One of the most common diseases associated with damage to the mucous membrane in the human oral cavity is stomatitis, which occurs in approximately a quarter of the entire world population. Children are most susceptible to the disease, the development of stomatitis in the mouth is accompanied by severe symptoms and requires immediate medical attention. But even among adults, stomatitis is not such a rare occurrence.
Therefore, even if you have never encountered the formation of painful ulcers on the palate, mucous membrane, throat or tongue, it will still be useful for you to know what stomatitis is, how it manifests itself, and most importantly, how such a disease is treated with medications . Dentistry "LeaderStom" will tell you about this, as well as how to prevent the occurrence and development of the disease through preventive measures for the hygiene of the human oral mucosa.
Stomatitis: what kind of disease is it, the mechanism of appearance of stomatitis ulcers
Scientists have not yet fully studied the mechanism by which stomatitis occurs on the mucous membrane in a person’s mouth. The manifestation of symptoms of the disease is associated with the specific reaction of a person’s immune system, which he exhibits in relation to irritants present on the mucous membrane of the mouth.
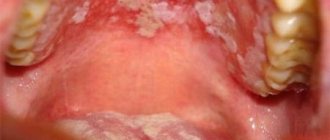
Bacteria, fungi, viruses and other microorganisms act as irritants. Normally, they are always present on human mucous membranes in one quantity or another. But when a person’s immunity is weakened, or other reasons provoke an increase in the number of microorganisms and the development of infectious diseases in the mouth (staphylococcal, streptococcal, candidal, etc.), this fact can trigger a stomatitis reaction.
Ulcers on the human mucosa, which are stomatitis in nature, are formed as a result of the fact that lymphocytes (white blood cells of the human immune system) begin to attack molecules that they cannot recognize. This reaction of the body is similar to that which occurs in the case of organ transplantation. As a result of such a lymphatic attack, stomatitis ulcers are formed on the oral mucosa, which usually go away on their own in one to two weeks without scarring.
Types of stomatitis, causes and symptoms of the disease
Based on the peculiarities of the mechanism of occurrence, stomatitis manifests itself not only as a separate disease, but also as a concomitant sign of the presence of infection in the human body. Depending on what mechanisms provoked the appearance of stomatitis ulcers in the mouth of a child or an adult, various types of stomatitis disease are distinguished.
Types of stomatitis:
- Aphthous stomatitis.
This is a common form of the disease that occurs in humans at any age. It appears in the form of yellow-gray ulcers (ulcers) surrounded by a red halo. Oral ulcers occur in groups or singly; they hurt and cause discomfort to a person. - Herpetic form of the disease.
This stomatitis reaction develops against the background of a herpetic infection in the human body. Herpetic stomatitis appears in the form of painful small blisters on the oral mucosa, which are located in groups. Such bubbles burst after 3-4 days. The herpetic form of the disease in both children and adults is accompanied by fever, gingivitis develops on the mucous membrane in the mouth, and a person’s saliva becomes viscous. To treat the disease, the doctor usually prescribes the drug acyclovir to the patient. - Vesicular stomatitis.
In this case, a person with such a disease is contagious, since the causative agent of the disease is an RNA virus. In order to avoid infection, the patient’s personal belongings should be disinfected and separate utensils and personal hygiene products should be provided. - Allergic stomatitis reaction.
The disease occurs due to allergens entering the human body, to which it reacts by forming stomatitis ulcers. Allergic substances enter our body with food or drinks. Foods such as citrus fruits, red berries (strawberries, raspberries), tomatoes, peanuts, chocolate or cereals (since they contain gluten) can provoke an allergic reaction, the development of stomatitis and the formation of ulcers on the mucous membranes of a person’s mouth. - Traumatic stomatitis.
The occurrence of the disease is associated with injuries to the mucous membranes in the human mouth. They appear when a person eats rough food or drinks hot drinks. In addition, an adult or child can simply bite their tongue or scratch an area of the oral mucosa, and this will provoke a stomatitis disease. - Catarrhal stomatitis.
This form of the disease develops if a person does not follow the rules of oral hygiene: neglects daily brushing of teeth, rinsing, and flossing.
Only a doctor can diagnose one or another form of stomatitis disease in an adult or child. Do not try to do this yourself at home, studying photos from the Internet, and prescribe treatment for yourself. Each case is individual, so if you suspect stomatitis in the mouth, you should seek advice from a dentist or therapist. Competent doctors from the LeaderStom network of dental clinics will help you cope with the disease and cure wounds on the oral mucosa, palate, throat and tongue.
What is white plaque on the wound after tooth extraction?
A few hours after the tooth is removed, a dark clot appears in the socket - bluish, black, red or brown. This clot is blood, and it is the primary protection of the socket from bacteria or pieces of food entering it. On the 2nd - 4th day, the patient may see that a coating appears on the clot - yellowish, gray or white. The deposit looks like pus and, together with the resulting bad breath, can alert the patient. However, there is no need to be alarmed - this plaque is not a sign of wound decay and indicates a normal healing process. This special protein compound is fibrin.
A milky plaque (fibrinous) can be very dense, hard or soft. This is no cause for concern. If you come to the dentist with this question for an unscheduled appointment, the specialist will tell you that everything is in order and there is no need to remove the film.
If the film is not removed and the wound is not disturbed, active processes will occur underneath it:
- the blood clot will begin to dissolve;
- the hole will begin to decrease in size;
- young cells, osteoblasts, will begin to move from the edge of the wound to the center;
- The gums will begin to close the wound.
Fibrinous plaque after tooth extraction is a natural stage of gradual recovery of the body, in which it is better not to interfere.
Stomatitis in a child: symptoms, causes
The description of stomatitis in a child deserves special attention. The specificity of stomatitis that occurs in the mouth of a young child is that the disease is a consequence of a weakened or not fully formed immune system. Therefore, the stomatitis reaction manifests itself clearly and the course of the disease is accompanied by severe symptoms.
Symptoms of stomatitis in a child:
- The oral mucosa turns red and swelling appears.
- Characteristic stomatitis ulcers form in the mouth, which are located either singly or in groups. The localization of ulcerative formations during stomatitis in a child is different: wounds and blisters appear on the tongue, on the palate, mucous membrane or in the throat. The nature of the lesions depends on the form of the disease and on what factors triggered the reaction (infections, allergies, vitamin deficiency, etc.).
- The development of stomatitis in the baby’s oral cavity is accompanied by an increase in the child’s body temperature (up to 38-39 degrees).
- The baby’s submandibular lymph nodes increase in volume and become painful on palpation.
- The child becomes lethargic, drowsy, capricious and whiny.
The baby has a hard time suffering from stomatitis in the mouth, and this is a lot of stress for the young body, not to mention the fact that the disease worsens the child’s appetite and disrupts the child’s sleep pattern. Therefore, if you notice the formation of ulcers in the mouth of your daughter or son or identify other symptoms of stomatitis, immediately show your child to a doctor (dentist or therapist).
Studying pictures and photographs of other children with oral stomatitis on the Internet is pointless; you will only waste your time and may come to the wrong conclusions. The doctor will help you understand the reasons that provoked the development of stomatitis in the child’s mouth and prescribe effective treatment for stomatitis.
Why you don’t need to remove white plaque after tooth extraction
In some cases, patients intentionally or accidentally remove a blood clot or fibrinous film from the socket. This is not necessary, since removing a clot or film can provoke negative processes.
First of all, an open wound provides access for bacteria to the circulatory system and tissues of the maxillofacial apparatus. Infection can cause serious consequences and require long-term treatment with antibiotics. Also, removing the clot and white plaque increases the pain, since an open wound is more sensitive to any irritants, including drinking drinks and food, during a conversation.
Finally, plaque on the gums after tooth extraction does not need to be cleaned off because this can cause re-bleeding and prolong the wound healing stage.
In any case, there is no need to intentionally remove plaque; this can cause:
- serious complications;
- severe pain;
- improper gum formation;
- long recovery process after tooth extraction.
To avoid accidentally damaging the socket, blood clot or fibrinous film, you must follow the recommendations given by the doctor after the operation.
Which people are at risk for stomatitis?
As already noted, children are primarily susceptible to stomatitis, since their immune system is just learning to fight infections and diseases and respond to irritants appropriately. Therefore, if, with timely consultation with a doctor and proper treatment, your baby still chronically develops stomatitis in the mouth, then perhaps the reason is due to age, and over time these problems will disappear.
But besides age, there are other factors that increase the risk of stomatitis ulcers in a person’s mouth. They are associated with various reasons, some of which we have already named when characterizing the types of stomatitis, but now we will try to specify each factor separately.
Those at risk for possible development of stomatitis include:
- People with a hereditary predisposition to the disease. Scientists have proven that the likelihood that stomatitis will develop in a person’s mouth (on the palate, mucous membrane, throat or tongue) increases if one or both parents have ever encountered similar problems. The best way out in this situation is to follow the rules of oral hygiene and take vitamin and immunomodulatory complexes as prescribed by your doctor.
- People with current somatic diseases. Quite often situations arise when stomatitis chronically develops in a person’s mouth without any obvious reason. During a complete examination of the body of such a person, any diseases are usually revealed, in particular, diseases of the gastrointestinal tract (giardiasis or helminthic infestations). Parasites, while in the body, may not manifest themselves in any way and not bother a person for years, but they reduce his immunity and prevent resistance to infections and other diseases. In this case, in order to get rid of stomatitis in the oral cavity, a person should undergo a course of treatment that will allow him to get rid of other concomitant diseases.
- People with reduced immunity. Human immunity is reduced not only by somatic diseases, but also, for example, by factors such as stress. Therefore, if you have a hard job or tense family relationships, this can cause chronic stomatitis, localized on the oral mucosa. In addition, frequent occurrence of ulcers in a person's mouth may indicate more serious problems with the immune system caused by a disease such as AIDS. Therefore, in this situation, a person is recommended to get tested, undergo a full examination of the body and get plenty of rest.
- People with bad habits. Bad habits such as alcohol, smoking and drug use can cause stomatitis and the formation of painful ulcers in the mouth. The fact is that such a lifestyle weakens the immune system and undermines human health. In addition, cigarette smoke and alcohol create favorable conditions in the oral cavity for the development of bacteria, viruses and fungal infections, which provoke the appearance of stomatitis ulcers on the human mucosa.
If you have seen photographs of people with stomatitis in the mouth, then you have probably noticed how unattractive this disease looks, not to mention how much discomfort it causes to a person. Therefore, if you are at risk for the possibility of developing stomatitis ulcers on the mucous membrane, palate, throat or tongue, then you should take measures to reduce the chances of getting stomatitis: quit bad habits, undergo a course of treatment for somatic diseases, increase your immunity and take vitamin complexes. But these measures should be taken only after consulting a doctor.
Treatment methods for stomatitis
Local treatment of stomatitis involves treating ulcers on the palate, tongue, or other areas of the oral mucosa with antiseptic agents. If stomatitis ulcers appear in the throat, the patient is prescribed gargling with an antiseptic solution or medicinal herbs.
General therapy for the disease includes drugs that are aimed at eliminating the causes of stomatitis in the mouth: antibiotics (for a bacterial infection), antiviral drugs (for example, acyclovir for herpetic stomatitis in the mouth), antifungals (if the cause of stomatitis is a fungus of the genus Candida or what -other), antihistamines (for allergic stomatitis or to relieve swelling during the inflammatory process), etc.
For prevention, increasing the defenses of the human body and in order to prevent complications and the development of chronic stomatitis, the patient is prescribed immunomodulatory agents and vitamin complexes. To relieve pain and reduce fever during stomatitis, doctors use painkillers.
The closure and disappearance of stomatitis ulcers with appropriate treatment of stomatitis disease and inflammation that occurs in the human mucosa usually occurs within 1-2 weeks, but you should take medications prescribed by your doctor strictly within the course. The fact that you felt better and stopped experiencing pain and discomfort due to stomatitis in the mouth does not yet indicate that the disease has been cured.
Strictly follow all the doctor’s recommendations and do not try to cure stomatitis yourself, using the advice of friends or photographs and recipes for preparing medicinal potions found on the Internet. At best, you simply will not achieve the desired effect, and at worst, you will increase the symptoms of the disease.
Gum healing
After tooth extraction, you need to be prepared for the fact that pain and swelling may intensify on the second day after surgery. But already on the 3rd - 4th day after the operation, the discomfort will begin to decrease. By this time, the wound healing processes are more active, and by touching the tip of the tongue to the hole, you can feel that a compaction has formed.
During this period, the following are actively developing:
- bone formation in the area of the removed tooth root;
- narrowing of the socket due to the “growth” of the gums;
- formation of the mucous membrane in the socket area.
Fibrinous plaque after tooth extraction persists for a week. It disappears on its own, without mechanical cleaning. Little by little, the mucous membrane begins to turn pink, gradually acquiring a healthy, natural color. Around the 10th day, wound healing is completed: healthy tissue is formed that covers the mouth of the hole. A small depression remains in the area of the removed tooth. The formation of bone tissue at the site of tooth extraction takes much longer - up to 6 months. Changes will be visible on an x-ray.
Acute and chronic stomatitis, what is the difference?
There are two forms of stomatitis disease: acute and chronic. For the first time, stomatitis usually manifests itself in an acute form, characterized by the sudden appearance of ulcers on the palate, mucous membranes in the mouth, tongue or throat of a person. The ulcers hurt and cause discomfort when talking or eating.
Acute stomatitis goes away on its own after 7-10 days, even if it is not treated, but in most cases the disease returns in a chronic form. This means that a person develops stomatitis ulcers in the oral cavity from time to time throughout his life. In order to prevent the transition of stomatitis disease from an acute to a chronic form, a person should undergo a course of treatment for the disease at the initial stage. It is very important that a plan and methodology for combating stomatitis in the patient’s mouth is developed by a competent and competent doctor who could take into account all the factors that could provoke this disease and get rid of them.
The LeaderStom clinic invites you to diagnose stomatitis and undergo a course of effective treatment under the supervision of the institution’s experienced dentists. Our doctors know modern methods of combating this disease in patients of different ages and are able not only to solve the existing problem, but also to give valuable recommendations for further oral care in order to prevent the occurrence of stomatitis ulcers on the mucous membrane, palate, throat or tongue of a person again .