body and when the immune system is weakened again (due to stress, illness or other reason), it is activated and leads to relapse of stomatitis.
Chronic recurrent stomatitis can be not only viral in nature, but also bacterial, allergic, and candidiasis. The causative agents of many diseases are constantly present in the body, or easily enter it from the external environment. And if stomatitis was caused by an allergy to some substance or exposure, then it is very likely that with each contact with this allergen the stomatitis will return again.
Treatment of chronic stomatitis always includes the use of specific therapy aimed at suppressing the pathogen: antibacterial, antiviral, antifungal. It is also necessary to eliminate foci of infection (for example, carious cavities) and complete sanitation of the oral cavity with professional hygiene.
Bacterial
Bacterial stomatitis is caused by pathogenic microorganisms (for example, streptococci or staphylococci) that enter the oral cavity or are already in it (for example, in carious cavities, in the thickness of tartar) and infect the mucous membrane. This is facilitated by injury to the mucous membrane with sharp edges of teeth, rubbing dentures, or other objects.
Treatment of bacterial stomatitis involves the use of antiseptic and antibacterial agents. If the cause of stomatitis is a denture, then it should be cleaned with special means (for example, in an ultrasonic bath), or replaced with a more comfortable one.
Angular
Angular stomatitis is associated with the appearance of cracks in the corners of the mouth (“jams”). The main causes of this disease are lack of vitamins and bacterial (or fungal) infection. This type of stomatitis is characterized by damage to the outer surface of the lips.
Treatment for angular stomatitis depends on the type of infection. For fungal infections, fungicidal ointments and preparations are used. The streptococcal variety requires the use of antibacterial agents. Treatment is complemented by taking vitamins, eliminating their deficiency and raising the level of immune defense.
Viral
Viral stomatitis is caused by infection of the body with a virus. Most often (in about 80% of cases) this is the herpes virus. But besides it, stomatitis can be caused by almost any virus - chickenpox, measles, influenza, adenoviruses or rotaviruses. Typically, the onset of the disease is typical for a viral infection of this type - it may be fever, chills, runny nose, cough, or swollen lymph nodes. But after 1-3 days, characteristic symptoms of viral stomatitis appear: blisters form in the mouth, which later turn into ulcers, swelling of the gums, bleeding, and putrid breath may occur.
Viral stomatitis can be considered a complication of the underlying viral infection. Its causes (in addition to the virus itself) are reduced immunity and poor oral hygiene - the presence of untreated caries, periodontal disease, gingivitis.
Treatment of viral stomatitis involves first of all treating the underlying disease. In addition, the affected areas of the mucosa can be treated with local antiseptic drugs, anti-inflammatory and wound healing agents. Often in such cases, antiviral ointments or gels are prescribed, and vitamins, immunomodulators, and adaptogens are prescribed to maintain and strengthen the immune system.
Allergic
Allergic stomatitis is caused by exposure to allergens. In addition to the typical allergens that are well known to us, such as animal fur, pollen, foods such as honey, citrus fruits, etc., allergies can be caused by some medications, dental products and orthodontic structures (for example, acrylic dentures).
It often happens that an incorrectly manufactured prosthesis (for example, with a violation of the proportions of the material components) causes an allergic reaction and, as a result, stomatitis. When replacing the prosthesis with a correctly made one (without excess monomer in the composition), the allergy disappears. Symptoms of allergic stomatitis are redness of the mucous membrane (and with prosthetic stomatitis, this can be not only the areas under the prosthesis, but all parts of the tongue, cheeks, etc., in contact with the prosthesis), swelling, itching, and subsequently small blisters appear, often turning into sores.
When treating allergic stomatitis, it is important first of all to determine the cause of the allergy and remove contact with the allergen (eliminate foods that cause allergies, or replace the denture if this is the cause), and take antihistamines. The rest of the treatment involves the use of local antiseptic, anti-inflammatory and analgesic agents.
Herpetic
Herpetic stomatitis is one of the contagious forms of stomatitis. Moreover, contagiousness persists even for 2 weeks after recovery. In most cases, the herpes virus never completely leaves the infected body. It is in a dormant, inactive form, but can be activated when immunity decreases - due to stress, lack of vitamins, due to a severe respiratory disease. Therefore, herpetic (cold sore) stomatitis is often chronic.
An adult very often does not have a strong reaction to the effects of herpes and damage to the mucous membrane. In children, acute herpetic stomatitis can be accompanied by an increase in temperature, general intoxication; when the bubbles merge, burst and form erosion, the child may feel severe pain, which interferes with eating, drinking, and talking. Most often, rashes appear on the palate, tongue, and inner surface of the cheeks. But often they also affect the lips and gums. The danger of this type of stomatitis is that it can turn into gingivitis, so it must be treated.
Treatment of herpetic stomatitis always involves suppressing the herpes virus. Antiseptics (chlorhexidine) and even many antiviral drugs do not affect the herpes virus. Moreover, antibiotics have no effect on him. Special medications have been developed against herpes - acyclovir, valacyclovir, famciclovir. They should be taken only as prescribed by a doctor, in case of severe herpetic stomatitis.
Among the local antiseptics, you can use Miramistin (effective against both types of herpes viruses) and Hexoral (active only against HSV-1). Anti-inflammatory drugs (cholisal) and wound-healing agents (solcoseryl, actovegin, sea buckthorn and rosehip oil, vitamins A and E) perform well.
Candida
Candidal stomatitis often occurs in children under 3 years of age and is therefore often called childhood thrush. This disease is caused by the fungus Candida. It is distinguished by a characteristic white cheesy coating, which is practically impossible to remove mechanically. When trying to remove it, the patient experiences pain, and under the plaque a bleeding, swollen surface of the mucous membrane is found. At the onset of the disease, a person may feel dry mouth, a burning sensation, and white dots appear that merge to form a continuous plaque.
The decision on how to treat candidal stomatitis should be made by a doctor, especially when it comes to a child. For adults, antifungals and topical medications (such as candida) are almost always prescribed. Treatment of candidal stomatitis in children is often limited to the use of vitamins and immune-strengthening agents. To eliminate symptoms, use alkaline rinses and lubricate the mouth with iodine. Antifungal drugs are used only in cases of severe candidomycosis stomatitis.
Ulcerative
Ulcerative stomatitis is a more severe form of the disease than catarrhal stomatitis. Its peculiarity is that the lesion covers the entire thickness of the mucosa, in contrast to the catarrhal form, where it affects only the superficial layers. Deep damage to the oral mucosa causes great suffering to the patient, and after the ulcers heal, scars often remain. Treatment for ulcerative stomatitis depends on the cause of the disease. If an infection is present, antibacterial, antiviral or antifungal therapy is carried out, as well as a course of restoratives and vitamins. Treatment is carried out with means for topical use - antiseptic drugs (furacilin, chlorhexidine, miramistin), herbal decoctions, healing agents. If the cause is traumatic damage to the mucosa, dental procedures are indicated: removal of decayed teeth, treatment of caries, professional oral hygiene.
Vesicular
Vesicular stomatitis is most often enteroviral. It is usually transmitted from animals (or from people who are carriers of the virus) - by airborne droplets, contact and fecal-oral routes. Children most often suffer from it. One of the characteristic symptoms of this disease is a rash on the palms and soles (sometimes also on the face around the mouth, on the buttocks and genitals) - this is vesicular stomatitis with exanthema.
Watery rashes are quite painful and cause itching, which causes severe discomfort to the child, often leads to refusal to eat, and disrupts sleep. With proper timely treatment, the disease goes away without a trace, leaving lasting lifelong immunity. Unfortunately, there are several types of Coxsackie virus, so a person who has had vesicular stomatitis can become infected again with a different type of virus.
Treatment is mainly symptomatic and includes isolating the patient (to avoid infecting other people), taking painkillers, treating rashes with local antiseptics, using applications and rinses, taking vitamin complexes, and in some cases, antiviral and antihistamine drugs.
Aphthous
Aphthous stomatitis is characterized by the formation of aphthous stomatitis on the oral mucosa - one (less often two or three) round ulcers up to 1 cm in size, surrounded by a bright red border and covered with a gray-yellow coating. Touching them is very painful. Itching or burning is often felt before ulcerations appear. Other symptoms rarely appear - slight fever, weakness.
The cause of aphthous stomatitis is reduced immunity, the presence of foci of infection (chronic tonsillitis, pharyngitis, etc.), gastrointestinal diseases, allergic reactions (including to sodium lauryl sulfate contained in some toothpastes), trauma to the mucous membrane (biting), increased concentration of nitrates in food or drink.
If the situation of decreased immunity, exposure to infections or allergens is repeated, the disease may recur, taking on the character of recurrent aphthous stomatitis. With a mild course of the disease, there are no more than 2-3 relapses per year. More frequent attacks indicate a severe form of the disease.
Treatment of aphthous stomatitis involves eliminating contact with allergens, incl. Avoid toothpaste with sodium lauryl sulfate and avoid allergenic and acidic foods. Antihistamines are also often prescribed.
When deciding how to treat aphthous stomatitis, the doctor must conduct a thorough diagnosis and establish the cause of the disease. In accordance with this, a selection of antiseptic drugs (for example, miramistin or chlorhexidine), anti-inflammatory gels (for example, cholisal) and wound healing agents (solcoseryl) is made.
The severe course of chronic aphthous stomatitis often involves the use of more serious medications and methods: laser treatment, immunomodulators, glucocorticoids, but such drugs should be prescribed exclusively by the attending physician.
Symptoms
- redness of a local area of the mucosa (at the very beginning of the inflammatory process);
- swelling of the reddened area, burning and itching;
- the appearance of a round ulcer in the bacterial form (occurs within a day), the formation of a white coating in the fungal form or small blisters in the case of a viral infection;
- salivation gradually increases;
- the appearance of bleeding gums;
- unpleasant odor;
- increased discomfort, pain or burning sensation;
- Without treatment, your health may deteriorate and your temperature may rise.
If these symptoms appear, doctors at the Dentospas clinic recommend planning a visit to the dentist.
Causes
The question of why stomatitis appears has several possible answers. First of all, this is the body’s weak resistance due to age, lack of vitamins, severe stress or heavy physical activity. In addition, the harmful effects of allergens, new or existing infections in the body, and traumatic damage to the mucous membrane are important. So, all the variety of reasons can be reduced to several groups:
- weakening of the immune system for any reason (age, illness, stress, strain, bad habits, poor nutrition or environment),
- insufficient oral hygiene (presence of untreated caries, periodontal disease, gingivitis, hard plaque, infrequent or improper brushing of teeth),
- allergies (not only to foods, but also to medications, denture materials, dental products and pastes, food or vitamin supplements),
- injuries to the mucous membrane - mechanical (biting, hard and sharp food particles, rubbing dentures, blows, etc.) and thermal (burns from hot food or drink),
- infection entering the body (in children this is “disease of dirty hands”), or activation of microorganisms present in the body.
Bad habits have a great influence: for example, smoking damages the mucous membrane (with hot smoke, chemicals from smoldering tobacco), reduces immunity, and irritates the mucous membrane of not only the mouth and nose, but also the bronchi. Avoiding excesses and unhealthy foods, alcohol and tobacco significantly strengthens the immune system and prevents repeated relapses of stomatitis.
Causes of stomatitis
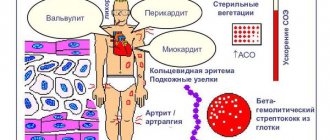
The mechanism of stomatitis, unfortunately, has not yet been fully identified, so there are many causes of the disease:
- microorganisms that cause infection, acting directly on the oral mucosa;
- diseases of the gastrointestinal tract;
- diseases of the cardiovascular system;
- general weakening of the immune system;
- avitaminosis;
- metabolic disorders;
- nervous disorders;
- malignant tumors;
- hormonal fluctuations;
- various injuries in the form of abrasions of the oral mucosa;
- anemia;
- heredity.
Among the causes of stomatitis there are also local factors. Elementary lack of oral hygiene, caries, dysbacteriosis, poorly made or poorly installed dentures, the consequences of using medications, nicotine and alcohol consumption, as well as allergic reactions to products. Of particular note is the use of toothpastes containing sodium lauryl sulfate. Various studies have proven that they provoke the occurrence of stomatitis and its exacerbation.
Signs and symptoms of stomatitis
The symptoms of acute stomatitis are very similar for different types of this disease, although there are differences that make it possible to more accurately diagnose the disease. The location of the rash does not always indicate the form or causes of the pathology. The symptoms of stomatitis on the tongue or in the throat are generally the same; much more important is the nature of the manifestations, the presence of rashes - small blisters or one large ulcer. The severity of the inflammatory process allows us to judge whether the disease is milder, catarrhal, or more severe. For example, the symptoms of catarrhal stomatitis include only:
- redness and swelling of the mucous membrane,
- soreness, sometimes bleeding gums,
- bad breath,
- increased (or, on the contrary, decreased salivation),
- Sometimes a white sticky coating appears.
But at the same time, there are no rashes or ulcers, the temperature rises very rarely and slightly, the lymph nodes are not enlarged. It would seem that this indicates the stability of the immune defense and an easy and quick cure, however, even this form of stomatitis needs treatment, otherwise, once neglected, it can become more severe, ulcers will appear, a bacterial infection will join, which will spread to neighboring organs, causing serious complications.
So, let us highlight the symptoms of the disease characteristic of stomatitis:
- redness and swelling of certain areas of the mucous membrane,
- blisters, blisters or sores (not always),
- pain, burning, itching in the affected areas, which intensifies when touched, eating, talking,
- bad breath,
- plaque (white or grayish-yellow) on the affected areas,
- fever, chills (not always, more often in children than in adults),
- signs of intoxication - weakness, headache, nausea (not always).
Symptoms of stomatitis in newborns are slightly different. Most often this is:
- temperature increase,
- baby's refusal to breastfeed,
- restlessness and moodiness of the baby,
- small blisters or sores on the oral mucosa.
The most common causes of stomatitis in newborns are the herpes simplex virus (65%) or the Candida fungus (30%). In the case of herpes, blisters with transparent contents appear on the mucous membrane, which soon burst, forming ulcers. With candidal stomatitis, white dots appear that merge to form a solid white coating. Since damage to the mucous membrane causes pain and burning, the baby refuses to eat, which is very dangerous, as it leads to weight loss and dehydration.
Temperature with stomatitis
The question of whether there can be a fever with stomatitis usually worries the parents of a sick child, who are trying to understand whether it is worth seeing a doctor. Yes, with stomatitis in children, the temperature very often rises. In general, the signs of stomatitis in children are usually more pronounced than in adults, due to the fact that the child’s immune system still reacts to infections and inflammation quite violently.
But even in adults with stomatitis, the temperature may rise, especially with a more severe course of the disease.
You need to know how long the temperature lasts for stomatitis. Usually this is several days, but depending on the cause of the disease and the severity of its course, this time may be shorter or longer. In any case, you should definitely consult a doctor - correct diagnosis and proper treatment can shorten this period and prevent the disease from developing into a complicated form.
Which doctor should I contact if I have signs of stomatitis?
Which doctor treats stomatitis? At the first signs of stomatitis, you should go to a doctor who treats diseases of the oral cavity - a dentist. He will determine the type of disease and its causes, prescribe treatment, and, if necessary, refer you for tests or to a specialized doctor to clarify the diagnosis.
If manifestations of stomatitis are noticeable in a child, then you should contact your local pediatrician.
Diagnosis of stomatitis
Successful healing requires correct diagnosis of stomatitis. Only a doctor with the necessary knowledge and professional experience can accurately determine the type of disease, establish the causes and propose treatment tactics taking into account the individual characteristics of a particular patient.
On the one hand, this disease has very characteristic symptoms and stomatitis is relatively easy to diagnose. On the other hand, stomatitis may be concomitant with another, more serious disease. The effectiveness of the medications and treatment methods used directly depends on the correct identification of the causes that caused stomatitis.
Treatment of stomatitis in adults
Adults usually tolerate stomatitis more easily than children, however, stomatitis in adults also requires treatment, since if it is neglected, it can become more severe, cause serious complications, and become chronic.
Treatment of stomatitis in adults should always be based on identifying the causes of the disease. If the cause is an allergy, then it is necessary to identify the allergen and eliminate contact with it. If the cause is a bacterial or viral infection, then a course of antibacterial or antiviral therapy should be administered. Depending on the specific diagnosis, the most effective painkillers, antiseptic, anti-inflammatory and healing agents in a particular case are selected. To the question - how to treat stomatitis in adults? — the dentist must answer. In no case should you self-medicate, as this can have the opposite effect and lead to a worsening of the situation.
Treatment of stomatitis includes:
- Elimination of the cause of the disease (allergy or viral infection, bacterial contamination).
- Local treatment - rinsing with antiseptics and herbal decoctions, using anti-inflammatory and healing gels.
- Suppression of acute conditions - reduction of high temperature, pain relief.
In addition to systemic treatment aimed at suppressing infection, antihistamines are often used, and local treatment - rinses, applications, ointments and gels, the purpose of which is to clean the surface of the mucous membrane from plaque with microorganisms, prevent the proliferation of pathogenic microflora, reduce inflammation, eliminate pain, and stimulate regeneration of damaged tissue.
How to rinse
Mouth rinsing for stomatitis is aimed at mechanical removal of dead epithelial cells, mucus containing pathogenic microflora, as well as the death of harmful microorganisms and suppression of their reproduction.
One of the best antiseptics is Miramistin - it has not only antimicrobial activity, but also antiviral activity (including against both herpes simplex viruses). It also restores local immunity of the mucous membrane.
The second rinse option is chlorhexidine. It has less antiviral protection, but more actively suppresses bacteria, and most importantly, it leaves an indelible layer of the drug on the mucous membrane, which prolongs the rinsing effect.
Furacilin and other antiseptics give good results. Hexoral contains not only an antiseptic, but also anti-inflammatory and analgesic components.
Rinsing with herbal decoctions helps with stomatitis: chamomile, sage, calendula, eucalyptus, etc. But you need to understand that these remedies are auxiliary, not primary - you should not rely on them alone in the treatment of such a serious disease as stomatitis.
Soda for stomatitis
Rinsing with soda for stomatitis has two advantages: first of all, soda softens and helps remove mucus and bacterial plaque. In addition, it creates an alkaline environment, which is destructive for many harmful bacteria, fungi and viruses.
Soda solution for stomatitis does not cause burning or pain, has no contraindications, and is suitable even for children. To prepare it, you need to dissolve 1 teaspoon in 200 ml of warm water. The solution will help reduce swelling and pain, soothe the mucous membranes, and slow down the development of harmful microorganisms.
Stomatitis during pregnancy
Stomatitis occurs very often in pregnant women. The reason for this is weakened immunity, lack of vitamins, and hormonal changes in the body. It is necessary to treat this disease only under the supervision of a doctor, since only a doctor can prescribe medications that will not harm the health of the mother and her unborn baby.
To avoid stomatitis during pregnancy, it is necessary to visit the dentist in advance and perform a complete sanitation of the oral cavity - cure caries, remove tartar, and solve all other problems. And also regularly and carefully care for your oral cavity throughout the entire period of pregnancy, take care of your health and follow all doctor’s recommendations.
Antibiotics for stomatitis
In all cases, antibiotics are prescribed only by a doctor. They are effective only against bacterial infections and the forms of stomatitis caused by them (for example, with Vincent's ulcerative necrotizing stomatitis). Viral types of stomatitis cannot be cured with antibiotics. The success of treating stomatitis with antibiotics directly depends on correct diagnosis and accurate selection of the most effective drugs and dosages in a particular case.
How to get rid of stomatitis
The best decision is to immediately consult a dentist. But if the disease takes you by surprise and medical help is temporarily unavailable, you should not be inactive.
Rinsing and irrigating the mouth with special preparations, such as HEXORAL®10,11, will help combat the symptoms of stomatitis.
HEXORAL® spray can be recommended for children over 3 years of age who do not yet know how to gargle independently and can swallow the solution. The drug contains hexetidine, a broad-spectrum antiseptic that is active against most bacteria, herpes simplex viruses type 1, influenza A, PC virus that affects the respiratory tract, and fungi. Due to the action of hexethidine and other components, the drug helps reduce pain and bad breath10.
HEXORAL® solution can be used as a mouth rinse. The procedure should be carried out after meals for 30 seconds 2-3 times a day. Hexethidine adheres to the mucous membrane, due to which it continues to act all the time between procedures11.
In addition, for stomatitis, areas of mucosal inflammation can be treated directly with HEXORAL® solution. In this case, the drug must be applied to the affected area using a swab or cotton swab, left for 2-3 minutes and then rinsed out. In some cases, this speeds up recovery11.
For stomatitis, HEXORAL® lozenges can also be used:
- HEXORAL® TABS based on chlorhexidine and benzocaine, which has an antiseptic and analgesic effect, approved for use by adults and children over 4 years of age12.
- HEXORAL® TABS CLASSIC with lemon, orange, blackcurrant, lemon and honey flavors for adults and children aged 6 years and older. The tablets are based on a combination of the antiseptics amylmetacresol and dichlorobenzyl alcohol13.
- HEXORAL® TABS EXTRA, which can be used for the symptomatic treatment of stomatitis in adults and children over 12 years of age. In addition to the antiseptic, it contains the anesthetic lidocaine, which can relieve even severe pain in the mouth14.
Important! Using the drug HEXORAL® does not replace visiting a dentist. Thus, for ulcerative and aphthous inflammatory processes, in addition to local treatment, general therapy may be required: antibiotics, antiallergic drugs, etc. In addition, dental treatment may be indicated to prevent stomatitis1.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Up to contents
Treatment of stomatitis in children
How to treat stomatitis in a child depends on the cause of the disease. Fungal candidiasis infection, or herpes virus, enterovirus require different treatment tactics and the use of different drugs. This is why it is important to see a doctor as soon as possible.
Children's stomatitis is usually treated with gentle means, limited to rinses, anti-inflammatory and painkillers, and vitamins. But in cases where the disease is more severe, antifungal, antibacterial or antiviral agents are used, the choice and dosage of which is prescribed by the attending physician.
Types of stomatitis
The treatment regimen for stomatitis in children is based on the type of disease. There are several types of stomatitis:
- bacterial;
- viral, including herpes;
- fungal;
- aphthous;
- angular;
- allergic;
- traumatic.
All types of stomatitis occur in children, but the most common among children under 3 years of age are aphthous, candidal, herpetic and allergic. An increase in the incidence of traumatic stomatitis is usually associated with a period of active growth of primary teeth.
It is important to understand that in some cases, stomatitis is combined with other diseases with similar symptoms and is the first sign of more serious diseases. For example, with cheilitis - inflammation of the mucous membrane and red border of the lips, food allergies, etc.
Stomatitis and coronavirus
There is a lot of talk now that many people develop stomatitis due to coronavirus. And so the question arises - how are they connected? It is quite obvious that coronavirus infection greatly weakens the body, undermines the immune defense, and leads to various complications. And with a decrease in immunity, as we know, many dormant infections in the body are activated, which lead to stomatitis. Therefore, it is impossible to consider stomatitis as a symptom of Covid. But it is more logical to look at stomatitis as a concomitant disease that occurs in approximately half of those suffering from coronavirus infection.
After coronavirus, stomatitis can also occur as one of the possible complications. Particularly susceptible to this are those patients who did not closely monitor the condition of the oral cavity, rarely visited the dentist, who had advanced caries or problems with the gums (gingivitis, periodontitis), and tartar deposits. In order to avoid contracting stomatitis after Covid, it is important to regularly and thoroughly perform oral hygiene, brush your teeth, and visit the dentist in a timely manner.
Stomatitis rarely occurs after vaccination against coronavirus. Some patients have a more difficult time with vaccination, so a decrease in immunity may result in a recurrence of stomatitis, especially in those who have had it before or in those who are at risk.
Stomatitis in the throat and its symptoms
Stomatitis in the throat is usually called damage to the mucous membrane by ulcers. The course of the disease is complicated by the localization of the ulcers. The surface of the tonsils and tonsils is too sensitive; when redness appears, it becomes painful and causes discomfort to the patient. When the first ulcers appear, the pain intensifies and even leads to restriction of drinking and nutrition.
Stomatitis in the throat occurs for various reasons
Treating affected surfaces is not easy; the course of the disease is especially painful for young children, who completely refuse to eat because of the pain caused.
It is important not to miss the first symptoms of throat stomatitis and start treatment as early as possible:
- general malaise
- muscle pain
- the onset of the inflammatory process may be accompanied by an increase in body temperature to 37.5
The disease then develops:
- Effective remedies and recipes for treating mouth ulcers
- an unpleasant burning sensation in the mouth and throat;
- swelling in the throat, redness appears;
- pain when swallowing;
- rashes appear in the form of whitish-gray spots on the tonsils and throat; both single spots and small multiple rashes may appear;
- the base of the tongue is covered with a white coating;
- the lymph nodes located under the jaw become inflamed.
When children become ill, their appetite worsens, they refuse to eat, cry, are capricious, and salivate profusely.
A child’s temperature can rise higher than an adult’s, up to 38-39 degrees. Children experience the disease more painfully and the symptoms are more pronounced.
The symptoms are very similar to the onset of a common cold or sore throat. Moreover, not everyone knows whether there can be stomatitis in the throat. Whitish spots on the tonsils are very easy to confuse with purulent sore throat due to lack of awareness.
Therefore, treatment is often delayed. As a rule, the disease is recognized already at the stage of the appearance of characteristic ulcers, which can be seen in the photos offered on the Internet. But you should not rely on your own strength in recognizing and treating the disease from a photo. Stomatitis in the throat in children can manifest itself in different ways, so if you have similar symptoms, consult a specialist.
Stomatitis in the throat
Traditional methods of treatment
The main weakness of attempts to cope with stomatitis using traditional techniques and methods is that it is not always possible to accurately determine the type and cause of the disease on your own. This means that the means chosen are not always effective in this particular case. Nevertheless, traditional treatment for stomatitis is quite capable of helping to cope with the disease in a number of cases, especially when the disease is mild.
At the same time, you need to be aware that not all folk remedies for stomatitis are effective. For example, blue (methylene blue dye) has such weak antiseptic properties that its use is simply pointless.
Herbal decoctions have a positive effect on the oral mucosa, softening, providing an antiseptic, healing effect, but it is most often quite weak, so they should not be considered as the main means of treatment. The best folk remedies:
- propolis - it is used in the form of an alcohol tincture, but before applying to the affected mucous membrane, the tincture must be diluted; propolis has a disinfectant and even a slight analgesic effect;
- chamomile flowers - used in the form of a decoction as a disinfectant, anti-inflammatory and sedative;
- oak bark - its decoction strengthens inflamed tissues of the gums and oral mucosa, reduces pain;
- sage - a decoction of its leaves relieves pain, suppresses inflammation of oral tissues;
- sea buckthorn oil - reduces pain, has a strong regenerating effect, helping to heal ulcers and cracks.
Treatment of stomatitis with folk remedies should not be opposed to medical technologies. Many modern doctors allow the use of folk remedies that have proven effectiveness or at least useful substances in their composition, and even recommend them as an aid.
Symptoms of the disease and its complications
Aphthous stomatitis does not begin with the formation of ulcers. The stages of the disease are:
- The lymph nodes become inflamed, the temperature rises and general weakness occurs.
- Small blisters form in the mouth, which spontaneously open and turn into aphthae.
- Salivation increases.
- At first, it is unpleasant for the patient to eat food with a pronounced taste, and then chewing any food causes pain.
- With a persistent form of aphthous stomatitis, the lymph nodes become inflamed and become painful on palpation.
- The mucous membranes of the mouth are loose and inflamed.
- A white coating appears on the tongue.
- At the final stage of the disease, aphthae scar, and soreness in the mouth disappears.
If the patient has not received adequate treatment, aphthous stomatitis becomes chronic. Wherein:
- The mucous membranes swell and turn pale.
- Aphthae grow and cover the inner surface of the cheeks, palate and back of the tongue. In advanced forms, the ulcers rise above the surface of the oral mucosa.
- Without receiving proper treatment, the growth of ulcers resumes every two weeks. The wounds bleed and penetrate deeper into the tissues of the mouth.
- When healing, erosions leave deep scars.
Diet for stomatitis
Proper nutrition plays a vital role in the treatment of diseases, incl. and stomatitis. First of all, it is important to avoid dishes and foods that irritate the mucous membrane - hot, salty, with a lot of spices. You will also have to give up dry food, coarse and hard products, because... they will increase pain. Avoid foods and drinks with a lot of acids (apples, tomatoes, oranges, sour berries, coffee, sour juices) - they not only irritate the inflamed mucous membrane, but also create a favorable environment for the development of pathogens.
With stomatitis, it is difficult to chew food due to pain, so the main part of the diet should be boiled, stewed foods, preferably crushed into a puree. It is better to use meat and fish in the form of minced meat for cooking; replace broth soups with pieces of vegetables and meat with cream soup or puree soup. It is advisable to eat food warm.
Be sure to include vitamins A, B, and C in your diet, either in natural foods or in supplement form. It is recommended to consume soft foods - soft cheeses and cottage cheese, milk and kefir, viscous and semi-liquid porridges. Baby food (purees, curds, yoghurts, puddings, jellies) is well suited. It is better to replace drinks with tea, herbal infusions and clean water.
How to treat herpetic stomatitis?
Herpetic stomatitis
The form develops against the background of cold complications, gingivitis and other inflammatory processes in the body. The symptom is the appearance of multiple small rashes on the tongue, gums and inner surface of the cheeks. The pain, as a rule, is much stronger than from aphthous ulcers, but it is not the discomfort itself that is scary, but the consequences - fever and weakness.
Herpes lesions are primarily treated with a course of medications:
- Acyclovir - from 1 to 3 tablets per day.
- Viferon-gel - topically, twice a day, and only after the approval of the attending physician.
- Solcoseryl - temporary pain relief, 15 minutes before and immediately after meals.
- Rinsing with soda creates an additional alkaline environment in the mouth against bacteria.
Is treatment possible at home?
Treating stomatitis at home is quite possible, especially if it is not severe. However, it is still necessary to consult a doctor for an accurate diagnosis and choice of medications than to treat stomatitis at home.
To treat herpetic stomatitis at home, local remedies are sufficient: rinsing with miramistin (3-4 times a day) or hexoral. To suppress inflammation, you can use Cholisal gel, for faster healing of ulcers - solcoseryl gel (or Actovegin), sea buckthorn or rosehip oil, oil solutions of vitamins A or E. If rashes appear on the lips or skin around the mouth, you can use Zovirax cream or acyclovir. In severe cases of the disease, it is necessary to use drugs against the herpes virus, but they must be prescribed by a doctor.
In general, it is dangerous to treat severe forms of stomatitis at home, especially such as Vincent’s ulcerative necrotizing stomatitis. To combat it, antibiotics will be required, which should be selected by the attending physician.
Literature
- Bazhanov N. N. Dentistry: Textbook, 6th ed., revised. and additional - M.: GEOTAR-MED, 2002. - P. 96-102 - ISBN 5-9231-0272-2.
- Bulkina N.V., Lomakina D.O., Meleshina O.V. Chronic recurrent aphthous stomatitis: features of the clinical course and complex treatment // Saratov Journal of Medical Scientific Research. - 2011. - T. 7. - No. 1 (appendix). — P. 281-282.
- Galizina O.A. Main aspects of the occurrence, clinical manifestations, treatment and prevention of chronic recurrent aphthous stomatitis. CLINICAL STUDIES // RUSSIAN DENTAL JOURNAL, No. 6, 2014. - pp. 39-42
- O.A. Zorina, N.B. Petrukhina, L.M. Kozlova. Treatment of aphthous stomatitis in adolescents // Pediatric pharmacology. 2014; 11(3). — P. 85–88.
- Lutskaya I.K. Ulcerative-necrotic stomatitis in adults and children: diagnosis, treatment and prevention // Modern dentistry. – 2018. – No. 2. – pp. 17–20.
- Belousova O.V., Belousov E.A., Dorokhova N.N. Application of pharmacoeconomic methods to optimize the procurement of drugs for the treatment of stomatitis in a pharmacy // Scientific result. Medicine and pharmacy. – T.3, No. 1, 2022. – P. 48-55.
- Mavrutenkov V.V. Viral stomatitis // Child's Health, No. 3 (63), 2015. - P. 63-68.
- K. G. Karakov Fungal, viral and traumatic stomatitis in the clinic of therapeutic dentistry // Textbook / 2013. – 100 s. /ISBN 978-5-89822-345-8
- Volkov E.A., Butova V.G., Pozdnyakova T.I., Dzugaeva I.I. Clinical recommendations (treatment protocol) for chronic recurrent aphthous stomatitis. // Russian Dental Journal, No. 5, 2014 p. 35-48/UDC 616.31-002.157.2-036.12-08
- Instructions for use of the drug HEXORAL® aerosol // Reg. number P N014010/01 // .
- Instructions for use of the drug HEXORAL® solution: , .
- Instructions for use of the drug HEXORAL® TABS // Reg. number LSR-002626/07 // .
- Instructions for use of the drug HEXORAL® TABS CLASSIC // Reg. number P N015976/01 // .
- Instructions for use of the drug HEXORAL® TABS EXTRA // Reg. number LSR-004122/09 // .
Prevention of stomatitis
Preventing a disease from occurring is much easier than treating it. Considering that the main risk factors for stomatitis most often are decreased immunity and poor oral hygiene, as well as bad habits, we can name the key points for preventing stomatitis:
- regular teeth cleaning and visits to the dental office,
- taking care of the immune system - avoiding stress, taking multivitamins, eating fruits and vegetables,
- getting rid of bad habits (primarily smoking),
- take care of your health and try to prevent the development of chronic diseases.
When visiting a dentist to install orthodontic structures, dentures, or crowns, you must carefully choose a clinic to avoid allergies or rubbing of the dentures.
Possible complications and prevention
Severe herpes sore throat can lead to the spread of infection throughout the body and damage to internal organs - so-called complications arise. The most common complication after suffering herpes sore throat is serous meningitis, or inflammation of the brain. The disease can lead to disturbances in the functioning of the heart and cause myocarditis, which is diagnosed by an electrocardiogram. Kidney diseases (pyelonephritis), liver, hemorrhagic conjunctivitis - this is just an incomplete list of complications with late diagnosis of the disease and delayed treatment. If you have the slightest suspicion of a disease, do not delay visiting a doctor!
To date, no vaccines have been developed to prevent herpangina disease. During an epidemic, if possible, do not take your child to kindergarten or school. Adults should try to avoid places with a lot of people and remember the rules of hygiene. Both children and adults need to strengthen their immune system in general, eat healthy and balanced, take vitamins and harden themselves.
If there is a sick person at home, it is necessary to ventilate the room frequently, and provide the sick person with individual dishes, linen and a towel.
Prevention
In the oral cavity of any person there is a conditionally pathogenic microflora, which can be activated when immunity decreases. For this reason, it is important to lead a healthy lifestyle, eat well, and treat illnesses.
Hygiene rules must be observed. Do not eat dirty vegetables, wash your hands before eating, and replace your toothbrushes regularly.
For persons predisposed to the disease, any trauma to the oral mucosa should be excluded. Do not eat scalding, hard foods or spicy seasonings. If a wound appears, you should immediately treat it with an antiseptic.
It is imperative to carry out timely treatment of dental and ENT diseases. Chronic diseases and advanced caries are sources of infection.
Reasons for development
Stomatitis often occurs in people with reduced immunity and impaired microflora. If these 2 conditions are observed simultaneously, then even opportunistic microorganisms can cause severe inflammatory processes. Many other factors also influence the development of the disease.
Inflammation of the oral mucosa can occur in the following cases:
- mechanical, chemical, thermal injuries - hot burn, injury from solid food, cheek bite, etc. leads to tissue damage, penetration and spread of infection;
- poor nutrition, lack of vitamins, especially C, group B, minerals - zinc, iron and others;
- failure to comply with hygiene rules, eating unwashed fresh berries, vegetables, fruits, dirty hands while eating;
- treatment with medications that reduce salivation, antibiotics that destroy beneficial microflora, and a number of other medications;
- Frequent brushing of teeth with a paste containing sodium lauryl sulfate leads to a decrease in saliva secretion and dry mucous membranes, which become more susceptible to aggressive substances;
- poor-quality prosthetics and dental treatment due to which the gums are constantly injured;
- smoking, drinking alcohol;
- dehydration with prolonged diarrhea, vomiting.
Stomatitis often occurs during pregnancy due to hormonal imbalance. At risk are patients with diseases of the heart, blood vessels, gastrointestinal tract, pathologies of the immune and endocrine systems, and those with helminthic infestation. In diabetes mellitus, the aphthous form is diagnosed. People who use hormone inhalers to relieve asthma attacks suffer from candidiasis.
To answer the question whether stomatitis is contagious or not, differential diagnosis is necessary. Bacteria, viruses, and Candida fungi can be transmitted from person to person. The most contagious is the viral form of the pathology. However, with good immunity, the infection will not necessarily develop. It is also important how stomatitis is transmitted. If this is direct contact, for example a kiss, then the risk of getting sick is higher.