According to statistics, the inferior alveolar nerve (IAN) suffers quite often during implantation.
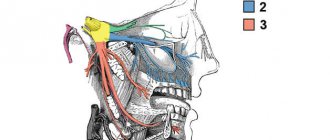
The nerve passing in close proximity to the inferior alveolar process is part of the trigeminal facial nerve, which is responsible for the sensitivity of the facial muscles. Disruption of this nerve during implantation 15-20 years ago was considered a common phenomenon. However, in modern dentistry, the equipment used makes it possible to reduce the risk of damage to the NAS.
Statistics say that only 3% of patients experience a postoperative complication in the form of disruption of the lower branch of the facial nerve. But dental practitioners are sure: more than 30% of people become victims of neuropathy, while about 15% of patients remain with this diagnosis forever.
Trigeminal and facial neuralgia
Neuralgia is a disease in which damage or compression of the trigeminal nerve and/or its branches occurs. This causes a sharp piercing pain that occurs suddenly and brings physical and psychological discomfort to the patient. Despite the fact that the term “neuralgia” can be literally translated as “nerve pain,” the matter is not limited to pain. Trigeminal and facial neuralgia are radically different in symptoms. The facial nerve contains mostly motor fibers, so neuralgia leads to dysfunction of the facial muscles (the degree depends on the severity of the disease), and can also cause lacrimation, dry eyes and partial loss of taste. Pain in facial neuralgia is usually concentrated in the area of the parotid gland (the patient complains that the pain radiates to the ear), but there may be no pain at all. It is because of the lack of pain that some experts use the term “neuropathy” when talking about damage to the facial nerve. With the trigeminal nerve it’s exactly the opposite, since it contains many sensory fibers.
Classification and diagnosis of pathology
Facial nerve injuries are divided into the following types:
- neuropraxia (cured in 3-5 weeks);
- axonotmesis (moderate nerve damage, requiring up to six months of therapeutic treatment);
- neurotmesis (irreversible changes in the structure of nerve fibers. Cannot be treated with medication. Surgical intervention is required).
This neurological pathology is diagnosed using two methods:
- mechanoceptive (brush test - the patient is carried out on the lip, and the patient says the direction of movement and irritation with two points - a device resembling a mathematical compass is applied to the lower part of the face. In this case, the distance between the legs of the device is constantly increasing. As soon as the patient stops feeling each injection separately, the result is recorded and the degree of nerve damage is determined);
- nociceptive (pin prick, temperature test).
Taste buds are tested by dipping a cotton swab in salty or sweet water.
Treatment
Pain in the area of the inferior branch of the trigeminal nerve requires the use of 3 treatment methods.
Drug therapy. The doctor prescribes blockers and painkillers to reduce symptoms. The dentist will also recommend anti-inflammatory therapy. This treatment usually lasts 5-7 days.
Removing the artificial root. 1-1.5 days after implantation of the rod (if symptoms occur), dentists recommend immediately removing the implant, since such a decision increases the chances of a favorable outcome of therapy. Further treatment is carried out with medication.
Surgical intervention. Indications for a radical method are considered to be the failure of removal of the implant and treatment with medications.
Important! Removing the implant is not always the key to successful treatment of the nerve, but this action increases the chances of a quick recovery and reduces the risk of tumor formation in the area of the nerve bundle.
Treatment tactics are agreed upon with the patient, who signs consent for the operation.
Predictions and prevention
| Click to sign up for a FREE consultation |
Neuropraxia and axonotmesis are quite treatable. Statistics show that more than half of patients completely cure the disease. With neurotmesis, complete recovery does not occur.
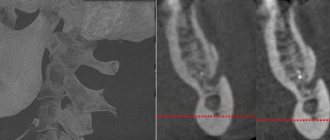
Dentists call the main preventive measure a comprehensive study of the performance of the dental system before implantation. At the diagnostic stage, the doctor finds out the exact location of the nerve. This helps to avoid injury to the “twig”.
An experienced dentist will definitely analyze CT and X-ray data, compare the results and draw up an implantation plan based on the individual structural features of the patient’s lower jaw.
The implant is screwed in carefully; its final position should be no closer than 2 mm to the nerve process.
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Clinical picture of some individual nerves
- Trigeminal nerve – pain is sharp, piercing, in series, along one or several branches of the nerve.
- Facial nerve – muscle weakness on one side of the face. It is difficult to close the eye, the corner of the mouth on the affected side is drooping. When liquid food or drink is taken, everything comes out of the mouth.
- Diaphragmatic – feeling of lack of air, shortness of breath, hiccups.
- Median – impaired flexion of the hand, fingers I, II and III and decreased sensitivity on the palmar surface.
- Ulnar – weakness of the flexors of the IV, V and partly III fingers, decreased sensitivity on the palmar surface of the above fingers.
- Radial – impaired extension of the hand and fingers, decreased sensitivity in half of the back of the hand (I and II fingers). It is difficult to move the thumb away.
- External cutaneous nerve of the thigh (Roth-Bernhardt disease) – pain, numbness and burning along the outer surface of the thigh.
- Femoral – impairment of leg extension at the knee joint and hip flexion. Pain and sensory disturbances on the lower 2/3 of the anterior surface of the thigh, the anterior inner surface of the lower leg.
- Sciatic – pain along the back of the thigh and lower leg, weakness of the flexors and extensors of the foot.
- Olfactory – anosmia on one side (lack of sense of smell). When a nerve is irritated, foreign odors may appear.
- Visual – decreased acuity and loss of visual fields. The phenomena of nerve irritation manifest themselves in the form of photopsia (sensation of light, flames, sparks, etc.).
- Oculomotor – drooping of the upper eyelid (ptosis), limited mobility of the eyeball, dilated pupil, diplopia (double vision).
- Block - restriction of the mobility of the eyeball downwards and outwards.
- Auditory – hearing loss, often accompanied by a feeling of noise or ringing in the ear.
- Glossopharyngeal - twitching pain in the tonsils, root of the tongue, pharynx and taste disturbances in the back third of the tongue, impaired salivation and swallowing.
- Wandering – manifested by disturbances in swallowing and speech. On the affected side, the soft palate is lowered, the uvula is deviated to the healthy side. There are also disturbances in the functioning of internal organs - bradycardia, shortness of breath, motility disorders of the esophagus, stomach and intestines (spasms), etc.
- Additional – difficulty turning the head in the healthy direction, the head is tilted towards the affected nerve, the shoulder is lowered.
- Tibial – the foot is extended, but the patient cannot bend it. Cannot stand on toes. Sensitivity is reduced along the back of the lower leg and on the sole.
- Peroneal – the impossibility of standing on the heels and straightening the foot, it hangs down. Sensitivity is reduced on the outer surface of the lower leg and the back of the foot.
- Intercostal nerves – pain in the intercostal space, often radiating into the chest, simulating pain in the heart, chest, lungs, and stomach. Often, pain in the paravertebral muscles is detected at the level of the thoracic spine.
Causes
Unlike neuritis, neuralgia is not an inflammatory disease. Fever, fever, swelling and other symptoms of the inflammatory process are not associated with this disease. However, if the trigeminal nerve is damaged due to neuritis, pain sensations that fit the description of neuralgia may well occur. To avoid confusion and differentiate the two pathologies, it is necessary to consider their etiology.
The cause of neuritis (like any other inflammatory disease) is viruses and infections that cause gradual destruction of the membrane and nerve trunk, and classical neuralgia in the vast majority of cases occurs due to mechanical effects on the nerve. Today, experts identify dozens of factors that provoke the development of the disease.
Main causes of neuralgia
- Head injuries leading to changes in the cranial structure and displacement of bones.
- Benign and malignant tumors that, as they grow, compress the trigeminal nerve.
- Various bite pathologies and other dental anomalies.
- Pathologies of the structure and diseases of blood vessels located in close proximity to the nerve (atherosclerosis, aneurysm, vasodilatation, etc.).
- Sinusitis and otitis in chronic form.
- Trigeminal neuralgia after tooth extraction. Occurs during a traumatic or incorrectly performed extraction procedure.
- Damage as a result of infection resulting from a number of diseases: periodontitis, periodontitis, stomatitis, herpes, syphilis.
Trigeminal neuralgia from hypothermia occurs rarely. However, this factor contributes to the development of the disease and complicates treatment. The same can be said about decreased immunity, metabolic disorders, neurosis, diabetes and other complicating factors.
Injury Prevention
Prevention is high-quality preparation for surgery and professional performance of manipulations. A thorough study of the structure of the patient’s mandibular canal, the parameters of the alveolar process and the topographical position of the nerve fiber prevents neurological complications.
For this purpose the following are assigned:
- orthopantomogram;
- computed tomography - 3-dimensional scanning.
Complications will be avoided:
- correct formation of the implant bed;
- careful implantation of the dental structure;
- lateralization (change in the position of the nerve) when it is close to each other.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Types of trigeminal neuralgia
There is an additional classification that can also be used in making a diagnosis.
Acute
Acute trigeminal neuralgia, accompanied by frequent and severe attacks.
Chronic
Chronic trigeminal neuralgia is a consequence of an untreated disease. The patient has been observed for a long time: remissions alternate with exacerbations.
Atypical
Atypical trigeminal neuralgia occurs against a background of stress and nervous exhaustion (psychosomatics).
Postherpetic
Postherpetic trigeminal neuralgia occurs after a history of herpes and its symptoms differ from the classic type. The pain is usually burning and may not go away for two to three hours.
Therapy results
The prognosis of microsurgical and therapeutic treatment is influenced by:
- age, health status of the patient;
- skill and experience of the surgeon;
- the duration of the period between injury and surgery.
In 80% of cases of neurotmesis operated on in the first 5 months after injury, partial restoration of the function of the mandibular nerve was observed. Delaying surgical intervention systematically reduces the chance of recovery. Seeing a neuromicrosurgeon a year or more after injury has only a 10% chance of success.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Treatment of trigeminal neuralgia
Treatment and drugs
For successful treatment, complex drug therapy is used. First of all, these are anticonvulsants (carbamazepine, finlepsin or clonazepam), which are included in the mandatory rehabilitation program and relieve the main manifestations of neuralgia. The dosage and duration of treatment are determined strictly by the attending physician.
For additional effect, antihistamines and local pain relievers may be prescribed. To compensate for the lack of gamma-aminobutyric acid (a kind of mediator between the brain and the nervous system), baclofen, phenibut or gabapentin are prescribed. In the stage of exacerbation of neuralgia, specialists often prescribe antidepressants to eliminate psychological discomfort (the most common remedy is finlepsin). If the cause of the disease is a virus or infection, antiviral and antibacterial agents, as well as NSAIDs, are prescribed. During the recovery period, it is recommended to take B vitamins.
Physiotherapy
To eliminate pain, novocaine blockades and sodium hydroxybutyrate injections are actively used. The most popular and effective physiotherapeutic techniques: acupuncture, ultraphonophoresis, magnetic therapy, and low-frequency laser therapy. Massage for trigeminal neuralgia is also a good addition to general treatment and allows for better blood circulation.
What methods are used in treatment
The treatment method depends on the extent of the lesion and is carried out after assessing the sensitivity deficit. With neuropraxia, recovery occurs on its own within 4-6 weeks . No medical attention is required since the nerve structure is not damaged.
With partial degeneration, symptoms subside two months after the injury. For a complete recovery, medical measures will be needed. Numbness for 9-12 months is dangerous due to irreversible degeneration of nerve cells . Microsurgical treatment can be urgent (for an open injury) or planned (for a closed injury).
Treatment tactics for closed injury
- For numbness that does not go away for three months - suturing, transplantation;
- For dysesthesia (perversion of sensitivity) for more than 3 months - revision, decompression, neurolysis, suturing and nerve transplantation;
- If hypoesthesia (decreased sensitivity) lasts for more than 3 months, partial unscrewing or removal of the structure, revision, transplantation, suturing is indicated.
Drug treatment
Indicated for chronic nerve inflammation syndrome. An important point is pain relief. Can be used:
- Antineuralgic drugs:
- Carbamazepine;
- Phenytoin;
- Baclofen.
- Antidepressants:
- Amitriptyline;
- Imipramine.
- Local products:
- ointments with capsaicin;
- acupuncture;
- electrical stimulation;
- physiotherapy.