What is mandibular anesthesia
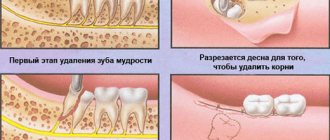
Dentistry today has a large selection of types of pain relief. This opens up wide opportunities for the dental surgeon, especially in terms of treating young patients. Mandibular anesthesia is a conduction-type local anesthesia. Provodnikova - temporary blocking of the transmission of nerve impulses through a large nerve trunk. It is used when there is a need for an absolute block of pain while keeping the patient fully conscious.
Mandibular anesthesia is required if surgical intervention on the lower jaw is planned. An unpleasant moment of injection is a short-term feeling of fullness, pain and burning in the injection area. This sensation lasts a few seconds and is comparable to a prick when blood is drawn from a vein.
Mandibular anesthesia by palpation
The target point is the mandibular foramen, through which the inferior alveolar nerve enters the canal, located on the inner surface of the ramus of the mandible. Location of the mandibular foramen .
The distance from the edges of the lower jaw: from the anterior edge of the lower jaw - 15 mm, from the posterior - 13 mm, from the semilunar notch - 22 mm and from the lower edge of the lower jaw - 27 mm (Fig. 93, A). Rice. 93. Lower jaw. A - lower jaw from the outside, slightly in front and above (V.P. Vorobyov, 1946): - articular process; 2— coronoid process; 3 - anterior edge of the lower jaw branch; 4 - mandibular eminence (torus); 5—temporal scallop; 6— retromolar fossa; 7 - mandibular foramen; 8 - tongue of the lower jaw; 9 - mental foramen. B - branch of the lower jaw: 1 - inferior alveolar nerve, 2 - internal pterygoid muscle.
The height of the hole in adults corresponds to the level of the chewing surface of the lower molars, in children and the elderly it is slightly lower. From below and in front, the mandibular foramen is covered by a bony protrusion (tongue of the lower jaw). In this regard, the anesthetic solution must be injected 7-10 mm above the level of the hole, where the nerve, before entering the mandibular canal, passes through a bone groove filled with loose fiber and in which the anesthetic spreads well. CONCLUSION : to approach the target point, the needle must be inserted 7-10 mm above the level of the chewing surface of the lower molars (Fig. 94, A).
Rice. 94. Needle position for mandibular anesthesia . (G.P. Ruzin, M.P. Burykh, 2000) A - on the mandibular bone. The needle passes 7-10 mm above the chewing surface of the lower molars, the end of the needle is located in the pterygo-maxillary space in the bone groove (sulcus n. mandibularis). 1 — level of the chewing surface of the lower molars; 2—tongue of the lower jaw; 3 - pterygomaxillary space. B - on a vertical section. B - on a horizontal section of the preparation.
Injection equipment (for all types of intraoral mandibular and torusal anesthesia): carpule or disposable plastic syringe 2 ml, needle 41.5-50 mm long.
Methods of mandibular anesthesia
There are two common methods of performing mandibular anesthesia. The first method is intraoral and is carried out according to the modification of Gou-Gates and Akinosi. The second method is extraoral, carried out in three ways - mandibular, retromaxillary or subzygomatic.
From a technical point of view, there are the apodactyl (without palpation) method, the finger method, as well as modifications of Go-Gates and Akinosi.
Mandibular anesthesia using the apodactyl technique is performed most often. In the area of the required tooth in the lower jaw, infiltration anesthesia is first performed to anesthetize the buccal space. Then, with the maximum opening of the mouth, the patient feels the line between the lower and middle third of the pterygomandibular fold in its lateral slope. This is the place where the needle is inserted. First, it is inserted all the way into the bone, then it is turned in the opposite direction and one milliliter is injected at the level of the incisors. A total of 2 to 2.5 ml of anesthetic is injected.
With the finger method, an injection of an anesthetic solution in an amount of 3-4 ml is carried out in the area of the retromolar space and temporal ridge. The anesthetic is administered, as with the apodactylic technique, in two stages with a change in the position of the needle.
The Go-Gates modification involves anesthesia of three branches of the mandibular nerve at once. For this purpose, an injection of an anesthetic solution is administered in the area of the condylar process of the mandible.
If the patient has limited ability to open his mouth, mandibular anesthesia is performed using the Akinosi method. The patient does not open his mouth and closes his teeth. The injection is placed at the border of the buccal mucosa and the retromolar region of the upper jaw.
To perform mandibular anesthesia, the doctor must be highly qualified and have deep anatomical knowledge of the structure of the lower jaw.
Medical Internet conferences
To motivate children for timely dental treatment, it is necessary that all interventions in the dental chair are minimally painful. This can only be achieved with high-quality anesthesia. In pediatric dental practice, of all types of anesthesia, infiltration, mandibular, torus and palatal anesthesia are most often used. In the lower jaw, mandibular anesthesia is often used, in which the inferior alveolar and lingual nerves are switched off. The area of anesthesia is: the mucous membrane and periosteum of the alveolar process on the lingual side on half of the jaw; anterior 2/3 halves of the tongue; half of the lower lip; all teeth on the corresponding half of the lower jaw: mucous membrane and periosteum on the vestibular side of the alveolar process, except for the area near the molars, which requires additional infiltration anesthesia, since this area is innervated by the buccal nerve. Fig.1.
Knowledge about the features of mandibular anesthesia is significant when planning measures to provide emergency care in emergency conditions and in the treatment of surgical pathology in children, therefore, during its implementation, you should know the following landmarks or features: the location of the bone tongue and the mandibular foramen on the medial surface of the lower branch jaws. There are anatomical differences in the size and proportions of the bones of the maxillofacial region in children, which must be taken into account when administering anesthesia.
In a 3-5 year old child, the mandibular tongue is located approximately at the level of the occlusal surface of the teeth; with age, the position of the tongue changes upward and posteriorly relative to the occlusal plane, and already in a 15-16 year old teenager it is located approximately 1 cm above it (as in an adult) , therefore, when carrying out anesthesia, the needle is injected not 1 cm above the chewing surface of the lower molars, as in adults, but at the level of the chewing surface of these teeth and the lower the younger the child.
The branch of the lower jaw in children 3-5 years old is twice as narrow as in an adult; the volume of the pterygomaxillary space in children is less than in adults, therefore the mandibular, lingual and buccal nerves are located closer to each other. The angle of the lower jaw in an infant is 140º-145º, due to which the mandibular foramen itself is located lower, being in the same plane with the chewing surface of the lower molars. With age, the angle of the lower jaw decreases due to the eruption of permanent teeth, including wisdom teeth. In preschool children, the needle penetrates soft tissue by 10-15 mm (in adults by 15-25 mm). Therefore, children are given pain relief with a short needle. For anesthesia of the inferior alveolar nerve, 0.5-1 ml is enough for children. anesthetic (adults 1.5-1.8 ml). In preschool age, using mandibular anesthesia, it is often possible to turn off the sensitivity of all three nerves (inferior alveolar, lingual, buccal) that innervate the teeth of the lower jaw, which makes it possible to use additional anesthesia of the buccal nerve less often.
In accordance with the growth of the jaws, the change in the location of the mandibular foramen has the following patterns: Fig. 2. In children 3-5 years old it is located 1-2 mm below the chewing surface of the teeth of the lower jaw, and in children over 6-8 years old - at the level of the chewing surface of these teeth, in children 9-11 years old - 3-5 mm higher level of the chewing surface of these teeth, 12 years and older - as in adults - 1 cm above the level of the chewing surface of these teeth.
Based on the above, it follows that mandibular anesthesia at different ages is carried out taking into account the anatomical features of the structure of the jaws, ignorance of which can lead to poor quality anesthesia and, consequently, to more painful necessary manipulations. As a result, the young patient is left with a negative memory of the dental appointment and a reluctance to be observed and treated in the future, which leads to the more frequent occurrence of advanced diseases.
Possible complications
Mandibular anesthesia in rare cases leads to the development of complications. One of them is numbness of the tissues of the pharynx with subsequent limitation of movements of the lower jaw. Physiotherapy, mechanical therapy and administration of medicinal solutions are prescribed as treatment. A hematoma can occur as a result of damage to a vessel. If it does not resolve on its own, a puncture may be required. When a nerve is damaged, neuritis sometimes develops, the treatment of which requires physiotherapeutic procedures using heating elements or electric current. A very rare complication is temporary muscle paralysis as a result of medical error. If the injection technique is violated, the needle rarely breaks off and gets stuck in soft or tendon tissue. In such cases, surgical removal is used after an X-ray examination. If the needle does not cause concern to the patient and has grown into the tissue, it does not need to be removed.
Relevance
Most dental interventions are performed under local anesthesia, the effectiveness of which depends on the correct anesthesia technique [3, 4, 9]. Among the variety of different intraoral methods of anesthesia of the inferior alveolar nerve (mandibular anesthesia), there is no universal method that would be based on topographic-anatomical data. Doctors most often use the pterygomandibular fold as a reference point for mandibular anesthesia. However, when a needle is inserted medial to the pterygomandibular fold, anesthesia may spread to the tissues of the oropharynx and damage to the internal pterygoid muscle with subsequent development of contracture of the mandible [5-8]. The danger of this complication increases when the needle is inserted into a muscle tendon (usually the temporal muscle). When a needle is inserted into the pterygomandibular fold or into its lateral edge, vascular damage and hemorrhage may occur, sometimes the formation of a hematoma, the entry of anesthetic into the bloodstream, the appearance of ischemic zones on the skin of the lower lip, chin, and even a needle fracture. The prevalence of post-injection neurological disorders after mandibular anesthesia is 0.01%. Most often, paresthesia of the lingual nerve is observed [1, 2, 10, 11]. The search for new methods of effective and safe anesthesia remains a pressing problem in dentistry.
The purpose of the study is to increase the effectiveness of anesthesia in the lower jaw teeth and reduce the likelihood of complications using a universal method of local anesthesia based on topographic and anatomical studies.
Recommendations after the event
Any type of anesthesia is stress for the body, which must be minimized. Immediately after applying anesthesia, you must rise from the dental chair carefully to avoid dizziness. After pain relief, you must avoid drinking hot and alcoholic drinks. Do not massage the injection area or eat hot food. It is necessary to rinse your mouth with soda-salt or any other solution as prescribed by your doctor several times a day. It is better to sleep on the side opposite to the injection.
Anesthetic solutions
Various compounds are used to innervate the lower jaw. These include lidocaine and novocaine. These substances are time-tested, but are highly toxic. Along with them, articaine anesthetics are used, which give excellent results with less toxicity. These include ultracaine, articaine, ubistezin.
Novocaine is not used in dentistry, since there are more powerful and safer anesthetics of the articaine series. They are 4-5 times superior to novocaine in terms of the degree of analgesic effect.
Articaine drugs, in addition to anesthetic substances, contain vasoconstrictor components such as epinephrine or adrenaline. This ensures that the anesthetic substance remains in the tissues for a long time, since it is not carried by blood vessels outside the area of medical intervention.
Mepivacaine
This short-acting anesthetic is more attractive for patients who have simply had a tooth removed or a cavity filled. After instillation of a long-acting substance, the patient leaves the dentist with numbness in half of his face, and this causes great inconvenience. Loss of sensitivity for 5-6 hours is very unpleasant.
Preparations based on mepivacaine act on tissue for no more than 40-45 minutes, which is quite enough for short dental procedures. The numbness goes away quickly, and the patient can safely eat and drink drinks at the prescribed time without experiencing discomfort.
Medicines based on mepivacaine are recommended for patients with:
- cardiovascular pathologies;
- burdened with allergic anamnesis;
- small carious lesions of molars;
- periodontal pathologies.
Also, short-acting painkillers are indicated for removing surgical sutures, applying bandages, removing intact teeth and other simple manipulations. If the patient only needs to change the iodoform bandage, there is no reason to anesthetize half of the face for 4-6 hours.
Anesthesia during pregnancy
Pregnant women are prescribed anesthesia with drugs that do not cross the placental barrier. That is, they do not penetrate the placenta. These include articaine drugs - ultracaine and ubistezin. The listed solutions also do not pass into breast milk, so they can be used without fear during breastfeeding.
All dental procedures using anesthesia are recommended to be carried out no earlier than the second trimester; in earlier stages of pregnancy, unpredictable complications are possible.
Mandibular anesthesia in childhood
The child’s body is not yet sufficiently adapted to the environment, so the reaction to anesthetics is different. However, it is not recommended to treat children’s teeth without anesthesia due to the risk of severe psychological discomfort and fear. Therefore, anesthetics are used widely and successfully. The dose of administration of the medicinal solution depends on the age of the child and is calculated according to the established formula.
Complications after the use of anesthesia in children are the same as in adults:
- spasm of the masticatory muscles;
- loss of sensation;
- hematoma (bruise);
- swelling of the mucous membrane (allergies).
For children with a mobile nervous system and too excitable, a different type of anesthesia is used - sedation. The child is put into a state of superficial sleep.
Hypnosis as a method of anesthesia
A separate group is represented by verbal manipulation, which includes the method of suggestion - hypnosis. The doctor puts the patient into an altered state by instilling a certain idea. After this, the patient stops experiencing pain. This method is convenient for patients with intolerance to a large number of drugs, as well as with serious damage to the liver and internal organs.
Contraindications for mandibular anesthesia
Mandibular anesthesia is not used for liver diseases, which is associated with a large load on it. Novocaine is the only anesthetic that is not subject to this contraindication. If a major operation is required, local anesthesia is not suitable due to the need to administer a large amount of it. Epilepsy and mental illness, as well as problems of the cardiovascular system are contraindications to mandibular anesthesia. During pregnancy, it is necessary to weigh the risk to the fetus when exposed to drugs. For blood diseases and bronchial asthma, mandibular anesthesia is not performed. Contraindications to anesthesia must be considered individually; sometimes their list can be shortened or, conversely, expanded at the discretion of the attending physician.
Results and discussion
The conducted topographic-anatomical study made it possible to establish that on the inner surface of the branch of the lower jaw there is an area (triangle) free from the branches of the trigeminal nerve, through which safe access to the lower alveolar nerve can be provided when performing mandibular anesthesia. The boundaries of the mandibular triangle in front were the anterior edge of the ramus of the mandible and the tendon of the temporal muscle, the lingual nerve was located behind and medially, the buccal nerve and the lower edge of the lateral pterygoid muscle were located above. The average dimensions of this triangle were: on the lateral side - 18±0.5 mm, on the medial side - 20±1 mm, on the top - 15±0.5 mm. In a wide-open mouth position, this triangle was projected onto the oral mucosa behind the mandibular molars (Fig. 1).
Rice. 1. Topographic anatomy of the mandibular triangle located in the pterygomaxillary space.
Based on the topographic-anatomical study of the retromolar space, an “intermaxillary triangle” was identified on the oral mucosa, which was projected onto the mandibular triangle, identified on the inner surface of the mandibular ramus. The apex of the intermaxillary triangle was facing the retromolar fossa, the base was located at the level of the alveolar process of the maxilla. The medial border of the premaxillary triangle was the pterygomaxillary fold, and the lateral border was the groove of the oral mucosa, formed in the position of the mouth wide open by the anterior edge of the branch of the lower jaw.
The experimental study made it possible to topographically substantiate the universal method of apodactylic administration of mandibular anesthesia. To carry out mandibular anesthesia, the “intermaxillary triangle” was used as a landmark for the needle insertion site. The needle is inserted with a syringe into the oral mucosa directly in the center of the triangle indicated earlier. The bevel of the needle was directed to the branch of the lower jaw to facilitate its advancement. Inserting the needle within this triangle and advancing it 15 mm in depth was safe, since the needle was located between the inner surface of the mandibular ramus and the lateral surface of the medial pterygoid muscle along with the lingual nerve. The syringe was located in the corner of the mouth at the level of the canine on the opposite side of the lower jaw. An anesthetic depot was created in an amount of 1.7 ml. After the experimental study, the pterygomaxillary space of the deep region of the face was prepared using sectional material.
It was established that this method of mandibular anesthesia was carried out without damaging the internal pterygoid muscle, lingual, inferior alveolar nerves and blood vessels, and the anesthetic was located near the neurovascular formations (Fig. 2, 3).
Rice. 2. Performing mandibular anesthesia on a topographic-anatomical preparation of the lower jaw in the intermaxillary triangle.
Rice. 3. Method of performing mandibular anesthesia (diagram). A priority certificate for invention No. 2017141093 dated November 28, 2017 was received for this method of mandibular anesthesia.
In a clinical study, anesthesia was performed for the purpose of painless preparation of hard tissues of the mandibular molars and surgical manipulation of the mucous membrane of the lateral floor of the mouth and tongue. The technique of this apodactyl method of mandibular anesthesia: the anesthetic was administered, focusing on a number of anatomical formations. With the mouth wide open, the needle was inserted into the middle of the intermaxillary triangle. The direction of the needle was at an angle to the branch of the lower jaw. The syringe was located in the corner of the mouth, at the level of the canine of the lower jaw, on the side opposite to anesthesia (Fig. 4, a,
Rice. 4. Method of performing mandibular anesthesia. b). The needle was advanced until it made contact with the bone tissue. An anesthetic depot of 0.3 ml was created. Next, the needle was advanced parallel to the inner surface of the lower jaw branch deep into the pterygomaxillary space by 15-20 mm. After the aspiration test, an anesthetic depot of 1.7 ml was created. Anesthesia in the area of innervation of the lingual nerve occurred after 3-5 minutes, the inferior alveolar nerve - after 5-7 minutes and continued, depending on the local anesthetic solution used and the concentration of the vasoconstrictor, up to 1.5 hours. The onset of anesthesia was determined by the appearance of feeling in the patient numbness and tingling on the corresponding half of the tongue and lower lip. The manipulations performed were painless in all 20 (100%) patients. In 7 (35%) patients, there were signs of anesthesia in areas of the oral mucosa included in the zone of innervation of the buccal nerve on this side. When performing mandibular anesthesia using this method, complications associated with damage to the lingual, buccal, inferior alveolar nerves, and medial pterygoid muscle were not observed.
Extraoral access
Extraoral anesthesia of the inferior alveolar nerve is carried out by three main methods: submandibular, subzygomatic and retromandibular.
With the submandibular method of anesthesia, the syringe needle is inserted into the skin under the inner surface of the lower edge of the jaw at a distance of 1.5 cm from the angle. The needle moves along the bone at the level of the posterior edge of the branch by 3.5-4 cm. The anesthetic depot of 1 ml created in this way helps to block the inferior alveolar nerve. Blocking the buccal and lingual nerves is achieved by moving the needle an additional 1 cm forward while adding 1 ml of anesthetic. The needle is moved 4 cm in the direction from the lower edge of the jaw, and an anesthetic solution is injected into the tissue at the same time. Additional movement of the needle to the area of the lingual and buccal nerves is due to the need to anesthetize the intervention zone of the three nerve areas.
This method of pain relief is also applicable if the patient’s neck is shorter than usual. The syringe is attached to the needle after it is injected at the level of the mandibular foramen. The thing is that the syringe itself creates a barrier to the movement of the needle to the bone level.
The subzygomatic approach, or Bershe Dubov approach, is characterized by inserting a needle into the skin. The injector is inserted at an angle of 90 degrees to its surface under the lower edge of the zygomatic arch, and a couple of centimeters from the base of the tragus of the auricle. Advancing the needle no deeper than 3-3.5 cm allows you to reach the inner surface of the marginal pterygoid muscle. Two mm of anesthetic substance in this case will be enough. Blocking of the lower alveolar, lingual and buccal nerves occurs after 10 minutes, and complete elimination of the contracture of the lower jaw is observed a little earlier.
The last option for extraoral anesthesia of the inferior alveolar nerve is a puncture of the gland located behind the ears. With this method of access to the site of dental interventions, there is a risk of touching the carotid artery, or even a branch of the facial nerve. Hence the rarity of its use, but it still exists as an anesthesia option.
Features of local anesthesia for double socket nerve
Mandibular anesthesia, as the main method of anesthetizing teeth in the lower jaw, has been known since the end of the nineteenth century. The very principle of its implementation has remained unchanged, but the technique has undergone a number of changes.
Thus, classical mandibular anesthesia is performed in the area of the mandibular foramen (Halsted method, 1885; Fischer, 1911; Egorov). “High” methods of blocking the inferior radial nerve have become more modern, during which an anesthetic depot is created in the area of the torus of the lower jaw (Weisbrem, 1940), the notch of the lower jaw with the patient’s mouth closed (Vizirani, 1960, - Akinozi, 1977), and the articular process mandible (Gow-Gates, 1973). Such a variety of methods makes us think that there is a problem in carrying out local conduction anesthesia of the teeth of the lower jaw. According to a number of researchers, mandibular anesthesia is ineffective in 10-15% of cases [12].
One of the reasons for its ineffectiveness is the anatomical variations in the structure of the mandibular nerve and canals [13].
There are studies confirming that mandibular anesthesia is in most cases ineffective when the patient has a double mandibular canal. It was noted that after its implementation in this group of patients, the pain sensitivity of the dental tissues remains, at the same time, there is a feeling of numbness of the lower lip and chin on the corresponding side of the anesthesia [7, 8, 12, 13, 16, 17].
Anatomy of the inferior alveolar nerve
The mandibular nerve is a continuation of the third branch of the trigeminal nerve and is located in the thickness of the lower jaw along the length from the mandibular to mental foramina. According to a number of authors, the mandibular nerve along its entire length forms three main branches: the retromolar branch, the molar branch, and the incisive branch [1-3]. Throughout its entire length, the mandibular nerve can run as one main bundle, but can be divided into two [4] or even three branches [5].
In terms of prevalence, double inferior alveolar canal occurs in less than 1% of the population. Thus, according to Grover PS and Lorton L., when studying 5000 orthopantomograms, a double lower alveolar canal was observed in 4 cases (0.08%) [7]. According to other authors, a study of 6000 OPTG revealed double mandibular canals in 57 cases (0.95%) [6].
Classification of double mandibular canals
Having studied 3612 OPTGs, Notje et al. identified the following variations in the structure of the double mandibular canal: type 1 - two canals that begin through a single opening; type 2 - branch of the small canal at the level of the second and third molars; type 3 - two canals begin from different foramina, but unite at the level of the molars [6]. Heasman proposed a classification of the position of the canal in relation to the roots of the teeth: 67.7% - type 3 (average), 15.6% - type 2 (high), 5.2% (low), type 4 (mixed) - 11.5 % [8].
The most famous is the Langlais classification of double canals of the lower jaw (Fig. 1): type 1 - bifurcation at the level of the third molar (0.367%), type 2 (0.517%) - bifurcation within the jaw ramus or beyond, then union, type 3 - mixed (0.03333%): on the one hand type 1, on the other - type 2, type 4 (0.03333%) - two channels that begin with different holes [9].
Rice. 1. Classification of double mandibular canals according to Langlais.
Formation of a double channel
Of course, the double alveolar nerve is an anatomical variation in the structure of the jaws, which is formed during the prenatal period of development. Johansson et al. found that the development of the mandibular nerve proceeds from three independent canals, which then combine into one canal. [10]. Chaves et al., studying preparations of the jaws of prenatal children, found that the mandibular canal is divided into three independent highways that innervate a certain group of teeth. Thus, the first canal approaches the rudiments of the incisors and canines, the second - to the premolars, the third - to the molars of the lower jaw. This fact largely explains why, in primary adentia, the lesion affects a certain group of teeth on each side of the lower jaw [11].
During the development of the lower jaw, intramembranous ossification, three independent canals with nerve trunks are combined into a canal with the nerve of the same name. Currently, there is no consensus on the reason for the formation of the double mandibular canal. However, it can be assumed that changes in the mineralization of the jaws during the developmental stages of the child may prevent the approximation of the main branches of the mandibular nerve, which leads to the development of several independent canals.
Tactics of local anesthesia for double inferior alveolar nerve
Before starting dental treatment, it is necessary to conduct an additional X-ray examination, such as orthopantomography. It allows you to evaluate the position of the mandibular foramen in relation to the occlusal surface of the molars, the number of canals, and their topography according to Langlais.
For anesthesia of the teeth of the lower jaw with a double mandibular canal, “high” methods of anesthesia are recommended (torusal, Gou-Gates, Vizirani-Akinozi). Of course, it is not advisable to do OPTG for each patient before mandibular anesthesia, but it is worth thinking about performing it in cases where the patient himself complains about the “ineffectiveness” of pain relief during dental treatment. It is safe to say that there is a group of patients with an unfavorable history in relation to local anesthesia, for whom X-ray diagnostics, up to computed tomography, are actually indicated to identify the reasons for the ineffectiveness of local anesthesia.
For anesthesia of the teeth of the lower jaw with a double mandibular canal, “high” methods of anesthesia (torusal, Gou-Gates, Vizirani-Akinozi) are recommended. They ensure the creation of an anesthetic depot above the mandibular foramen, thereby resolving the issue of an anomaly in its position with a double mandibular canal.
If the doctor prefers classical mandibular anesthesia, its effectiveness should be assessed after an average of 10 minutes. If the patient notes a feeling of numbness of the chin, but there is no anesthesia of the pulp, the anesthetic depot has been created correctly and there is no need for repeated mandibular anesthesia. Repeated mandibular anesthesia should be carried out using the “high” type and only if the patient does not have a feeling of numbness in the chin and lower lip. As an additional method of pain relief, it is recommended to carry out intraligamentary or intraosseous anesthesia, which is guaranteed to lead to anesthesia of a specific tooth.
Clinical case
Patient V., born in 1982, complained of periodic pain in tooth 37. Objectively: 38 - partially erupted with a mesioangular position. DS: Dystopia 38. During the examination, an OPTG was performed, which revealed a double mandibular canal, presumably starting with one mandibular foramen, then running separately along the entire length of the ramus and body of the mandible and ending with two foramina (type 2 according to Langlais) (Fig. 2, 3). The patient was recommended to remove 38. From the anamnesis, it was found that during previous dental interventions there were often problems with pain relief.
For the operation of removing tooth 38, mandibular anesthesia was performed by palpation (1.8 ml Ubistesin 1:100000 3MESPE) and buccal infiltration anesthesia (0.5 ml Ubistesin 1:100000 3MESPE). 5 minutes after anesthesia, the patient noticed a feeling of numbness in the edge of the lower lip on the left. During the creation of surgical access and partial odontopreparation, patient 38 experienced pain. As an additional anesthesia, intraligamentary anesthesia (0.8 ml Ubistesin 1:100000 3MESPE) was performed, the tooth was removed painlessly.
Discussion
In this clinical example, the patient received standard anesthesia used for the extraction of lower jaw teeth. However, in this case, there was no complete anesthesia of the pulp 38. The authors of the article suggest that this problem is associated with the presence of a double mandibular canal in the patient. The double mandibular canal contains both nerves and vessels responsible for the blood supply to the mandible [6].
It is believed that the main canal, which opens at the level of the occlusal surface of the molars and has a larger diameter, always contains the mandibular nerve. The additional canal, which has a smaller diameter, in most cases starts from the main mandibular foramen. There are double mandibular canals, which begin with two independent openings, while the additional opening can be located either above the main one, closer to the base of the articular process, or below the main one, in the distal part of the jaw branch.
The main canal, which opens at the level of the occlusal surface of the molars and has a larger diameter, always contains the mandibular nerve. According to the literature, the additional canal of the lower jaw may contain branches of the mylohyoid nerve (n. myelohyoideus), which is closest in topographic-anatomical relation to the mandibular nerve . The mylohyoid nerve is not amenable to anesthesia during standard mandibular anesthesia due to the fact that the anesthetic cannot diffuse through the sphenomandibular ligament, through which the mylohyoid nerve passes [14].
According to Wilson, this is explained by the fact that the mylohyoid nerve branches from the mandibular nerve 14.7 mm above the mandibular foramen, i.e., this zone may be outside the range of action of the local anesthetic solution [15]. Lew et al. described a clinical case of ineffective local anesthesia of the mandibular teeth in a patient with a double mandibular canal [13], DeSantis et al. described a similar case [17], in this article the authors also encountered this problem. At the same time, there is evidence of the effectiveness of mandibular anesthesia in patients with a double mandibular canal [16].
Conclusion
A double mandibular canal may cause failure of mandibular anesthesia. This is largely due to the dislocation of the additional mandibular foramen and the innervation of the teeth from the mylohyoid nerve. Additional x-ray diagnostics (OPTG, CT) allows us to find out the reason for the ineffectiveness of anesthesia of the lower jaw. When identifying double mandibular canals using an x-ray, you can determine their topography, choose the technique of conduction anesthesia and the planned location for creating a local anesthetic depot.
LITERATURE
- Oikarinen VJ. The inferior alveolar artery. SuomHammaslaToim 1965;61(Suppl 1):1–131.
- Poirot G, Delattre JF, Palot C, Flament JB. The inferior alveolar artery in its bone course. SurgRadiolAnat 1986;8:237–244.
- Zoud K, Doran GA. Microsurgical anatomy of the inferior alveolar neurovascular plexus. SurgRadiolAnat 1993;15:175–179.
- Northje, C.J.; Farman, A.G.; Grotepass, FW Variations in the normal anatomy of the inferior dental (mandibular) canal: a restrospective study of panoramic radiographs from 3,612 routine dental patients. Brit. J. oral Surg., Edinburgh, v. 15, p. 55-63, 1977.
- Auluck, A.; Keerchilatha, MP Trifid mandibular nerve canal. Dentomaxillofac. Rad., London, v. 34, no. 4, p. 259, Jul., 2005.
- Northje, C. J.; Farman, A.G.; Joubert, JJV The radiographic appearance of the inferior dental canal: an additional variation. Brit. J. oral Surg., Edinburgh, v. 15, p. 171-2, 1977.
- Grover, PS & Lorton, L. Bifid mandibular nerve as a possible cause of inadequate anaesthesia in the mandible. J. Oral Maxillofac. Surg., 41:111–9, 1983.
- Heasman, PA Variation in the position of the inferior dental canal and its significance to restorative dentistry. J. Dent., Chengtu, v. 16, no. 1, p. 36—7, Feb., 1988.
- Langlais, R. P. Broadus, R. Glass, B. Bifid mandibular canals in panoramic radiographs. Journal of the American Dental Association (1985), Vol 110, Issue 6, 923-926.
- Johansson CS, Hildebrand C, Poulsen B (1992). Anatomy and developmental chronology of the rat inferior alveolar nerve. AnatRec 234:144–152.
A complete list of references is in the editorial office.
Extraoral (tuberal) anesthesia
The method is practiced during long-term surgery or in case of jaw injuries, when the patient is unable to open the oral cavity.
Indications:
- extensive inflammatory process of oral tissues;
- long-term surgical intervention - 2 or more teeth;
- injury to the bones and muscles of the jaw.
The anesthetic anesthetizes a large area of the facial part of the skull, including 2/3 of the tongue, all teeth on the selected side, the alveolar process, gum tissue, and the skin of the lower lip.
Methods of administering anesthetic differ in the location of the needle insertion:
- submandibular;
- retromaxillary;
- anteriormaxillary.
This method of pain relief is especially indicated in the treatment of children, who may be difficult to force to open their mouths for therapy. Also, conduction anesthesia is indicated for severe infection of the oral mucosa, accompanied by copious secretion of saliva. In such conditions it is difficult to maintain sterility and it is easy to add a new type of infection to an existing one. Also, children do not always comply with the dentist’s request not to close their mouth, preventing the doctor from performing manipulations in compliance with sanitary standards.
Another problem when treating children: they do not understand the request not to touch the mucous membrane sanitized with antiseptics with their tongue and often change the position of their head, provoking contamination of the mucous membrane treated for medical manipulation. Therefore, the extraoral route of pain relief is the only possible method when dealing with young patients.
Postmaxillary route of mandibular anesthesia
This method was proposed by Peckert and Wustrow in 1937. The essence is to instill an anesthetic from a point at the posterior edge of the arch of the lower jaw to the pterygoid muscle. The advantage of the method is the accessibility of the inferior alveolar nerve, the path to which is not blocked by the uvula of the lower jaw. The nerve can be blocked from a great distance, so there are no obstacles to successful blocking.
However, the method is also characterized by disadvantages, among which there is a very significant one - puncture of the parotid gland. Also, for instillation, a needle of a special shape is required - with a curve. If the needle breaks, it will be difficult to remove the fragments. For patients, instillation at the specified point is felt as painful, and the proximity to the injection point of the carotid artery adds additional risk to the manipulation. Therefore, the retromaxillary method is practically not used in modern dentistry.
Submandibular path
This method is much safer than the mandibular method. During the puncture, the needle moves parallel to the jawbone. To find the correct place to insert the needle, you need to place your hand on your neck so that your index finger touches the lower edge of the auricle. Then the thumb will indicate the point through which instillation is carried out.
If it is necessary to block the nerves in the right facial part, the patient's left hand is used to determine the injection point. Accordingly, to determine the point of entry of the needle into the left part of the facial zone, use the right hand. This technique was proposed by German scientists Sicher and Klein in 1915.
The extraoral anesthesia technique should be mastered by every practicing dentist, as it is used in cases of inflammation in the mucous membranes of the gums and soft tissues. Thanks to it, it is possible to carry out surgical intervention, stopping pain impulses and gaining free access.
Bershe Dubov method
This is one of the types of extraoral anesthesia of the lower jaw, from the subzygomatic part of the skull. The needle is inserted under the zygomatic area of the face two centimeters from the tragus of the ear. Novocaine is used as an anesthetic, but other options are also possible. After instillation, the entire half of the jaw is frozen.
Dubov slightly modified Berche's technique, simply changing the depth of insertion of the needle into the tissue: it increased by 1 cm.
Uvarov also made his own adjustments to the technique of administering the anesthetic according to Berchet, proposing to insert the needle to a depth of 4.5 cm. Compared to the proposal of Berchet (2.5 cm) and Dubov (3.5 cm), this looks somehow bold. Berdyuk and Egorov proposed their own adjustments. Their innovations are associated with changing the angle of the needle.
Anteriormaxillary path
This anesthesia technique is not widely used due to the risk of puncture of the cheek and penetration of the needle into the oral cavity. Although, with a successful injection, three nerves can be immediately anesthetized - buccal, lingual and inferior alveolar.