Pathology of the connecting joint between the lower jaw and the temporal bone. In the acute stage, the following symptoms are noted:
- intense pain in the affected area;
- swelling of the skin over the joint;
- restriction of movements when opening and closing the jaw;
- increased basal temperature.
To make a diagnosis, the doctor examines the patient’s medical history, conducts an examination, and prescribes computer tests.
Methods of treating the disease:
- jaw immobilization;
- antibiotic therapy;
- local administration of corticosteroids;
- myogymnastics;
- physiotherapeutic measures.
General characteristics of the pathology
What is jaw arthritis
In medicine, this pathology is called arthritis of the temporomandibular joint, or TMJ arthritis. Due to this joint, the lower jaw moves and makes it possible to make movements with the mouth.
Arthritis of the maxillary facial joint is a disease that is a complex inflammatory process of this joint.
The pathological process can occur in both acute and chronic forms. A distinctive feature of the development of the anomaly is the limited mobility of this structure.
The disease is complex, it is treated by specialists of different profiles.
According to ICD 10, the specified pathological process is assigned code K07.6.
There are several forms of this disease, depending on the location of the pathological process. This:
- arthritis of the upper or lower joint;
- arthrosis of the upper jaw joint. The disease occurs when there is severe deformation of the joint. In this case, the lesion spreads to both areas of the jaw node, destruction of cartilage tissue occurs
The pathological process is characterized by the unilateral nature of the lesion. During the first stages of the pathological process, inflammation of the joint capsule and surrounding soft tissue occurs. As the pathological process spreads, cartilage tissue and articular surfaces are damaged. Because of this, lesions with connective tissue are formed.
Causes of TMJ dysfunction
Conventionally, we can distinguish 3 main reasons for the development and etiology of the clinic of TMJ jaw joint dysfunction:
- Imbalance and disruption of the nervous coordination of the jaw muscles that raise and lower the lower jaw. Most often, the tone and tension of the muscle fibers in the right and left masticatory muscles are first disturbed, and then their imbalance occurs, irritation of the bilaminar zone and pain when chewing and swallowing.
- Chronic stress, over a long period of time (from a year or more), caused by a disorder of the central nervous system and higher nervous activity.
- Malocclusion and occlusion (closing) of teeth, coupled with non-standard sizes and position of the jaws relative to each other and the base of the skull.
As a rule, all of the above factors, to a greater or lesser extent, occur if a diagnosis of TMJ dysfunction syndrome is made. Reviews from patients and a forum on the Internet confirm this.
A hereditary predisposition to dysfunction of the jaw joints has been proven, with genetic anomalies associated with malocclusion, especially with micrognathia and macrognathia of the lower or upper jaw.
Risk factors
A number of reasons can lead to the development of arthritis of the jaw.
Violation of the structure occurs due to the following reasons:
- traumatic factor. The cause in this case may be a blow, a fracture, or a sudden opening of the mouth;
- infectious diseases of the ENT organs or lower jaw. Arthritis of the maxillary joint is caused by streptococci, chlamydia, mycobacterium tuberculosis, and various viruses;
- osteomyelitis;
- untreated caries or periodontitis;
- otitis, mumps. Arthritis is a complication of these pathologies;
- gout;
- reactive arthritis;
- systemic lupus erythematosus;
- metabolic disorders;
- diabetes;
- thyroid diseases;
- rheumatoid arthritis.
Sometimes inflammation is a consequence of hypothermia.
Pathogenesis
The study of the mechanisms of development of pathology allowed us to come to conclusions about their progression associated with a lack of physiological endurance of the joint.
The resulting injuries and the appearance of inflammation lead to improper distribution or excessive load on the tissue, which causes disruption of the synchronization of the joints, causing loss of functionality of the muscular system. The result of the development of such unpleasant processes is a disruption of the nutrition of cartilage tissue, as well as a gradual loss of their elasticity, which inevitably leads to destruction.
Simultaneously with all of the above, serious transformations of bone tissue develop, which provokes the formation of growths that modify the elements of the joint: the head of the lower jaw changes shape, and signs of osteoporosis are visible.
As a result of the uncontrolled course of pathological processes, severe deformation and serious disruption of the tissue structure occur.
Clinical picture (symptoms)
Arthritis is accompanied by pain and discomfort.
The disease manifests itself in the following characteristic symptoms:
- pain in the jaw area, which radiates to other parts of the face and intensifies with movements and opening the mouth;
- dizziness;
- sleep disorders;
- limited movement in the joint;
- feverish condition;
- inflammation of the skin and soft tissues around the joints;
- elevated temperature;
- clicking in the jaw area when it moves;
- temperature rise up to 38 degrees, sometimes higher;
- pain when palpating the affected area (joint pain);
- deformation of the contours of the face due to the fact that the chin “goes” to the side;
- feeling of weakness, increased fatigue;
- hearing impairment.
Important! With arthritis of the jaw joint there is a risk of the formation of purulent inflammation. In this case, the joint swells and the skin becomes red and hypersensitive. A lump is felt in the area of the mandibular joint. The shade of the skin changes, speech and chewing functions are impaired.
Diagnostics
During an in-person examination, the dentist reveals a limitation, and a significant one, in the opening of the mouth, as well as a significant narrowing of the amplitude of jaw movement. To confirm the diagnosis, such patients are prescribed orthopantomography, teleradiography or computed tomography. A blood test will show signs of inflammation. If TMJ arthritis is rheumatoid, C-reactive protein increases. According to indications, magnetic resonance imaging is prescribed, which reveals disc displacement and degenerative changes. Primary damage to the muscle tissue is confirmed when the pain becomes stronger upon palpation.
As a result of the studies, purulent-septic diseases are excluded, the range of motion and functions of the joint are assessed. The minimum norm when opening the mouth is about 40 millimeters. Sound phenomena are common, but their occurrence does not indicate the need for therapy. If pain occurs with clicking and limited movements, therapeutic procedures are performed.
Types of deviations in the maxillofacial joint
The clinical picture of this disease depends on the form in which arthritis of the jaw joint occurs.
Types of disease:
| Type of pathology | Characteristics |
| Acute form | The predominant symptoms in this case are severe pain in the affected area and swelling of the soft tissues. Typically, acute arthritis of the jaw joint occurs after traumatic injury. |
| Chronic arthritis | With this form, aching pain is constantly observed in the jaw joint. In the morning, jaw mobility is limited. Body temperature usually does not increase, the general condition of the body is satisfactory. |
| Infectious arthritis of the TMJ | Usually this type of pathology is a consequence of previous diseases - influenza, tonsillitis. In the infectious form of arthritis, severe pain is observed, during which it is impossible to open the mouth freely. Unpleasant sensations radiate to the area of the ear, back of the head, and temple. |
| Traumatic | This is the most common form of arthritis of the maxillary joint. It occurs against the background of an injury. |
| Specific | This type of disease occurs quite rarely. Typically, specific arthritis is a consequence of previous diseases - syphilis, gonorrhea, tuberculosis. |
| Non-specific | In this case, the inflammatory process occurs due to traumatic or rheumatoid factors. |
| Purulent | This form of pathology is a consequence of acute arthritis, which has been neglected. A thickening appears in the area of the mandibular joint, and body temperature rises. |
| Rheumatoid | The disease manifests itself in constant pain localized in the area of the maxillary joint. In this case, the clinical picture is often supplemented by pain that is localized in the area of the knee, hip or elbow joint. |
Depending on what exactly caused the development of the inflammatory process, the following paths are distinguished:
- hematogenous . In this case, the pathogen penetrates the joint area along with the blood flow. This method of infection is possible with tuberculosis, syphilis, gonorrhea, scarlet fever, measles;
- contact . The disease develops against the background of damage to the sections that are located next to the maxillary joints. A similar thing is observed with otitis media, purulent mumps, phlegmon or abscess of the parotid-masticatory area;
- straight . Arthritis of the maxillary facial joint in this case develops due to direct infection, which occurs due to injuries or fractures of the jaw.
It is possible to determine the form in which the pathological process occurs only after carrying out specific diagnostic measures.
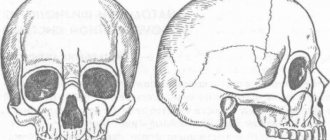
Features of the structure of the temporomandibular joint
The temporomandibular joint is involved in any movement of the jaw
The temporomandibular joint is a complex structure of two pairs of bones, on the left and right sides respectively. The peculiarity of arthritis in this area is that the paired bones are closely interconnected, so damage to the temporal bone on the right will necessarily negatively affect the condition of the mandibular bone, and vice versa.
TMJ arthritis always affects the bones symmetrically. Therefore, with the development of the disease on the right, over time there is a disruption of the joint in the left side of the head.
The temporomandibular joint is characterized by high mobility and is involved in almost any movement of the head and jaw. The process of chewing food, active facial expressions, conversation - the temporomandibular joint is involved in all these simple actions. It works constantly and withstands intense loads every day.
The articulation is formed by the upper part of the mandibular bone and the fossa of the temporal bone. The joint is small in size, but hidden by a large number of strong elastic ligaments. High mobility of the jaw is ensured by a disc hidden in the articular cavity.
Disruption of the normal functioning of the TMJ due to arthritis leads to the development of severe symptoms and significantly worsens the patient’s quality of life. This disease is quite difficult to treat and requires an integrated approach.
Methods for diagnosing arthritis of the jaw joint
Arthritis on x-ray
Diagnosis and treatment of the inflammatory process in the jaw joint area can be carried out by different specialists, which depends on the cause that caused its development. This could be an ENT doctor, a dentist, a traumatologist, an infectious disease specialist, or a dermatovenerologist.
The main diagnostic measures include:
- radiography . During this diagnostic exercise, widening or narrowing of the joint space is detected, which indicates acute or chronic arthritis of the TMJ, respectively;
- magnetic resonance imaging . The method allows you to study the condition of soft tissues, estimate the amount of fluid in the joint cavity;
- CT scan . This method of research makes it possible to differentiate between healthy and damaged tissues;
- ultrasound diagnostics . Using this research method, it is possible to visualize the fluid in the joint cavity. However, it is impossible to fully study the structure of soft tissues in this way.
Note! Acute arthritis of the TMJ is differentiated from such pathologies as acute otitis media, trigeminal neuralgia, gout.
After obtaining the necessary data and making a diagnosis, an individual course of treatment is developed.
Cost of treatment for TMJ dysfunction
Answering questions frequently asked by patients: “How much does treatment for TMJ dysfunction cost, with a discount, at a promotion? Where and how much cheaper are the prices for such turnkey treatment, in Moscow, St. Petersburg or other cities of Russia?”, it should be noted that the price of treatment for pathology and dysfunction of the TMJ jaw joints and the cost of its individual stages depends on the following points:
The cost of diagnosing TMJ dysfunction starts from 10,000 rubles and can reach 80,000 rubles or more. The price of treatment starts from 15,000 rubles and can reach 300,000 rubles or more.
- From the complexity of diagnosis and the number of medical procedures
- From the qualifications of gnathologists, orthodontists and other specialists
- From the pricing policy of each specific dental center
Just pick up the phone and call us!
8
We will definitely make you an offer that you cannot refuse!
Treatment options
Pathology is treated in the following ways:
- Fixation
fixation . The first thing that is done when arthritis of the jaw joint is diagnosed is to ensure the immobility of the affected structure. To do this, apply a bandage. On the side of the diseased joint, between the teeth, a special plate is placed, which should remain there for 2-3 days;
- taking medications . The patient is prescribed analgesics to suppress pain and reduce temperature (Nurofen, Analgin), antibacterial drugs (Tetracycline, Amoxicillin), non-steroidal anti-inflammatory drugs (Celecoxib, Nimesulide). Immunosuppressants may be prescribed, which is required for rheumatoid arthritis. The group of such drugs includes Etanercept, Leflunomide;
- drug blockade . The goal of therapy is to relieve pain in the affected joint. Novocaine injections may be prescribed;
- ointments, compresses . For pain in the affected joint, topical agents are prescribed, for example, ointments containing bee or snake venom. Ointments, by heating the affected area, restore joint mobility and suppress muscle spasms;
- sanitation of the oral cavity . This method is required for rheumatoid arthritis.
Drug blockade
Exercise is another way to restore the mobility of an inflamed joint at home. The specialist prescribes a course of therapeutic exercises for the patient. The most effective and common exercise is to open the mouth using only the upper part of the jaw.
Physiotherapy helps with TMJ arthritis. Effective measures include:
- magnetic therapy;
- laser therapy;
- mud therapy;
- ultrasound therapy;
- cryotherapy.
Therapeutic massage sessions are also available .
Surgical intervention is carried out in case of development of a purulent process, rupture of the joint capsule, fractures of the articular surfaces. During the operation, the specialist installs a drainage system.
Traditional methods of treatment include the following:
- cabbage leaf compress . You need to take one sheet, iron it with a heated iron, and apply it to the affected area. Carry out the procedure 1-2 times a day;
- compress with sea salt . It is necessary to calcinate natural sea salt in a frying pan, then wrap it in a piece of linen cloth. Apply to the affected area. Repeat application up to two times a day;
- infusion of yarrow . Pour 4 tablespoons of raw material into 400 ml of boiling water. The product should sit for 2 hours. You need to take it 4 times a day, 50 ml each time.
The condition must be corrected with the help of a doctor.
Orofacial pain is widespread in the population. Patients with facial pain see doctors from many specialties, including dentists, oral surgeons, neurologists, internists, and otolaryngologists. Diagnosing facial pain can be very challenging for a doctor.
Facial pain can be caused by a number of reasons. In the International Classification of Headache and Facial Pain, 3rd revision (ICHD-3 beta), pain syndromes in the facial area are given in Chapter 11 “Head or facial pain associated with pathology of the bones of the skull, neck, eyes, ears, nose, sinuses, teeth , oral cavity or other structures of the face and neck” and in Chapter 13 “Painful cranial neuropathies and other facial pain” [1]. It should be noted that in Chapter 11, almost all sections use the term “headache”; only one section mentions facial pain per se (11.8). In Chapter 13, pain syndromes are referred to as “neuralgia” or “neuropathy.”
Most of the syndromes listed in the ICHD are not often encountered in the practice of a neurologist. One of the common mistakes in interpreting the cause of facial pain is overdiagnosis of trigeminal neuralgia (TN) followed by long-term and ineffective treatment with carbamazepine. At the same time, it has been shown that TN is a relatively rare cause of facial pain [2].
This article will focus on temporomandibular joint dysfunction (TMD). Today, TMD is considered the most common cause of chronic facial pain not associated with dental diseases [3]. Facial pain associated with pathology in the temporomandibular joint (TMJ) occurs in 19–26% of the adult population, and in women it is observed 1.5 times more often than in men [4, 5].
Clinical picture
Patients with TMD may experience pain in the face, upper and lower jaw, neck and shoulders, and in and around the ear. The pain may be constant or appear when chewing, talking, or opening the mouth. Often the pain is also accompanied by a feeling of facial fatigue and swelling.
In addition to facial pain, patients may experience headaches, neck pain, ear pain, toothache, burning and stabbing pain in the face, as well as shooting and puncture sensations. In addition to pain, there are also more rare and therefore even more difficult to diagnose symptoms: noise, ringing or congestion in the ears, non-systemic dizziness and even itching or tingling in the head and neck area. Pain may develop gradually, but many patients report an abrupt onset of pain and associated symptoms.
The occurrence of difficulties with chewing, the inability to open the mouth wide, the appearance of crunching/clicking when opening or closing the mouth, as well as blocking of the lower jaw - all this indicates damage to the TMJ itself and facilitates diagnosis.
Diagnosis and differential diagnosis
Previously, TMD was considered exclusively as a pathology of the TMJ and as a consequence of subluxation of the lower jaw, arthritis, arthrosis or trauma to the TMJ, as well as occlusal disorders [6, 7]. However, in 2014, the Diagnostic Criteria for TMD for Use in Clinical Practice and Research (DC/TMD), developed by the International RDC/TMD Consortium Network and Orofacial Pain Special, was adopted Interest Group). In accordance with these criteria, TMD is divided into two groups: pain and intra-articular pathology; their combination is also possible [8].
A large number of patients with TMD experience a painful form, that is, pain in the area of the masticatory muscles, while no pathology of the joint itself is detected. The literature describes facial pain associated with myofascial dysfunction of the facial muscles [7, 9]. The authors indicate that when palpating the muscles on the side of pain, attention was paid to the dense consistency and tension of the muscles, especially the masticatory and facial muscles, as well as severe pain and myofascial trigger points. When palpating the masticatory muscle, pain spreads to the upper and lower jaws, upper and lower molars, ear, frontal region, TMJ, and neck. When palpating the temporal muscle, pain radiates to the corresponding half of the head, forehead, upper teeth, and orbit. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form [10], most patients can and should receive effective care from a neurologist. Thus, facial pain in a patient is most often caused by hypertonicity and myofascial pain syndrome in the masticatory muscles without pathological changes in the structures of the joint itself.
When a patient presents with facial pain, the neurologist needs to conduct a proper examination (palpation) in order to diagnose and optimally treat such patients. This will avoid unnecessary referral of patients to dentists and ENT doctors and unnecessary and often painful examinations.
New criteria for the correct diagnosis of TMD are presented in the table.
Diagnostic criteria for TMD DC/TMD for use in clinical practice and research (adapted from [8])
Thus, according to the diagnostic criteria for TMD for clinical use, pain disorders are not associated with the pathology of the TMJ itself and can be represented by myalgia, arthralgia and headache associated with TMD. The given criteria are based on anamnesis and clinical examination (palpation of the temporal and masticatory muscles) and do not require mandatory imaging studies. In myalgia, pain may be felt in the jaw, temple, ear, or anterior to the ear and usually changes with jaw movement, chewing, or parafunctional activities. This means that pain in the face, ear, anteriorly and near the ear, as well as noise in the ear may be symptoms of TMD and do not indicate the presence of an ENT pathology.
In the case of local myalgia, the pain felt by the patient is reproduced by palpation of the temporal and masticatory muscles within their palpable area. In myofascial pain syndrome, pain extends beyond the palpable area within or beyond the palpable muscle (myofascial pain syndrome with referred pain).
It should be noted that for a complete diagnosis, it is necessary to follow the correct muscle palpation protocol: 3 points in the temporal muscle (anterior, middle and posterior sections) and 3 points in the area of the masseter muscle (the beginning of the muscle, its body and its insertion) [11]. Palpation is carried out with one or two fingers on each side separately or on both sides at once (depending on the patient’s convenience), the duration of pressing to determine myalgia should be at least 2 s, if it is necessary to determine the subtype of myalgia - at least 5 s. In practice, it is also possible to palpate the masticatory muscle by pressing it with the examiner’s thumb in the patient’s oral cavity and with the rest of the fingers outside.
To determine the presence of arthralgia, it is necessary to confirm that the pain felt by the patient in the face is localized in the TMJ area and is reproduced with provocative tests: palpation in the area or around the condylar process of the mandible or with maximum active or passive opening of the mouth, lateral movement or protrusion of the mandible.
When pain is localized in the parotid region anterior to the pinna, identifying the specific structure involved may be challenging for the clinician. In this case, it is necessary to determine whether the pain is localized in the area of the condylar process of the mandible (arthralgia) or the masticatory muscle. In the latter case, one of the types of myalgia will be diagnosed. To determine the location of the condylar process of the jaw and confirm the source of the pain felt by the patient, it is necessary to palpate the preauricular area with the mouth closed. In case of difficulty, palpation should be performed when opening the mouth or moving the lower jaw forward (Fig. 1).
Rice. 1. Palpation to determine the location of the condylar process of the mandible. a - with comfortable closing of the mouth; b - with protrusion of the lower jaw.
To find the points of palpation of the masticatory muscle, it is necessary to ask the patient to clench and then unclench his teeth. In this case, determining the boundaries of the palpated muscle is greatly simplified (Fig. 2).
Rice. 2. Palpation of the masticatory muscle to determine the shape of the TMD. a — the origin of the muscle; b - muscle body; c — muscle attachment zone.
Palpation of the temporal muscle is much simpler. It is necessary to palpate at least 3 points in the anterior, middle and posterior portions of the muscle (Fig. 3). If there is difficulty in finding the boundaries of the temporal muscle, the patient should be asked to clench his teeth.
Rice. 3. Palpation of the temporal muscle to determine the shape of the TMD. a - anterior portion of the muscle; b - middle portion of muscle; c - posterior portion of the muscle.
Another type of painful form of TMD is TMD-related headache. In ICHD-3, beta headache associated with TMD is classified as a secondary cephalalgia and is described as “tension caused by a disorder involving structures in the region of the TMJ” [1]. The first two points are nonspecific criteria confirming the secondary nature of the pain; only point 3 contains characteristics specific to TMD: headache is provoked or aggravated by active movements of the jaw, passive movements in the usual range of jaw mobility and/or during provocative tests with temporomandibular structures, for example, by applying pressure to the TMJ and surrounding masticatory muscles. However, the comments to the diagnostic criteria contain a recommendation from the International Headache Society to use newer and more accurate criteria developed by the International Network Consortium RDC/TMD and the Orofacial Pain Study Group to fully diagnose and clarify the causes of pain associated with TMD.
Differential diagnosis of headache associated with TMD includes other forms of primary and secondary cephalgia. When carrying out differential diagnosis, it is necessary to rely on the known diagnostic criteria for these cephalgia. In the case of strictly unilateral headache, it is necessary to exclude migraine and cervicogenic headache. Patients with migraine are characterized by provocateurs of a painful attack that are not typical for TMD, migraine symptoms accompanying the attack (nausea, vomiting, phono- and photophobia), and often a hereditary history of G.B. To confirm the diagnosis of cervicogenic headache, rotation tests and diagnostic blockades of cervical structures are used [1]. In the case of bilateral localization of pain, it may be difficult to differentiate from tension headache combined with tension in the pericranial muscles. In this case, inspection and palpation shown in Fig. 1-3 are of key importance for diagnosis.
Somewhat less common in neurologist practice are intra-articular forms of TMD. It should be noted that in many cases, the identified intra-articular pathology is combined with the painful form of TMD, and is not isolated.
When there is damage to the TMJ itself, there are several forms of TMD. With various forms of displacement of the intra-articular disc with reduction, different intracapsular sounds are noted during palpation of the joint and movements of the lower jaw: crunching, crackling, clicking. Disc displacement without reduction is usually caused by spasm of the lateral pterygoid muscle [12]. When the disc is displaced without reduction, there is a pronounced limitation in mouth opening and impaired ability to eat. In the case of degenerative disc pathology, a rougher (grinding-like) and longer sound can be noted - crepitus, caused by friction of the damaged intra-articular disc. Locking of the TMJ with the mouth open and the inability to close the mouth without an auxiliary maneuver indicate subluxation of the mandible.
The examination rules for diagnosing the intra-articular form of TMD are shown in Fig. 4. To confirm the diagnosis of various intra-articular forms of TMD, an MRI examination of the joint is necessary.
Rice. 4. Palpation aimed at detecting sounds in the TMJ. a - when opening/closing the mouth; b - lateral movement of the jaw to the right; c - lateral movement of the jaw to the left; d - protrusion of the lower jaw. Palpation is carried out sequentially on each side.
Etiology and pathogenesis of TMD
The etiology of TMD is multifaceted and is a combination of psychological, postural, orthopedic, genetic, biopsychosocial and occlusal factors that disrupt the functional balance in the structures of the TMJ itself and the muscles surrounding it [6, 13, 14].
The view on the pathophysiology of TMD cannot be considered fully formed. In 1934, James Costen first gave a systematic description of this group of diseases, citing malocclusion as the main cause. For many years, it was believed that the cause of myogenic and joint disorders in TMD were malocclusion (occlusal disorders, missing teeth, suboptimal prosthetics, chewing on one side and other causes) and parafunctional activity (night and/or daytime bruxism), which leads to increased load on the TMJ and muscles that provide chewing (temporal, masticatory, medial and lateral pterygoid). Facial and jaw injuries and emotional disorders also played a significant role. In particular, the presence of symptoms of depression doubles the likelihood of developing the arthralgic form of TMD, and anxiety disorders more often accompany myalgia in TMD [15, 16]. Some authors [7] point to the role of orthopedic disorders (for example, short leg syndrome) in the genesis of TMD. During an orthopedic examination, a significant number of patients (66%) reveal asymmetries of the shoulders, shoulder blades, and shortening of one leg, which causes a compensatory change in posture and muscle imbalance throughout the entire spine. The “forward head posture” also has a serious influence on the occurrence of the myogenic form of TMD [17].
However, in recent years, a number of authors have expressed doubts about the exclusive role of dental pathology in the development of TMD. Indicate a frequent combination of TMD and various types of headache. In patients with TMD, the most common primary form of headache is migraine (55.3%), the prevalence of tension-type headache is 30.2% [18]. According to other authors [19], the prevalence of TMD in patients with chronic daily headache is 58.1%.
In recent years, the works of leading Russian and foreign researchers of chronic pain [20-22] have for the first time suggested the possible central causes of TMD, in particular the role of possible dysfunction of pain control systems. Thus, it has been shown that the prevalence of the painful form of TMD in chronic migraine is significantly higher than that in episodic migraine. The authors suggested that pain and myofascial pain syndrome in TMD may be caused by impaired processing of pain impulses in the central nervous system and are not related to peripheral/dental factors.
Treatment
Based on the current understanding of the pathophysiology of TMD, a number of treatment options have been developed. In neurological practice, treatment of TMD includes a wide range of non-drug and pharmacological approaches:
1. Patient education.
Educating patients about the causes and form of TMD and the importance of behavior modification (eg, actively focusing on not clenching teeth) is important. In case of acute pain, it is necessary to recommend a temporary refusal to eat solid foods and open the mouth wide.
2. Nonsteroidal anti-inflammatory drugs
(NSAIDs) are often the first choice drugs and are effective in relieving TMD pain. Among the large group of NSAIDs, the drug nimesulide (Nise) deserves special attention. The difference in clinical efficacy and tolerability of different NSAIDs may be due to different selectivity for COX-1 and COX-2 inhibition. Nimesulide is primarily a COX-2 inhibitor with a wide range of additional effects, which helps explain its specific anti-inflammatory and analgesic activity. More than 200 clinical studies have assessed the effectiveness of nimesulide in a wide range of pain syndromes (tooth extraction and other dental operations, hypertension, back pain, joint pain, dysmenorrhea). In these studies, nimesulide systematically demonstrated a reduction in inflammatory pain that was significantly superior to that of placebo and at least equal to or in some cases more effective than other NSAIDs [23].
The main clinical benefit of nimesulide is the time to onset and duration of pain relief. Compared to other NSAIDs, nimesulide has a faster onset of analgesic action, namely 15 minutes after oral administration [24]. It should also be noted that a rapid onset of action was noted in patients with chronic pain syndrome.
A significant advantage of this drug is the lower relative risk of complications of the upper gastrointestinal tract compared with non-selective NSAIDs due to its predominant effect on COX-2. However, a single dose of nimesulide provided higher efficacy and a faster onset of analgesic action than comparable single doses of selective COX-2 inhibitors such as celecoxib and rofecoxib [25]. When comparing nimesulide with the non-selective NSAID diclofenac, the drug showed comparable efficacy, but better overall tolerability [26].
The overall risk of severe liver reactions associated with NSAID use is low. The incidence of liver injury associated with the use of nimesulide is within the frequency range for other NSAIDs [23].
The use of all NSAIDs is associated with some cardiovascular risk and in patients with hypertension, hypercholesterolemia and cardiovascular disease, all NSAIDs should be used with caution, especially in the elderly. Risks and benefits should be assessed on an individual basis and the lowest effective dose recommended for the shortest possible period of time. Many data indicate that nimesulide demonstrates a low overall risk of cardiovascular events such as myocardial infarction or congestive heart failure [27].
An international panel of experts concluded that, when used appropriately, nimesulide remains an extremely important and safe treatment option for a variety of conditions characterized by acute inflammatory pain due to its rapid onset of analgesic action and proven positive benefit/risk profile [23].
For TMD, Nise is recommended to be used at a dose of 100 mg 2 times a day. The duration of its use, like other NSAIDs, should be limited to the minimum necessary time.
3. Gymnastics
. After applying a cold compress, exercises are performed to stretch the masticatory muscles, then a warm towel must be applied.
4. Cognitive behavioral psychotherapy and biofeedback
communications are also highly efficient.
For chronic TMD, it is recommended:
1. Prescription of the tricyclic antidepressant amitriptyline (up to 75 mg/day). The choice of amitriptyline as a first-line drug is due to the relatively high risk of developing bruxism while taking selective serotonin reuptake inhibitors [28].
2. Referring the patient to a dentist to select a special muscle relaxant splint (especially in the case of night bruxism) and assess the presence and correction of occlusal disorders.
3. In the case of myofascial pain syndrome, it is possible to inject anesthetic into trigger points in the masseter, temporal and pterygoid muscles.
4. Treatment with botulinum toxin type A for the painful form of TMD, which has demonstrated high effectiveness in a large volume of studies [9, 29]. Such therapy can allow not only to achieve long-term and sustainable relaxation of the muscles of the masticatory group and relief of pain associated with myofascial pain syndrome in these muscles, but also temporary remission of nocturnal bruxism, which will reduce the risk of developing an intra-articular form of TMD.
5. Conducting comprehensive treatment of comorbid diseases, in particular depression, anxiety disorders, chronic pain.
6. In case of proven presence of intra-articular form of TMD, impaired jaw function and lack of effect of conservative therapy, the patient should be referred to a maxillofacial surgeon [30].
TMD is considered today to be the most common cause of chronic facial pain not associated with dental disease. It has been shown that facial pain in many cases is caused by hypertonicity and myofascial syndrome in the masticatory muscles without pathological changes in the structures of the joint itself. Since the prevalence of the painful form of TMD exceeds the prevalence of the intra-articular form, most patients can and should receive effective care from a neurologist. To fully diagnose the nature of TMD, one should rely on the DC/TMD diagnostic criteria for clinical use. These criteria are based on history and clinical examination (correct palpation of the temporal and masticatory muscles) and do not necessarily require imaging studies. If typical symptoms of intra-articular pathology (primarily sound) are detected, an MRI of the joint is indicated to confirm the diagnosis.
Currently, TMD is considered a disease with a multifactorial etiology. Myofascial pain syndrome in the muscles of the masticatory group can be considered as a manifestation of a violation of antinociceptive functions, i.e., it is a reflection of central sensitization and a violation of descending pain control.
Treatment of the painful form of TMD at the first stage should be carried out by a neurologist. Recommendations for the treatment of TMD include patient education, NSAIDs, cognitive behavioral therapy, and biofeedback. For chronic pain, it is also possible to prescribe amitriptyline, administer injections of anesthetics and botulinum toxin type A, as well as referral to a dentist and maxillofacial surgeon.
The authors declare no conflict of interest.
Prevention
To minimize the risk of developing a pathological process, it is recommended to follow the following rules:
- promptly treat diseases in which the formation of purulent foci occurs;
- protect yourself from traumatic factors;
- avoid hypothermia;
- promptly treat nasopharyngeal pathologies;
- treat acute infectious processes;
- eliminate dental problems.
To prevent the pathological process from worsening, it is important to seek help from a medical facility as quickly as possible.
Classification
Based on the results of an X-ray examination, in accordance with the diagnosed changes, it is customary to distinguish between two types of arthrosis:
- sclerosing - changes suggest sclerotic changes in bone surfaces, accompanied by a significant narrowing of the gap between the heads of the bones;
- deforming – there is a significant loss of texture and inherent forms of bone tissue, as well as a significant proliferation of osteophytes.
According to their origin, there are two types of pathology:
- primary – forms independently, without previous diseases/damages, mainly in old age;
- secondary - has a close connection with previous trauma, inflammation or metabolic disorders.