12/21/2021
79 475
17 minutes
Co-author, editor and medical expert – Maksimov Alexander Alekseevich.
- Symptomatic treatment
- Rinsing
Many people are familiar with the diagnosis of tonsillitis. This unpleasant disease can take you by surprise and prevent you from leading a normal life. Tonsillitis is a pressing problem today, as it can occur at any age and with various diseases, such as herpes, diphtheria, streptococcal infections, scarlet fever and others. Often tonsillitis (or simply tonsillitis) acts as an independent disease. To understand the diagnosis and begin proper treatment, you need to consult a doctor. Remember that self-medication can lead to complications. What is tonsillitis? And how to cope with this disease? We will consider the answers to these questions below.
Up to contents
Causes of tonsillitis in children
The disease occurs due to the ingress of bacteria or viruses. Tonsillitis is often caused by streptococcus bacteria. The disease is also caused by adenoviruses, influenza and parainfluenza viruses, herpes, etc.
Other reasons:
- staphylococcus, pneumococcus, hemophilus influenzae and other microbial associations;
- enterovirus infection;
- mushrooms;
- parasites – membrane and intracellular (mycoplasma and chlamydia);
- disruption of the process of self-cleaning of lacunae against the background of restructuring of lymphoid tissue and dysbiosis of the respiratory tract;
- a single or multiple history of tonsillitis;
- ARVI, sinusitis, adenoiditis, caries, stomatitis, periodontal disease;
- anatomical features of the pharyngeal part of the lymphatic system - deep and narrow lacunae, adhesions, multiple fissure passages;
- burdened by concomitant diseases - food allergies, perinatal pathologies, rickets, impaired breathing through the nose, intestinal infections and other factors that reduce immunity.
Reasons for appearance
Purulent tonsillitis in a child is of an infectious nature, and is provoked by the increased activity of pathogenic pathogens such as staphylococcus, streptococcus, pneumococcus, diplococcus. When identifying the causative agent of infection, one should not exclude the penetration of influenza, parainfluenza, and adenovirus viruses into the child’s body. Other provoking factors for inflammation of the tonsils are presented below:
- Treatment of sore throat with beets and vinegar
- prolonged hypothermia of the body;
- environmental factor and climate change;
- physical or emotional fatigue;
- decreased immunity;
- diseases of the ENT organs.
Types of disease
- Spicy. Most often, the acute form develops after suffering from acute respiratory viral infection, due to reduced immunity. Source: A.D. Vetrova Acute tonsillitis in children: a pediatrician’s point of view // Pediatric pharmacology, 2014, v. 11, no. 2, pp. 61-64
- Chronic. Occurs after relapses if the patient has not fully recovered. Diseases in the mouth, nose, and structural features of the tonsils contribute to the development of chronic tonsillitis. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248716/ Raja Kalaiarasi, Kalaivani S Subramanian, Chellappa Vijayakumar and Ramakrishnan Venkataramanan Microbiological Profile of Chronic Tonsillitis in the Pediatric Age Group // Cureus. 2022 Sep; 10(9): e3343
Classification
Acute tonsillitis, well known to us as tonsillitis. She may be
- catarrhal
- follicular
- lacunar
- fibrinous
- phlegmonous
- herpetic
- ulcerative membranous
If there is acute tonsillitis, then there is also a chronic one, which, in turn, can be simple (manifested by local symptoms) and toxic-allergic (occurs with lymphadenitis, damage to the cardiovascular system, joints, kidneys, skin). It can be compensated (no recurrent sore throats, the barrier function of the tonsils is not impaired) and decompensated (the child is bothered by frequent sore throats, complications from the sinuses, ear, kidneys, and heart are possible).
Tonsillitis can be an independent disease, then it is called primary. Sometimes inflammation of the tonsils is a consequence of another infection, for example, with diphtheria, scarlet fever, measles or blood diseases.
Symptoms of the disease
The main symptoms of tonsillitis in children that require immediate treatment are:
- pain when swallowing and yawning;
- heat;
- general intoxication of the body (weakness, decreased appetite, headaches);
- swelling and redness of the tonsils;
- formation of whitish or yellowish plaque on the tonsils;
- blisters, sores on the throat;
- loss of voice, hoarseness;
- bad breath;
- enlarged and painful lymph nodes (this sign can indicate not only tonsillitis, it accompanies many other diseases in children).
Symptoms of tonsillitis
Clinical manifestations are quite varied and depend on the type of tonsillitis. The disease debuts acutely, against the background of hypothermia or stress. First there is a sore throat. It may intensify when swallowing, after smoking, or eating hard, dry foods. There is a cough, a feeling of a foreign body in the throat, rawness, soreness in the throat. The body temperature rises, the patient feels weak, tired, unwell, quickly gets tired, and there is pain in the joints and muscles. Upon examination, the doctor reveals enlarged and painful submandibular and cervical lymph nodes; the pharyngoscopic picture varies from hyperemia of the tonsils to friability, purulent changes (lacunae and follicles), and enlarged tonsils. The mucous membrane becomes swollen. In the presence of purulent plaque, a characteristic unpleasant odor from the mouth may appear.
Treatment for tonsillitis depends on its type and cause. Let's look at it in detail:
Etiotropic treatment (impact on the cause of the disease) depends on the causative agent of the disease. If a sore throat is bacterial in nature and if there are indications, antibiotics are used, which are prescribed by a doctor. Self-treatment of tonsillitis with antibiotics is not recommended, since an insufficient dose or the wrong choice of drug can lead to the development of resistance (persistence) in the microorganism, as well as to complications of angina (for example, peritonsillar, retropharyngeal abscess, diphtheria croup in children, acquired heart defects). For a viral infection, symptomatic therapy is prescribed, as the patient’s general condition remains satisfactory. Physiotherapy methods are also effective: ultraviolet irradiation increases the barrier function, the resistance of the tonsils, improves, stimulates local and general immunity, and has an antimicrobial effect. Laser treatment of tonsillitis in the submandibular area is carried out daily, in a course. The therapeutic effect is achieved by dilating small blood vessels and increasing blood circulation in the area of inflammation1.
Symptomatic treatment
Anti-inflammatory drugs (paracetamol, ibuprofen, aspirin) have proven themselves well in the treatment of tonsillitis. They reduce swelling, inflammation, and as a result, pain. Antihistamines (Zyrtec, Tavegil) and analgesics are also used. For the duration of treatment, smoking, drinking alcohol, and spicy and hot foods are excluded. A gentle diet and bed rest are prescribed for 5-7 days.
If the patient’s general condition does not suffer, we can limit ourselves to the use of local means of treating tonsillitis.
Local treatment consists of prescribing medications that have an antiseptic, anti-inflammatory, and analgesic effect2. Drugs for local therapy should not only relieve sore throat, but also have a wide spectrum of antibacterial activity, low allergenicity, and be non-toxic.
Hexoral ® has all these properties. The drug is active against a wide range of gram-positive bacteria, as well as pathogenic fungi of the genus Candida; the drug Hexoral ® can have its effect in the treatment of infections caused by Pseudomonas aeruginosa and Proteus. At a concentration of 100 mg/ml, the drug inhibits the growth of most bacterial strains. Hexetidine, being the active ingredient of the drug Hexoral ®, also has an anesthetic effect on the mucous membrane3. The variety of dosage forms of Hexoral ® makes its use accessible to the whole family. Hexoral ® spray is a convenient, effective and proven form for the treatment of tonsillitis in adults and children from 3 years of age. The Hexoral® line also includes a rinse solution (from 3 years old), Hexoral® tabs tablets (from 4 years old), Hexoral® tabs Classic (from 6 years old), Hexoral® tabs Extra (from 12 years old) years). In the form of a rinse solution, lozenges and sprays, the medicine is convenient to use, which makes patient adherence to treatment high.
In all cases of tonsillitis, it is necessary to consult a doctor, so that only a specialist can prescribe adequate treatment and prevent complications.
Surgery
Tonsillectomy is the removal of tonsil tissue and the underlying capsule. It is used in cases of unsuccessful conservative therapy, in the presence of a focus of chronic infection in the tonsils. A tonsillectomy is performed by an ENT doctor. Before the operation, you should consult with a therapist, do blood and urine tests, perform an ECG, and a chest x-ray. If there are concomitant diseases, undergo additional examination by specialized specialists.
Tonsillectomy is usually performed under local anesthesia with the patient sitting. Local anesthesia is performed, and then the tonsils are removed along with the capsule. The operation does not last long, about 10 minutes, complications are quite rare. Indications for surgical treatment are chronic persistent inflammation of the palatine tonsils in the stage of decompensation, frequent exacerbations of chronic tonsillitis, purulent complications in the form of abscesses and phlegmon.
Contraindications for tonsillectomy are: blood diseases (hemorrhagic diathesis), neuropsychiatric diseases in the stage of decompensation, which can interfere with the course of the operation and compliance with the postoperative regimen, open form of respiratory tuberculosis, cardiac, renal failure, severe diabetes mellitus. In each specific case, the issue of performing an operation is decided individually1.
Cryotherapy is a gentle method of semi-surgical treatment. Cryotonsillotomy - exposure to the tonsils with a special applicator (cryoprobe), in a closed system of which liquid nitrogen circulates at a temperature of -196 °C4. Areas of chronic inflammation where the tonsil no longer performs its functions are removed. Since cryotherapy is painless and bloodless, it is the method of choice for weakened patients, patients with blood diseases and those for whom surgical treatment is contraindicated (allergy to novocaine, severe diabetes mellitus, uncontrolled hypertension, severe heart failure, renal failure, hemophilia) and also in children. After cryodestruction, the body recovers more quickly and the patient returns to normal life. However, along with the advantages, the cryosurgical method has a number of disadvantages: several stages are assumed over 1.5 months, but in some cases it is not possible to achieve complete removal of tonsil tissue.
Contraindications to cryotherapy: decompensation of diabetes mellitus, some oncological diseases, acute myocardial infarction, high-grade heart failure, severe hypertension.
Up to contents
Diagnostic methods
During the consultation, the doctor will examine the patient’s throat and palpate the lymph nodes. The examination should be carried out by a pediatrician and pediatric ENT specialist. In case of decompensation of the chronic form, the child requires consultation with a pediatric cardiologist, rheumatologist, nephrologist, because tonsillitis can cause concomitant diseases. To rule out pockets of infection in the oral cavity, the child should be examined by a dentist. Laboratory and instrumental studies are also prescribed:
- blood and urine tests;
- pharyngoscopy;
- blood test to determine C-reactive protein;
- definition of ASL-O;
- bacterial culture from the pharynx for flora.
If there are difficulties in making a diagnosis, additional studies may be required - ECG, x-ray of the sinuses, etc.
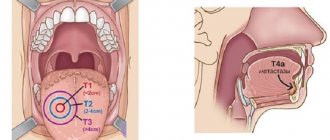
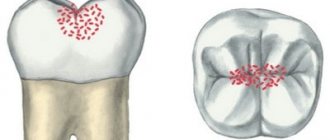
Development mechanisms
The palatine tonsils are an important organ of the immune system; they form a barrier against foreign microorganisms and dust particles entering the respiratory tract. This must be remembered when deciding on surgical treatment of tonsillitis. In the thickness of the organ there are crypts, which are convoluted canals; they open to the surface with an exit hole called a lacuna. The wider the lacuna, the better microorganisms and dust particles are removed from the tonsils and the less likely it is to develop inflammation.
On the surface of the organ there is always a non-pathogenic, conditionally pathogenic flora; immunoglobulins and interferon are produced in the tissues. When the balance shifts towards the former, the tonsils turn from protectors into a source of constant infection. In this case, a sore throat develops, and with untreated acute tonsillitis, the disease becomes chronic. Based on the above, it is easy to conclude that careful and complete treatment of acute tonsillitis is necessary.
Treatment of tonsillitis in children
With properly selected medications, treatment of tonsillitis in a child takes about a week. The patient is prescribed bed rest, plenty of fluids and a gentle diet, excluding spicy and fatty foods. Medicines are selected according to the type of tonsillitis, accompanying symptoms, and the age of the child. Medicines should only be prescribed by a doctor.
The treatment program includes:
- painkillers;
- washing and rinsing;
- sprays and lozenges;
- physiotherapy. Source: T.V. Spichak Diagnosis and treatment of tonsillitis in children from the perspective of evidence-based medicine // Issues of modern pediatrics, 2010, vol. 9, no. 2, pp. 130-135
Antibiotics are prescribed to children only in severe cases, as they cause side effects (abdominal pain, diarrhea, etc.).
Removal of the tonsils (tonsillectomy) is used in exceptional cases, if frequent relapses of the disease are observed, conservative treatment is ineffective, and complications from internal organs are identified.
In case of exacerbation of the chronic form of tonsillitis, the child requires bed rest, diet correction with the exception of fatty, fried, smoked, sweet foods, as well as drug therapy, which includes antibiotics, vitamins, desensitizing drugs, and immunomodulators.
Necessary:
- wash the lacunae of the palatine tonsils with antiseptics;
- treat the back wall of the pharynx and tonsils with solutions of fucorcin, Lugol;
- the child should regularly gargle with antiseptics and herbal decoctions.
You also need to do inhalations, use antiseptic aerosols, and take antimicrobial lozenges.
Physiotherapy may be prescribed :
- Ural Federal District;
- UHF;
- microwave;
- ultraphonophoresis;
- laser therapy.
Complications of the disease:
- descent of purulent infection into the heart sac;
- abscess;
- bleeding from the tonsils;
- eustacheitis;
- otitis;
- purulent inflammation;
- swelling of the larynx with the development of asphyxia, which can be fatal.
Treatment for sore throat
Treatment is carried out mainly at home. Moreover, it is necessary to adhere to bed rest. A sick child is hospitalized when he is less than 3 years old, his high fever (39°-40°) does not subside, he has difficulty breathing, swallowing food and liquids, an abscess is detected on the tonsils, and there is a real threat of complications.
Drug treatment
In order to prevent complications of purulent tonsillitis in a child, treatment is carried out with antibiotics, local agents for the inflamed tonsils, and drugs to eliminate painful symptoms.
Treatment with antibiotics
Penicillin-based drugs (phenoxymethylpenicillin, amoxicillin) are used. If you are allergic to penicillin or need re-treatment with antibiotics due to recurrent sore throat, use antibacterial agents of a different group (macrolides), such as sumamed, azithromycin, erythromycin.
In severe forms of the disease or when complications occur, even stronger antibiotics (cephalosporins) are used for treatment.
Treatment with topical drugs
To speed up the cleansing of the surface of the tonsils from pus, gargle with antiseptic solutions of miramistin or chlorhexidine. Sprays that have an antiseptic effect and contain an antibiotic are used: for example, hexoral, bioparox.
To eliminate pain and sore throat with purulent sore throat in children, you can use lozenges (strepsils, falimint). They contain components with analgesic, anti-inflammatory and antiseptic effects.
Warning: If the child does not yet know how to gargle and suck tablets, treatment can only be carried out with sprays. It is recommended to give him slightly warm tea to disinfect the oral cavity.
Clinical recommendations for disease prevention
The main methods of preventing tonsillitis in children are compliance with sanitary and hygienic measures (avoiding contact with patients and their things, washing hands, using a scarf and hand sanitizers) and strengthening the immune system (hardening, playing sports, etc.).
Tonsillitis is a common disease in children and adults, which without proper treatment can become chronic. If you notice symptoms of illness in your child, immediately contact the children's medical department.
Sources:
- HELL. Vetrova. Acute tonsillitis in children: a pediatrician’s point of view // Pediatric pharmacology, 2014, vol. 11, no. 2, pp. 61-64.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248716/ Raja Kalaiarasi, Kalaivani S Subramanian, Chellappa Vijayakumar and Ramakrishnan Venkataramanan. Microbiological Profile of Chronic Tonsillitis in the Pediatric Age Group // Cureus. 2022 Sep; 10(9): e3343.
- T.V. Spichak. Diagnosis and treatment of tonsillitis in children from the standpoint of evidence-based medicine // Issues of modern pediatrics, 2010, vol. 9, no. 2, pp. 130-135.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Lacunar tonsillitis
Regional lymphadenitis develops. On palpation, the submandibular, anterior ear, and cervical lymph nodes are enlarged, painful, dense, and not fused to each other.
A clinical blood test is characterized by leukocytosis - an increase in the level of leukocytes to 15*109/l and higher, the appearance of a large number of immature forms of leukocytes and an increase in ESR to 40-50 mm/hour.
Treatment
As in most cases, treatment can be conservative or surgical.
Surgical treatment includes tonsillectomy (complete removal of the tonsils) and tonsillotomy (partial removal of the tonsils).
Conservative therapy
- antibacterial, protected aminopenicillins are more often used because many bacterial strains have β-lactamase activity. Antibiotics must be taken in full, despite the reduction in symptoms; ignoring this rule often leads to the development of chronic tonsillitis
- desensitizing, relieves swelling of the tonsils
- immunostimulating, it is very important to help the immune system fight infection
- painkiller
- diet therapy, spicy, fried foods must be avoided. Stop using spices
- physiotherapy (KUF)
A necessary remedy for combating chronic tonsillitis is local rinsing of the tonsils with both antiseptic solutions and antibiotics. Miramistin and Dioxidin are more often used as solutions. You can do this at home, but not all “plugs” can be washed out, and it is these deep-seated accumulations of microorganisms that cause tonsillitis to become chronic. To clean the lacunae of the palatine tonsils as completely as possible, the ENT specialist performs rinsing of the tonsils.
This method allows you to:
- effectively bring chronic tonsillitis into stable remission
- avoid the development of dysbiosis and fungal infection on the surface of the tonsils
- reduce the risk of needing surgery
- exclude trauma to the tonsils
- treat tonsillitis painlessly
Rinsing is performed using a syringe or a vacuum rinsing apparatus. In the first case, the antiseptic solution is drawn into a syringe and flowed through a special nozzle to the tonsils. In the second case, the solution is supplied and sucked out using the device, and the contents of the lacunae are removed along a pressure gradient. This allows you to penetrate deep into the tissues of the tonsils. In our clinic, your baby will have tonsils washed and a course of physiotherapy, which will allow you to forget about tonsillitis for a long time and avoid surgery. Washing is usually carried out in a course of 5-10 procedures, twice a year or as needed.
To prevent tonsillitis, it is necessary to harden the baby and avoid excessively salty, spicy or hot foods. Follow the rules of home hygiene. It is important to treat acute tonsillitis on time, and most importantly, in full.
Diagnosis of pharyngitis
Acute pharyngitis can be determined by patient complaints and examination of the oropharynx (pharyngoscopy).
Objective symptoms of pharyngitis, which are assessed by a doctor when examining the throat:
- swelling and hyperemia (redness) of the pharyngeal mucosa
- purulent or mucopurulent plaque on the walls of the pharyngeal mucosa
- the presence of inflammation in the arches, tonsils, orifices of the auditory tubes
- the presence of bright red tubercles on the back surface of the pharynx and on the side - hypertrophied (enlarged) lymphoid follicles
- thinning of the mucosa with areas of exfoliating epithelium, crusts and viscous mucus (atrophic pharyngitis)
Based on this, the doctor can make not only a diagnosis of pharyngitis, but also suggest its cause (viral inflammation, fungal infection, etc.).
Despite the fact that 70% of acute pharyngitis is a viral disease, sometimes it is necessary to exclude a bacterial cause. This is very important for further treatment tactics and prevention of complications. To do this, you should conduct a rapid test to exclude the streptococcal nature of pharyngitis.
In some cases, with fever, long-term complaints, or a temperature exceeding 3 days, it is also necessary to take a general blood test to understand the cause of acute pharyngitis.
How common is pharyngitis?
Pharyngitis, like a common ARVI (viral infection), occurs quite often. The incidence rate increases during the season from September to May, with a peak in February and March. A decrease in the incidence of pharyngitis by 3-5 times is observed in the summer months.10,11
Acute pharyngitis occurs more often in childhood than in adults. Children under 5 years of age suffer viral infections, including pharyngitis, 6-8 times a year.8,9
In the first year of visiting a preschool institution, the incidence of the disease is 10-15% higher than in children at home. But, unfortunately, “home” children subsequently get sick more often at school age.
Prevention of pharyngitis
To prevent pharyngitis, it is recommended:
- avoid hypothermia and dress appropriately for the weather
- avoid contact with tobacco and chemical irritants
- carry out frequent ventilation of working and living spaces
- walk outdoors more often. Walking will help strengthen the body's defenses in the fight against pharyngitis.
- don't drink ice water
- do not share food and cutlery, cups
- avoid crowded places and, if possible, stay in them for as little time as possible
- use disinfectants, including in public places,
- transport, etc.
- wash your hands often
ICD - pharyngitis:
- J02 - acute pharyngitis
- J02.0 - streptococcal pharyngitis
- J02.8 - acute pharyngitis caused by other specified pathogens
- J02.9 - acute pharyngitis, unspecified
- J31.2 - chronic pharyngitis
- J31.1 - chronic nasopharyngitis
Pharyngitis is rarely isolated as a separate disease; the diagnosis is usually acute respiratory viral disease (ARVI).
ARVI is a general name; the doctor usually specifies how exactly ARVI manifests itself.
This may be rhinitis (runny nose), pharyngitis (red throat), nasopharyngitis (inflammation of the nose and throat), etc.1,2
It is important not to confuse pharyngitis with tonsillitis.
To do this, let's understand the structure of the pharynx and oral cavity.
Causes of pharyngitis and tonsillitis
Etiology (origin, cause) of pharyngitis. In 70-90% of cases, pharyngitis is caused by viruses. Pharyngitis can also be caused by bacteria, fungi, allergies, injuries, and exposure to irritating factors.
The most common viruses are rhinoviruses, adenoviruses, influenza, parainfluenza, enteroviruses, Coxsackie A, coronaviruses, a group of herpes viruses (Epstein-Barr virus, cytomegalovirus, HSV).12
There are pharyngitis, which are classified as a separate diagnosis depending on the pathogen, for example streptococcal pharyngitis ICD J02.0