Cheilitis is an isolated inflammatory process in the area of the mucous membrane, skin and red border of the lips. Outwardly it looks like swelling with redness and peeling of tissue. It can be an independent disease or a symptomatic manifestation of other pathologies. Sooner or later, almost every person encounters it, but at a young age the disease is noticeably milder, recurs less often and has no complications. In older people, due to a weakened immune system, periodic relapses of cheilitis can cause malignant tissue degeneration.
Causes
Cheilitis is a polymorphic and multifactorial disease that can be triggered by infections, physical and chemical environmental factors, as well as internal characteristics of the body. Among them:
- constant exposure to the open air - inflammation and peeling of the lips occurs when chapped by hot or cold air, excessive insolation;
- the presence of chronic diseases with skin manifestations of symptoms - various types of dermatitis, psoriasis, lupus erythematosus, lichen planus, syphilis, etc.;
- allergic reactions of the body - mainly with food allergies;
- tissue irritation from regular exposure to chemicals, including medications (for example, nasal drops);
- various neurological disorders, severe stressful situations, depression, constant anxiety;
- endocrine abnormalities - primarily hyperfunction of the thyroid gland, diabetes mellitus.
Symptoms and treatment of lip jams in adults and children
The popular name for angulite is zaeda.
The disease is characterized by the presence of cracks in the corners of the mouth, erosion and irritation. In some cases, slight bleeding may occur. Common causes of sticking at the corners of the mouth include infection, irritation, and damage to the skin at the corners of the lips. Angulitis is rare in children. Most often, the disease is diagnosed in adults. Predisposing factors:
- decreased general immunity;
- deficiency of B vitamins;
- the presence of a bacterial infection;
- habit of licking lips, malocclusion;
- hypothermia;
- long-term use of corticosteroid drugs;
- eating unwashed vegetables and fruits;
- presence of caries;
- chronic diseases (diabetes mellitus, anemia, HIV, liver disease).
Your pediatrician will tell you at your appointment what causes seizures in babies.
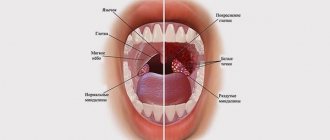
Types of cheilitis
Manifestations of cheilitis may vary depending on the type and cause of the disease. There are:
- Exfoliative cheilitis - manifested by peeling of the red border of the lips, with rare areas of burning and dryness of the lips themselves.
- Exudative cheilitis - symptoms of the disease are supplemented by swelling and severe pain. The skin in inflamed areas may become covered with baked crusts, which greatly complicate the patient’s life.
- The glandular form affects the minor salivary glands. Their congenital or acquired proliferation is observed, followed by infection with bacteria. In this case, the source of infection can be caries, periodontitis or banal plaque. Outwardly it manifests itself as the formation of cracks on the surface of the lips, which begin to become wet over time.
- The allergic form occurs under the influence of household, cosmetic or food irritants (often this is lipstick). There are characteristic manifestations of allergic cheilitis in musicians who play wind instruments and in those who like to chew pencils. This type of inflammation is characterized by severe swelling, often with the formation of blisters, as well as itching, severe redness and burning.
- Meteorological cheilitis develops under the influence of weather conditions (wind, sun) and is manifested by burning, itching with small weeping blisters, in place of which erosions and ulcers form over time.
- The atopic form manifests itself as a symptom of dermatitis or neurodermatitis. Manifests itself in the form of redness and ulcers in the corners of the lips.
- The hypovitaminosis type of the disease is formed in response to a severe lack of vitamins, mainly vitamins A, C, B2. A characteristic burning sensation affects the surface of the lips, mouth and tongue. The mucous tissues take on a swollen appearance, cracks on the lips peel and bleed.
- Macrocheilitis is a response to damage to adjacent nerves (facial nerve neuritis), while itching and swelling from the tongue can spread to other parts of the face.
Attention! With a long course, there is a high probability of inflammation degenerating into a malignant neoplasm. This is especially typical for the meteorological form, which, in the absence of proper treatment, is often complicated by precancerous diseases.
How to care for your lips?
- If cracks form, be sure to keep the wounds clean and do not let your child touch them with his hands or chew his lips. If an infection gets into such a crack, it can fester.
- For older children who will not lick the medicine from their lips, use healing creams and ointments.
- You can compensate for the lack of vitamins both with the help of tablets and with topical application. Many vitamins are available in the form of capsules, the contents of which are used to treat damaged areas.
- Monitor the child's emotional state. Perhaps constantly chapped lips are an indicator of increased stress, fears and stress.
- Pay attention to how much fluid your child drinks. The best alternative to juices and tea is clean drinking water. To avoid irritating your lips again, you can drink through a straw. Especially to avoid contact with hot food and drinks.
- And, of course, you can’t do without using hygienic lipsticks and lip balms. You can also apply baby cream, olive, castor and sea buckthorn oils to your lips.
La-Cri products are designed specifically to help the little ones. They are based on natural hypoallergenic components and do not use dyes or fragrances.
Lip balm provides daily care, softens and heals lips. And the cream can be used for enhanced healing and regeneration in severe cracks. La-Cri cosmetics are suitable for children from 0 months and will be safe even if the baby licks it from his lips.
Diagnosis of cheilitis
There are no specific laboratory tests to detect cheilitis. All diagnosis of the disease is carried out by visual examination. To determine the causes of inflammation, diagnostics of the gastrointestinal tract may be prescribed for the presence of Crohn's disease or ulcerative colitis. Additionally, allergy tests are performed to exclude food allergies.
General laboratory tests allow you to check the condition of the body and determine the possible causes of cheilitis:
- low levels of vitamins due to hypovitaminosis can provoke exfoliative cheilitis;
- bacterial cultures of smears and biopsies are performed in patients with immune system disorders in the absence of results from the treatment;
- testing for markers of HIV infection, herpes, the presence of fungal or bacterial microflora, respectively, allows us to identify the viral, bacterial or fungal causative agent of cheilitis;
- a blood test for anemia, ESR are required to assess general health;
- examination of the function of the thyroid and pancreas for endocrine pathologies.
On a note! Cheilitis tends to be chronic with periodic relapses. Self-healing without medical supervision is almost impossible, so try to pay attention to such a “minor” problem and consult a specialist. Diagnosis of the disease is carried out by a general practitioner or attending dentist. In some cases, consultation with an allergist, infectious diseases specialist, dermatovenerologist or gastroenterologist may be required.
Manifestations of atopic dermatitis
Skin symptoms and location of lesions vary in children of different ages. Common symptoms are the appearance of red, dry, itchy patches on the skin that occur as a result of inflammation. There is always itching - from mild to unbearable, disrupting sleep and appetite. Frequent scratching may cause scratches (scratching), oozing (separation of serous exudate through tiny defects in the epidermis), crusting, or erosion due to secondary infection. Sometimes, if atopic skin lesions, lesions from chronic pruritus and secondary infections last for many weeks, areas of skin atrophy (scars, hypopigmentation/hyperpigmentation, thinning or thickening of the skin) may develop.
In infants, atopic dermatitis usually affects the face, scalp, arms and legs. In older children, as a rule, only the elbows, popliteal fossae and wrists are affected. In some children with severe disease, the entire body may be affected. Eczema causes severe itching, which can in turn lead to a number of secondary problems: sleep disturbances, weight loss, depression (in the child or in the adult who cares for him), etc.
Symptoms usually worsen in the autumn-winter period (this fact is usually associated with the inclusion of central heating and more severe external climatic conditions) and improve in the spring-summer period, as well as in seaside resorts (this is usually associated with the abundance of ultraviolet radiation and milder climatic influences on affected skin). Typically, the most severe course of the disease is observed in children aged 6–18 months (in winter, exacerbations are more frequent and severe, in summer - less frequent and milder), then from year to year, exacerbations become less frequent and milder. By school, most children recover or have symptoms that do not reduce their quality of life.
Treatment
Different forms of cheilitis differ in their approach to treatment. Collectively, the impact may include:
- correction of the psycho-emotional sphere - a neurologist prescribes sedatives, tranquilizers, a psychologist or psychotherapist conducts appropriate psychotherapy;
- physiotherapy - treatment with laser, ultrasound, magnetotherapy, electrophoresis is prescribed locally; they relieve irritation and accelerate tissue regeneration;
- drug symptomatic therapy - non-hormonal anti-inflammatory drugs are prescribed; in case of severe inflammation - hormonal drugs;
- immunotherapy – strengthen the immune system by taking immunomodulators and immunostimulants;
- vitamin therapy - taking vitamins A, C, group B (mainly vitamin B2) is of great importance;
- surgical treatment – typical for glandular cheilitis with enlargement of the salivary glands; Both laser ablation with a surgical laser and direct removal of areas of the gland are used;
- antiallergic therapy with antihistamines.
Additionally, the doctor may prescribe diet therapy with the exclusion of foods that provoke allergies or chemical irritation of tissues (spicy foods, saltiness and marinades). When staying outdoors for a long time, it is imperative to use special protective equipment.
What to do if a child has diathesis
Local therapy using ointments is one of the components of complex treatment. But both hormonal and non-hormonal drugs should be prescribed by a doctor individually for each baby, taking into account the characteristics of the diathesis.
Self-medication in such a situation is not only ineffective, but also dangerous for the child’s health. Therefore, it is better to contact competent specialists. PsorMak employs doctors with extensive experience in treating diathesis.
We take a comprehensive approach to diagnosis and treatment, and for local therapy we use ointment made according to our own recipe without the addition of hormones.
She has been helping our patients at our clinic for more than 25 years, so we guarantee a complete cure without side effects. Contact us for a consultation so we can begin solving your problem. April 5, 2020
Author of the article: dermatologist Mak Vladimir Fedorovich
Prevention
The main prevention of cheilitis is maintaining a healthy lifestyle and timely treatment of any infectious and allergic diseases. Basic list of measures:
- Eat right - a balanced menu should contain an abundance of fruits, vegetables, herbs, nuts, fish, and high-quality dairy products.
- Reduce the use of cosmetics - try to choose hypoallergenic formulations and constantly monitor the skin's reaction.
- Dose your exposure to open wind or direct sunlight.
- Protect your lip skin from physical and chemical damage.
- Take vitamin and mineral complexes periodically in courses (after consultation with your doctor).
- Give up bad habits.
- Seek medical advice promptly if you have characteristic symptoms.
Remember: your health is the greatest value, and constant monitoring of its condition is very important to maintain the body’s performance, especially in old age.