Young people often don’t think about whether stomatitis is transmitted through kissing, and carefreely kiss their other halves. At the same time, they do not take any measures for treatment, considering this disease to be trivial. Is stomatitis so dangerous that you can’t contact other people?
Stomatitis is an inflammation of the oral mucosa, which in most cases is accompanied by the formation of ulcers. Along with this, swelling of the mucous membrane is observed, and a white or yellow-white coating forms. When communicating, a person feels discomfort, and pain occurs while eating. Increased salivation, gums often bleed, and bad breath appears.
What is stomatitis
Stomatitis (mucositis) is a disease that is accompanied by damage to soft tissues in the oral cavity.
It can be either an independent disease or a complication of various pathological processes, for example, measles, influenza, scarlet fever, etc. Until recently, stomatitis was considered a childhood disease. Today it is becoming more common in adults too. This trend raises questions about whether stomatitis is transmitted and, if so, how to protect yourself and your child. It all depends on the form of manifestation of the disease
Hepatitis A
This is an infectious disease that affects the liver. Hepatitis A in most cases ends in complete recovery. The disease does not become chronic. But the danger is that the disease is extremely contagious and a sick person can infect a huge number of people without even knowing that he is a carrier of the virus. The infection is most contagious in the last days of the incubation period, while there are no symptoms. In this case, infection can occur not only through a kiss, but even through objects touched by the patient.
Symptoms of stomatitis
Stomatitis can be recognized by the following signs:
- ulcers, wounds, erosions and rashes on tissues;
- red color of the mucous membrane;
- plaque on the tongue, inner surface of the cheeks, palate;
- unpleasant taste;
- swelling of tissues;
- heavy salivation;
- bad breath;
- itching and burning – in some cases;
- discomfort and pain;
- bleeding gums – occasionally;
- increased body temperature;
- lymphadenitis.
Symptoms in children are always more pronounced. The child often feels severe pain. Adults tolerate the disease easily. Its symptoms usually do not cause severe discomfort.
When the first symptoms appear, you should immediately consult a doctor to protect yourself and, possibly, others.
Mononucleosis
This disease is also caused by the herpes virus, but not the first type, but the fourth. This virus is also called the Epstein-Barr virus. The virus enters the body through saliva and begins to multiply in the mouth and throat. For this reason, it is very easy to become infected with mononucleosis through a kiss. This disease even has a third name - “kissing disease.” Symptoms of mononucleosis are high fever, sore throat, and swollen lymph nodes. Symptoms do not begin to appear immediately, but after a couple of weeks.
Types of disease
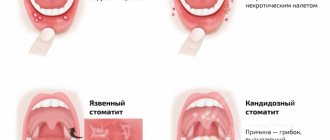
Stomatitis has different forms, depending on which the doctor determines whether it is contagious or not, and also prescribes appropriate treatment.
Allergic stomatitis
This is a common form of the disease that is difficult to treat. From the name it is clear that the cause of its development is an allergy, but it is necessary to find out what exactly it is. These could be medications, food, materials used for prosthetics. The disease is accompanied by the appearance of ulcers, which provoke pain.
Viral stomatitis
The most common type of viral stomatitis is herpetic stomatitis, the causative agent of which is the herpes virus. There are other forms that are provoked by adenovirus, enterovirus, etc. They are often found in children under 5–6 years of age, but are also common among older age groups. A feature of viral stomatitis is its erosive spread, when one ulcer appears next to another. Herpes mucositis may cause complications such as fever, nausea, vomiting and diarrhea.
This form of the disease is transmitted to others by contact and airborne droplets. If it is diagnosed, for example, in someone in kindergarten, then quarantine must be introduced. Infection occurs through dishes and toys, so the disease can quickly spread from child to child.
The virus spreads from nursing mothers to children if hygiene rules are violated. Adults become infected even through handshakes. Sneezing also causes the disease to develop.
Aphthous stomatitis
This form is common among adults. It develops against the background of a weakening of the body’s immune forces, so aphthous stomatitis is a common occurrence in spring and autumn. With this type of disease, characteristic aphthae appear - small ulcers. They can be single or group. Aphthous mucositis is not spread from person to person.
Fungal stomatitis
The disease manifests itself in children and adults, mainly in infants and women. It is provoked by fungi of the genus Candida, which are activated in the oral cavity when the immune system is weakened. The cause of fungal stomatitis can be long-term use of antibiotics. In addition to ulcers, its characteristic feature is a cheesy coating on the tongue, palate and inner surface of the cheeks.
Bacterial stomatitis
This type of disease is diagnosed when the oral cavity is affected by microorganisms, most often streptococci, staphylococci. The manifestation of bacterial stomatitis is provoked by tuberculosis, as well as sexually transmitted diseases, for example, gonorrhea, syphilis. More often, children whose immunity is not strong enough suffer from it. But everyone must be careful. The disease is transmitted from children to adults through dishes, toys, and damage to the mucous membrane.
This form is characterized by swelling in the oral cavity, redness of the mucous membrane and hardening of the palate, as well as an unpleasant odor, ulceration and cracks. Symptoms of intoxication may appear: vomiting, weakness, rapid pulse.
Other forms of stomatitis
In addition to the above types of disease, the following can also be distinguished:
- chemical stomatitis - occurs as a result of burns to the oral cavity with alkaline substances or acid;
- traumatic - ulcers are formed as a result of impact and disruption of tissue integrity;
- radiation – develops as a result of radiation.
Such forms are non-contagious and therefore do not pose a danger to other people.
Stomatitis: causes
A variety of factors and diseases contribute to the development of stomatitis in adults. For ease of diagnosis, doctors combined the causes of stomatitis into four groups, highlighting the main problem conditions:
- Mechanical injury. Ulcers appear as a result of some irritating factor. Damage can be caused by eating hard foods, poorly installed dentures, tartar buildup, and sharp edges of chipped crowns. Pathogenic microflora enters the damaged area, causing inflammation and active formation of ulcers.
- Chemical or thermal burn. Aggressive chemical agents can be food (citrus fruits), medications, nicotine, incorrectly selected toothpastes or mouth rinses. Thermal burn occurs when consuming excessively hot food or drinks.
- Poor oral hygiene. Failure to comply with regular hygiene procedures, tartar, and plaque provoke the active proliferation of bacterial microflora, which leads to inflammation of the oral mucosa.
- Chronic diseases. In adults, stomatitis develops as a reaction to problems of the gastrointestinal tract, cardiovascular system, due to anemia, endocrine pathologies, and HIV infections.
In addition to the listed categories, the causes of stomatitis can also be internal problems:
- vitamin deficiency, micronutrient deficiency - unbalanced diet, metabolic disorders in the body;
- allergies - of any origin;
- heredity - the individual reaction of the immune system to deteriorating health;
- a general decline in immunity - as a result of serious illnesses.
Unfavorable factors become catalysts for the development of pathology, and external circumstances aggravate the course of the disease.
The variety of causes points to an important point: there is no obvious causative agent of stomatitis. In order for an ulcer to localize, several circumstances must coincide - decreased immunity for any reason, an abundance of pathogenic microflora in the oral cavity, a traumatic agent.
Ways of transmission of stomatitis
Let's summarize. Viral, bacterial and herpetic forms of stomatitis are contagious. Knowing how the disease is transmitted, you can protect yourself and your loved ones. Ways of transmission of infection:
- airborne - sneezing, coughing;
- household items - common dishes, linen, personal items;
- toys, raw pacifiers, rattles;
- dirty hands;
- unwashed food;
- biological fluids - through saliva, blood, breast milk;
- Pets can carry the virus.
It is possible to catch the infection anywhere – from the street to your own home. You can get infected from both a child and an adult.
Cytomegalovirus
This is another member of the herpes virus family. It is very common and in most cases is in an inactive state in the body. Its activation occurs when the immune system is weakened, as well as during stressful situations. The virus is contained in all biological fluids of the infected person, and therefore can easily be transmitted through saliva during a kiss. Cytomegalovirus is especially dangerous for pregnant women, since when infected with it, the child often dies in utero. Surviving children who were infected in utero subsequently develop various abnormalities.
Bacterial stomatitis
The bacterial form often occurs against the background of an underlying disease. Risk factors:
- Pharyngitis.
- Laryngitis.
- Rhinitis.
- Chronic tonsillitis.
- Angina.
When the immune system is significantly weakened, bacteria begin to multiply rapidly. Staphylococcus and streptococcus are common. Bacteria lead to the appearance of a purulent rash. The bubbles open, erosions and ulcers form.
Children transmit the disease to each other through household and contact routes. Toys and personal items become a breeding ground for pathogenic bacteria. One bath towel in a family for several members contributes to the fact that stomatitis will be detected immediately in a brother and sister or in a grandson and grandmother.
Transmission of bacterial stomatitis is not uncommon in children's groups. Adults become infected less frequently. For bacteria to get inside and begin their destructive activity, there must be damage to the skin or mucous membrane.
The slightest scratch may be enough if the body's defenses are reduced. But if an adult has a strong immune system, there is little chance of contracting bacterial stomatitis. The exception is representatives of the older age group. They experience an age-related decline in their defenses.
A kiss that tastes like “stomatitis”: is the disease contagious and how is it transmitted?
Stomatitis is a disease that is a lesion of the oral mucosa.
Often occurs as a result of an immune response to the appearance of molecules that are difficult to recognize by the body.
The appearance of such elements causes an attack on lymphocytes, forming ulcers. The body reacts in a similar way to a human organ transplant.
Stomatitis is transmitted through kissing or any other type of contact . The cause of the disease can be a simple lack of oral hygiene.
Ulcers heal within 7-14 days. People who have had stomatitis are susceptible to recurrent illness, however, with a fairly variable frequency. Sometimes the disease appears several times throughout the year, which indicates a chronic form of the disease.
Is stomatitis contagious?
The question of whether stomatitis is contagious should be considered at the level of the root cause of the outbreak of the disease.
Of course, there are contagious types - herpes and candidal stomatitis are especially dangerous. However, each disease is considered by specialists individually.
The following types of stomatitis exist:
- Viral. Generated by viruses caused by diseases such as chickenpox, herpes or influenza. Symptoms include pain in the oral cavity and fever. It manifests itself in the form of the appearance of purulent blisters, which, bursting, form wounds. This type of disease is contagious;
- Bacterial. It affects not only the mucous membrane, but also the gums, palate or sublingual area with the appearance of cracks and bad breath, as well as nausea, dizziness, increased heart rate and general weakness. In most cases, it poses a danger to newborns who do not have a sufficiently developed immune system due to their age. For adults, viral stomatitis is dangerous only through airborne droplets or in the case of sharing cutlery with a patient;
- It is known that about 20% of the population suffers from this disease, of which pregnant women predominate.
Transmission routes
As mentioned earlier, the routes of transmission of stomatitis can be completely different - from airborne droplets to traumatic.
Children often suffer from stomatitis due to poorly developed immunity, which is not yet able to fully cope with surrounding viruses.
Is stomatitis transmitted through kissing?
Prolonged contact with a sick person can also lead to infection with stomatitis.Constant exposure of the oral mucosa to foreign pathogenic microorganisms causes a decrease in the immune system and a reduction in the protective mechanisms of the oral cavity itself.
That is why the transmission of stomatitis through kissing is quite common.
How to protect yourself?
In order to protect yourself from stomatitis, first of all, you must adhere to the rules of hygiene of the gums and teeth.One of the main protective measures is strengthening the immune system through a healthy diet.
Often stomatitis can be caused by a deficiency of B vitamins, zinc or iron in the body.
A preventive examination by a dentist and timely dental treatment are mandatory.
If the infection with stomatitis is permanent, then it is necessary that all family members living with the patient be examined by a doctor.
The cause of frequent stomatitis may unexpectedly be someone from your close circle, without even knowing it.
How to treat stomatitis
For any form of stomatitis, treatment begin with a visit to the doctor's office. The dentist must determine the form and severity of the disease in order to prescribe appropriate therapy. Self-medication may not bring results and thus aggravate the situation, allowing the disease to progress to a more severe stage.
The diagnosis of “stomatitis” is made by the doctor after an examination, and after that he can prescribe the patient to take an oral smear to find out the exact cause of the disease. PCR analysis of the biomaterial will show the presence or absence of a pathogen, for example a Candida fungus or a herpes virus. If the cause is not the pathogen, an additional visit to another doctor may be required. Thus, if allergic stomatitis is suspected, the patient will be referred to an allergist, and if immunity or metabolic disorders are suspected, the patient will be referred to an immunologist or gastroenterologist.
In addition to establishing the cause of the disease, the patient receives recommendations on how to treat stomatitis in his case , including:
- ✔️ Bringing oral hygiene back to normal and further supporting it;
- ✔️ Treatment of ulcers with special means, depending on the diagnosis - antiseptic, antiviral or antifungal;
- ✔️ Pain relief with anesthetics;
- ✔️ Use of products that eliminate inflammation and swelling;
- ✔️ Following a diet to restore the mucous membrane.
Although stomatitis is treated with drugs , the patient needs to adhere to a diet so that food does not cause mechanical damage to the already inflamed mucosa. You will have to exclude hard, sour, spicy and overly salty foods from your diet. The menu will be similar to what is prescribed for gastrointestinal diseases: boiled products crushed to a puree state, liquid porridges and broths, fermented milk products. Everything is warm temperature, nothing hot or cold. Even soft bread will have to be removed, as it can scratch irritated areas in the mouth. For children, the doctor gives recommendations depending on their age.
The likelihood of contracting aphthous stomatitis
People with serious chronic diseases are susceptible to aphthous stomatitis. Most often these are diseases:
- Oral cavity.
- Throat.
- Upper respiratory tract.
The presence of a focus of infection weakens local immunity. The consequence is the appearance of blisters, ulcers, and plaque. A yellow-white coating is characteristic. Erosive changes become pronounced if left untreated.
The disease may not cause concern for a long time. In any disease, with exacerbation of chronic diseases, the eroded surfaces become painful.
The risk of developing aphthous stomatitis increases:
- Poor nutrition .
- The presence of long-term non-healing wounds in the mouth.
- Presence of untreated teeth.
- Gum diseases .
- Incorrectly fitted dentures .
- Oral injuries
Diet for stomatitis
Stomatitis often worries children, becoming a consequence of insufficient immune forces of the body, weakened by some disease.
Aphthous stomatitis is typical for those suffering from diabetes.
Aphthous stomatitis itself is not contagious. Communication with a person who has signs of the disease is not dangerous. The risk of infection arises when a patient with aphthous stomatitis “adds” a viral infection to the underlying disease.
Redness of the throat may indicate pharyngitis, purulent discharge from the tonsils may indicate tonsillitis. In these cases, the pathogen is transmitted to a healthy person through contact with a sick person.
Is it possible to get stomatitis through a kiss?
Young people often don’t think about whether stomatitis is transmitted through kissing, and carefreely kiss their other halves. At the same time, they do not take any measures for treatment, considering this disease to be trivial. Is stomatitis so dangerous that you can’t contact other people?
Stomatitis is an inflammation of the oral mucosa, which in most cases is accompanied by the formation of ulcers. Along with this, swelling of the mucous membrane is observed, and a white or yellow-white coating forms. When communicating, a person feels discomfort, and pain occurs while eating. Increased salivation, gums often bleed, and bad breath appears.
Infection with stomatitis through kissing
The symptoms of the disease are quite different, as are the pathogens. Despite the seemingly complete study of stomatitis, scientists to this day do not know the exact method of its appearance; one version is inclined to believe that stomatitis is a reaction of the immune system to irritating substances unfamiliar to the body that have entered the oral cavity. As a result, the body sends lymphocytes to fight them, and so ulcers are obtained, which clearly indicate the presence of the disease.
In addition, a fungal infection in the mouth can also play the role of a pathogen. In such a situation, kissing is also best avoided.
If we are talking about herpes, it is very easy to catch it by using the patient’s dishes, so during the period of illness it is strongly recommended to maintain personal hygiene and scald the dishes with boiling water. Upon completion of treatment, you should change your toothbrush.
There is an excellent remedy against the herpes (aphthous) form of the disease. The use of acyclovir for stomatitis helps get rid of inflammation and pain.
What if stomatitis cannot infect a partner?
There are situations when kissing does not transmit stomatitis to a partner - for example, if the cause of stomatitis is a gastrointestinal disease, poor personal hygiene, or poor-quality fitting of dentures. But even in this case, it is better to refrain from kissing. After all, the altered microflora of the mouth during stomatitis creates a bad odor from the oral cavity, which is unlikely to please your partner . To eliminate the bad odor, you can use Metrogyl Denta. Plus, Metrogyl Denta helps with stomatitis.
You should first undergo a course of treatment, and then you can move on to kissing. As a rule, the illness does not last longer than 10 days if patients adhere to good personal hygiene and take medications responsibly for topical or internal use.