A. V. KuzinCandidate of Medical Sciences, Doctor - Dental Surgeon, Department of Surgical Dentistry, Federal State Budgetary Institution Central Research Institute of Dentistry and Maxillofacial Surgery, Ministry of Health of the Russian Federation (Moscow)
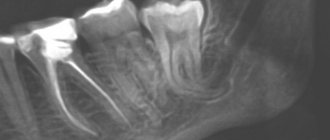
Recently, there has been an increase in the number of young and middle-aged patients visiting a dental surgeon for the removal of impacted third molars. This is not just about providing them with emergency care for pericoronitis. Quite often, the patient is referred for removal of intact impacted teeth for orthodontic reasons. Clinical symptoms include: close position of teeth “bouquet symptom”, lack of space in the retromolar fossa for full eruption of the third molar, lack of dynamics in orthodontic tooth movement, relapse of bite pathology after orthodontic treatment.
As a rule, such teeth are located inside the alveolar part and body of the lower jaw at different angles to the second painter standing in front. In most cases, a close relationship between the roots of the impacted molar and the mandibular canal is observed. In some cases, there is a risk of iatrogenic injury to the neurovascular bundle when tooth roots are dislocated. Violation of the integrity of the canal and nerve injury leads to a persistent disorder of sensitivity of the lower lip, which can last from several days to several months. Externally, facial expressions and the smile line are not deformed, but the constant feeling of “numbness” of half the chin and lower lip from the side of the extracted tooth causes significant discomfort to the patient.
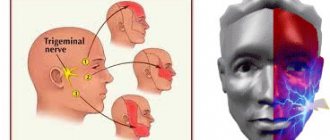
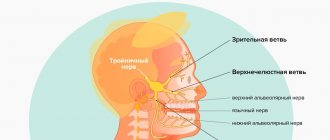
Anatomy and functions of the trigeminal nerve
The trigeminal nerve belongs to the class of mixed nerves, including both sensory and motor fibers.
It is the largest of the 12 cranial nerves. This name of the nerve is due to the presence of three branches - the orbital, maxillary and mandibular nerves. When one of the branches of the trigeminal nerve is damaged, a sensitivity disorder occurs in the area of innervation. When the trigeminal nerve root is damaged, sensitivity disorder is observed in the areas of innervation of all three branches.
Can a filled tooth hurt and react to heat without nerves?
With proper depulpation, the organ should lose any sensitivity, including to temperature changes. Therefore, the occurrence of a reaction to thermal effects probably indicates the incompetence of the doctor, who made a mistake and did not remove all the nerve endings. But sometimes carelessness has nothing to do with it; the cause may be a hidden channel that is not even visible on an x-ray. And another option in which a reaction to hot manifests itself is proximity to a sick neighbor in the dentition.
Causes of trigeminal neuralgia
Trigeminal neuralgia occurs due to various reasons, among which the following are common:
- Compression (squeezing) of the trigeminal nerve by vessels or neoplasms.
- Pathologies of the nervous system (multiple sclerosis, meningitis).
- Malocclusion.
- Inflammatory pathologies of the nasal sinuses.
- Injuries.
- Hypothermia.
- Viral or bacterial infections of the upper respiratory tract.
Damage to the trigeminal nerve after tooth extraction
There is also trigeminal neuralgia of odontogenic origin. In this case, the pathology is caused by diseases of the teeth, jaws or oral cavity. Sometimes such complications arise after tooth extraction.
You can suspect damage to the facial nerve after tooth extraction if pain occurs in the eye area, temporal area or nose. In this case, the trigger for pain is harmless procedures or events, for example, a gust of wind or brushing your teeth.
Important! Don't be afraid to have teeth removed when it is medically necessary. Damage to the facial nerve during tooth extraction is extremely rare. But complications in the absence of proper dental treatment occur much more often. Therefore, it is important to trust an experienced doctor, with whom the likelihood of complications is minimized.
There are two main reasons why the trigeminal nerve is damaged due to tooth extraction:
- Diagnostic error . Sometimes neuralgia is so successfully disguised as a toothache that the doctor makes an erroneous diagnosis. Instead of treating trigeminal neuralgia, the patient is treated or the tooth is removed. At the same time, the pain intensifies.
- Difficulties in dental treatment . Sometimes, when treating severe stages of pulpitis, the nerve is often injured, which causes neuralgic symptoms.
Complication after implantation
Among the complications encountered in implant dentistry is damage to the trigeminal nerve. In this case, the nerve fibers are affected mechanically (during the procedure), due to the inflammatory process or against the background of an infectious complication.
Damage to the trigeminal nerve during implantation can occur at various stages of the procedure, starting with anesthesia. Careful diagnostics using computed tomography, as well as surgical templates, will minimize the risks of complications in implantology.
Complications from the trigeminal nerve also occur with an incorrectly selected implant, when the risk of injury to nerve fibers increases. Increased pressure on the implant during installation is also fraught with damage to the trigeminal nerve.
Important! According to statistics, the likelihood of complications from the trigeminal nerve during implantation is less than 3%. At the Center of Israeli Dentistry this figure is even lower. In this case, an experienced team of doctors and careful preparation for the implantation procedure can minimize the likelihood of complications. Therefore, our patients do not need to worry about the consequences.
Symptoms of the disease
Symptoms of the pathology include:
- Severe pain in the face . Often the pain syndrome covers the area of the upper and lower jaw. Often this type of pain misleads a person, masquerading as toothache. However, after dental treatment the pain does not go away.
- Facial muscle spasms and changes in skin sensitivity . The spasms cause the person to have difficulty communicating or chewing.
- Facial asymmetry . In particular, the asymmetry is clearly visible when talking or smiling.
- Shooting pain attacks.
Concomitant symptoms of trigeminal neuralgia include increased salivation, insomnia, anxiety, changes in taste, local or general increase in body temperature.
Prevention
Prevention measures:
- balanced diet;
- limiting alcohol consumption, quitting smoking, reducing factors that lead to intoxication of the body;
- active sports;
- do not overcool;
- increase stress resistance;
- avoid injury;
- timely treatment of respiratory and infectious diseases;
- preventive examination at the dentist several times a year, dental treatment;
- timely contact a neurologist if pain occurs.
How to treat trigeminal neuralgia
Treatment of this pathology is carried out by conservative and/or surgical methods. Preference is given to conservative therapy, and surgery is used in extreme cases when medications and non-drug methods do not bring the desired result.
The treatment regimen for the trigeminal nerve is selected taking into account diagnostic parameters. Doctors also take into account the patient’s health and condition. The main goal of therapeutic measures for this pathology is to eliminate pain and prevent relapses.
Conservative treatment
Conservative therapy for neuralgia boils down to taking medications, as well as physiotherapeutic procedures. The first drugs for trigeminal neuralgia began to be used at the beginning of the last century. The most popular was phenytoin. However, since the 60s, carbamazepine began to be used for these purposes. When using this drug, pain relief can be achieved in 70-75% of cases.
Drug therapy
Today, three types of medications are used for this pathology:
- Anticonvulsants are medications that eliminate pain and dull the hypersensitivity of facial nerve fibers to irritating factors. Anticonvulsants are used for epileptic seizures to relieve muscle cramps. However, they are also effective for neuralgia.
- Antispasmodics are medications that help relax smooth muscles. Thus, antispasmodics relieve secondary pain syndrome.
- Neuroprotectors are drugs that have a protective effect on nerve fibers and cells.
Let's look at some drugs for the treatment of trigeminal neuralgia:
- Phenytoin . Today this drug is used for exacerbations. Prescribed by intravenous injection.
- Baclofen . This medicine belongs to the group of muscle relaxants.
- Valproic acid preparations. Prescribed both in tablet form and in the form of intravenous injections.
- Tizanidine . It is a centrally acting muscle relaxant. For neuralgia, it is prescribed orally.
- Vitamins . For neuralgia, as well as other pathologies of the nervous system, B vitamins are prescribed. These vitamins take part in the metabolic processes of nerve cells, contributing to the speedy restoration of the functions of nerve cells.
As practice shows, painkillers for trigeminal neuralgia are ineffective. Taking analgesics for this pathology is also undesirable for the reason that the patient may experience severe headaches while taking them. This is due to the patient’s expectation of quick pain relief, which is why they may be taken excessively. Against the background of overdose, headaches often develop, which are called abuse headaches.
Physiotherapeutic methods for treating trigeminal neuralgia
Physiotherapy is a complementary therapeutic component that promotes the rapid restoration of nerve fibers. For neuralgic disorders, the following physiotherapeutic techniques are often used:
- Magnetotherapy is a technique that has a stimulating effect on blood microcirculation in the target area. In addition, the magnetic field created during magnetic therapy has analgesic and muscle relaxant effects. Muscle tension is relieved, which improves the appearance of the face.
- Ultrahigh frequency therapy (UHF) is a procedure that activates normal neuronal responses to external stimuli. In addition, UHF also has a neuroprotective effect. It has been established that UHF courses help eliminate the inflammatory process and reduce pain.
- Laser therapy is a method of physiotherapeutic treatment that improves microcirculation and also promotes the restoration of nerve tissue. In addition, laser radiation of a certain wavelength helps eliminate spasms, pain and inflammation.
- Diadynamic currents (DCT) is a procedure that improves blood circulation in the target area. DDT also improves lymph flow and local defense mechanisms.
Surgery
If conservative therapy is ineffective, then trigeminal neuralgia can be treated with surgery. The essence of surgery is to remove the structure that is compressing the nerve. Often it is the vessel that is exerting compression. In other cases, they resort to removing the nerve to relieve the patient from pain and inflammation.
Surgeries for trigeminal neuralgia are often minimally invasive. These are interventions through small punctures. Such operations are not accompanied by heavy blood loss, and after them the patient recovers much faster. In some cases, stereotactic radiosurgery is also used instead of “classical” surgery. In this case, the removal of target structures is carried out by a beam of high-energy radio waves.
How to treat trigeminal neuralgia at home
Doctors strongly discourage self-medication. This is how patients waste valuable time. Often people seek help with advanced forms of damage to the trigeminal nerve, which requires radical (surgical) interventions.
What happens after nerve damage?
The interaction between peripheral sensory nerves and the central nervous system is extremely complex. It has been proven that minor trauma such as compression, concussion, contusion or pinching can only lead to numbness, but more serious trauma (chemical burn, partial or complete anatomical break) can lead to dysesthesia and/or neuropathic pain, which causes constant discomfort in patients (especially at night) and affects their quality of life.
- After damage to the fibers of the inferior alveolar nerve, degeneration develops within just a few minutes from the entire site of damage: retrograde towards the central nervous system and Wallerian towards the periphery.
- With acute compression, the axoplasmic flow is immediately disrupted, which will lead to a decrease in membrane excitability. If the compression is not removed = chronic compression, the development of axolysis and Wallerian degeneration begins, which in turn will lead to the development of fibrosis, the formation of neuroma and the progression of neuropathy.
- Even if the nerve fibers are partially interrupted, the possibility of spontaneous regeneration of the nerve remains due to the ingrowth of the axons of the terminal sections of its central segment into the peripheral section, provided that the implant is immediately removed. Between the interrupted nerve fibers, a linear array of Schwann cells is preserved, which significantly increases the nerve growth factor. In addition, the work of the gene encoding receptor mRNA is significantly activated and nerve regeneration is activated. These defense mechanisms and repair reactions can be completed within 2 to 3 weeks. This way, the nerve can reconnect fairly quickly unless there is severe neuropathy or complete rupture.
Although regenerative repair and nerve reconnection will be observed histologically, function is not completely restored. Reconnecting (reconnecting) the nerve does not mean healing, and under certain conditions can cause pain in patients.
The inferior alveolar nerve is a mixed nerve and is responsible for pain, touch, heat, cold, and pressure, although the mechanism of each sensation is different. An analogy can be drawn with an underground network of pipes in a big city, where gas, electricity, telephone, water and sewage are transported, but each pipe is separate and along its own route. If the nerve networks are damaged, the insulation of the structure is compromised, and when regeneration occurs, adjacent nerve fibers may be accidentally connected to each other. This means that impulses from peripheral nerves can be transmitted to the wrong destination, and from there to the central nervous system. If we take the pipeline analogy, it is as if groundwater and electrical cables severed by an earthquake were cross-connected.
Rice. 8. Inferior alveolar nerve. Mixed sensitivity. Each fiber is responsible for its own type of sensitivity.
This inappropriate connection is called “ ephapsia ” and was proven in laboratory animals back in the 70s of the last century. https://www.ncbi.nlm.nih.gov/pubmed/224343
Thus , after injury, nerve function is never completely restored, even if histological nerve regeneration is completed through active repair.
Consider a case where nerve fibers designed to convey the sensation of cold accidentally become associated with heat fibers, which can compromise the patient's ability to respond to changes in temperature. There are countless numbers of nerve fibers, so injury to any particular nerve can result in connections to any number of other nerves depending on the severity of the injury. A large number of incorrect connections of nerve fibers leads to the formation of neuroma.
Neuromas often generate spontaneous discharge. This electrical impulse causes dysesthesia, and such patients usually complain of numbness, tingling or goosebumps on the skin. https://www.joms.org/article/0278-2391(90)90385-F/pdf
Thus, the healing of a damaged nerve is an incredibly complex process, which is not limited only to the site of injury, but involves the entire system from the periphery to the central nervous system, in contrast to the healing processes of the mucosa or bone. Regressive changes in axons and myelin sheath, as well as nerve regeneration, affect all neurons not only histologically, but also molecularly and electrophysiologically. The emerging ephaps
creates a contact area in which excitation from one cell to another is transmitted through electric current without the participation of mediators.
Rice. 9. Cross-excitation of adjacent fibers of cold and hot sensitivity due to ephaptic transmission of electrical impulses. It is possible for fibers of different diameters to interact (eg, cold and pain sensory fibers), with the signal propagating in both directions, which underlies stimulus-dependent pain symptoms and explains the abnormal perception of non-noxious stimulation in allodynia and hyperpathia.
Dental restoration for neuralgia
Some patients have to deal with several problems at once. For example, restoration of teeth against the background of neuralgia. In this situation, it is important to understand the nuances in order to understand the correct algorithm of actions.
The treatment process for damage to the trigeminal nerve is long. The patient will have to work for a full recovery. In particular, requirements are also imposed on dentures if the patient does not have his own teeth. This is due to the need to maintain optimal condition of the masticatory apparatus. Indeed, if facial expressions are impaired (which is accompanied by neuralgia), the chewing process is also disrupted. The denture must be made of high-quality, high-strength materials. It should not cause discomfort to the patient, for example, falling out of the mouth.
If the patient is faced with the need to restore teeth due to neuralgia, then in the acute stage of the disease, restoration work should be abandoned for at least 3 weeks. If during this time the problem has been resolved, then you can contact the dentist with a question about restoring the dentition. As for the types of prosthetics for neuralgia, if possible, the patient is recommended to have implantation. Removable dentures, due to their size and care features, have a number of disadvantages compared to fixed ones.
Remember that in any situation, thanks to modern advances in dentistry, you can find a way out. The team of doctors at the Center for Israeli Dentistry will create a competent treatment plan that is optimal for each patient.