According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99.9%.
Key words, tags: X-rays, tooth extraction, orthopantomogram, periodontitis
A dental cyst belongs to the group of jaw cysts. Jaw cyst is a general concept that unites many pathologies. The formation of a cystic cavity in the jaw can be caused by an inflammatory process, or in rare cases, by a growing tumor. It can be in a “dormant” state and not manifest itself in any way, or, on the contrary, be in an active, acute phase, get sick, affect neighboring healthy tissues, and cause various diseases. In any case, the presence of cysts in the jaw and, in particular, the presence of a dental cyst, requires attention and serious consideration.
Tooth cyst: historical background
The word “cyst” is of Greek origin (“kystis”) and literally means “bubble.” A dental cyst is a cavity-like tumor-like formation. Previously, when X-rays were not taken, it was extremely difficult to see such formations and, as a rule, dentists encountered them during the extraction of teeth from patients. Thanks to the advent of X-ray diagnostics at the end of the 19th century (1895), it became possible to plan the treatment of dental cysts. And today, if a patient regularly visits the dentist’s office, we can successfully diagnose and eliminate dental cysts at those stages when they do not pose a danger.
Contraindications
Cystectomy is contraindicated in cases of intolerance to anesthesia and severe concomitant diseases of the heart, liver, kidneys, lungs, blood, diabetes mellitus, exhaustion, and systemic infections. In addition, partial cystectomy is not performed if a reduction in the working volume of the bladder is unacceptable for stage 0 cancer, as well as in cases where the tumor is located near the junction of the ureters and urethra with the bladder (there is no technical ability to ensure urinary function).
Tooth cyst: anatomy
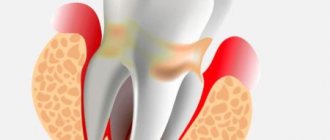
A dental cyst is a benign cavity tumor-like formation that has a membrane and an internal epithelial lining, the cells of which produce fluid. Modern medicine still cannot accurately answer the question of how and where an incipient cyst takes epithelial tissue from. However, most scientists are inclined to believe that it comes from the remnants of the dental epithelium, the so-called islands of Malasse-Astakhov. And it develops as a result of chronic odontogenic inflammation, when microbes enter the jaw bone through the tooth canal. Further development of the process can go in two directions, the result of which are pathologies: an extensive destructive process that does not have a shell - a non-shell formation (such a process is not a cyst), or a dental cyst itself - a shell-like formation.
Types of dental cysts
It is customary to distinguish between 2 types of dental cysts - follicular and radicular. Follicular cysts are less common than radicular cysts. In the presence of certain factors, it grows from the dental follicle - the membrane around the growing tooth. When it is large in size and involves adjacent teeth, it is called a follicular dentigerous cyst.
Radicular (odontogenic inflammatory) cysts form on the roots of teeth as a result of pathological processes spreading beyond the root apex. By location, radicular cysts can be apical (root), lateral (lateral), apicolateral and interradicular.
The mechanism of formation and growth of a dental cyst
The cystic cavity, located in the jaw, has external resistance from the surrounding jaw bone. But the epithelial cells of the lining begin to produce fluid, which gradually fills the cavity, creating excess pressure.
This pressure acts on the surrounding bone tissue, causing its gradual peripheral resorption, giving the cyst the opportunity to grow even larger, increase fluid secretion, and therefore put even more pressure on the walls. This is why cysts can grow to very large sizes, sometimes asymptomatically, if not accompanied by periodic inflammation. This may be due to the patient’s good immune status, low pathogenicity of the microflora in the lesion and other factors.
Rehabilitation
The recovery period for soft tissue is up to 2 months, for bone tissue - 5-6 months. The duration depends on the characteristics of the body and compliance with medical recommendations:
- eat soft foods at a comfortable temperature;
- do not eat or drink hot, spicy, salty foods;
- give up alcohol and smoking;
- brush your teeth carefully;
- take all prescribed medications.
Dentists consider cystectomy the most effective and preserving method, which is recommended for everyone in the absence of contraindications.
Possible complications of a dental cyst
As the cyst grows, it can “push aside” nearby anatomical formations, such as the canal of the inferior alveolar nerve, and can disrupt the external contours of the jaw bones (plastic toy syndrome), thereby changing the contours of the face, that is, causing facial asymmetry. It may also involve other neighboring tissues in the pathological process. So, often, retrograde periodontitis develops in the teeth located next to the cyst. And if the cyst grows into the maxillary sinuses, chronic odontogenic sinusitis is formed, which can be asymptomatic for a long time, but, nevertheless, have a detrimental effect on health.
When not to have surgery
There are some factors, the presence of which is a contraindication to dental cystectomy; the price is about 7,000 rubles. These include:
- If the purulent tumor has reached a large size, under the influence of which several elements of the dentition have fallen, as a result their structure has been disrupted, suppuration and the inflammatory process have begun.
- If a patient is diagnosed with an infectious disease or inflammation, which has caused the destruction of the structure of the teeth, their loosening, as a result, periodontitis or periodontal disease begins to develop.
- For oncological or endocrine disease, the occurrence of which is associated with an inflammatory process in the gum or tooth root. These diseases include leukemia, sarcoma, and diabetes.
- When the tooth crown is destroyed, blackened, resulting in suppuration. Causes include infectious disease and bad habits in humans.
Diagnosis of a dental cyst
The choice of treatment method for a dental cyst is based on a multifaceted diagnosis, which may include:
— examination of the patient; - “targeted” x-ray of the tooth, which the patient indicates as the causative tooth; - orthopantomogram (panoramic image of the jaw bones), which allows you to see pathologies and the most likely places of their development in the upper and lower jaws, in the maxillary sinuses, in the canals of the nerve trunks; - in some cases - a computed tomogram, which allows you to see the facial skeleton and skull bones, joints, maxillary sinuses in three projections (frontal, sagittal and horizontal) and in a three-dimensional volumetric image.
Robot-assisted RC in men
Position of the patient and localization of trocars. The patient is placed in the dorsal lithotomy position, the arms are placed along the body, the lower limbs are spread to the sides so that it is possible to bring the robot. The patient is adequately fixed to the table and placed in the Trendelenburg position at 30-450 (Fig. 1).
Figure 1. Position of the patient on the operating table
After induction of general anesthesia, the surgical field is prepared, a nasogastric tube and a sterile Foley catheter are installed. Correct placement of trocars is very important for the success of the operation. We used a 6-trocar technique with the camera port located 5 cm above the umbilicus in the midline. After insufflation of the abdominal cavity to 10-12 mm Hg. Art. under visual control, two robotic trocars were installed along the navel line on the right and left lateral to the rectus abdominis muscles. The left port is set 8 cm and the right port 10-11 cm from the midline, which provides more space for the assistant's trocar. The third of them is installed 7-10 cm lateral from the left port and 5-7 cm above the iliac crest. When performing intracorporeal urine diversion, this port is replaced with a 15 cm trocar for the stapler, which provides a better angle for resection of the small intestine and the formation of an interintestinal anastomosis. Two assistant ports are located on either side of the right robotic port. The location of the trocars is shown in Fig. 2.
Figure 2. Trocar position
Posterior dissection. Initially, both ureters are mobilized along the lower third from the area of intersection with the iliac vessels to the urinary tract. Closer to the juxtavesical portion of the ureter, two Hem-o-lock clips are applied, between them it is intersected and part of it is sent for pathomorphological examination (Fig. 3).
Figure 3. The left ureter is mobilized along the lower third and clipped
A ligature is applied to the proximal clip, which facilitates further manipulation when anastomosing the ureter with the reservoir. The vas deferens and seminal vesicles are then identified, the wall of the bladder behind the vesicles is mobilized to the Denonvilliers fascia, which is opened, and further dissection is performed between it and the rectum (Fig. 4).
Figure 4. Posterior MP dissection. A) Seminal vesicles. B) Rectum.
Retroprostatic dissection should be performed anterior to the prerectal fat to avoid rectal trauma. If the neurovascular bundles are not preserved, the seminal vesicles are left unchanged on the MP. In the case of nerve-sparing RC, they are allocated closer to the prostate, thereby avoiding damage to the neurovascular bundles, which are located laterally and close to the vesicles.
Mobilization of the bladder and prostate on both sides. After separation of the bladder from the rectum, the bladder is mobilized on both sides. The medial umbilical ligaments are identified closer to the abdominal inguinal ring. The peritoneum is divided laterally to the ligaments extending into the medial portions of the external iliac artery and into the space of Retzii. Using a combination of sharp and blunt dissection, the space between the lateral surface of the bladder and the lateral pelvic wall is widened until the pelvic fascia is reached (Fig. 5).
Figure 5. Excretion of the bladder along the lateral surface to the prostate
In this case, the urachus and umbilical ligaments should not be crossed so that the MP does not fall into the surgical field. The endopelvic fascia is then opened and the lateral surface of the prostate is exposed.
Clipping and intersection of MP vessels. The vas deferens is divided to provide access medial to the external iliac vessels, and lateral dissection is continued. Using the fourth arm, the MP is retracted cranially. With sufficient retraction, the lateral crura can be well identified for division with LigaSure or clipping with Hem-o-lock clips. First, the superior cystic artery is isolated and clipped (Fig. 6).
Figure 6. Clipping of cystic vessels
Next, the inferior cystic and vesicoprostatic arteries are mobilized. Isolation of the pedicles of the bladder ends on the superolateral portion of the prostate near the seminal vesicles while preserving the neurovascular bundles. They are located in the posterolateral part of the prostate and are easily distinguished all the way to the apex of the prostate. Nerve-sparing dissection for RC can be performed using a similar technique as for robot-assisted prostatectomy. The incision is performed in the periprostatic fascia and continues distally to the apex of the prostate. In this case, thermal injury or excessive traction of the neurovascular bundles should be avoided. Next, the vascular pedicles of the prostate are isolated and dissected between Hem-o-lock clips. This technique effectively preserves the lateral periprostatic fascia. We performed infrafascial dissection in patients with low prostate-specific antigen levels, and they did not have prostate cancer in our RC series.
Mobilization of the anterior wall of the bladder and urethra. The urachus and medial umbilical ligaments are coagulated with a bipolar dissector and divided. The anterior wall of the bladder and prostate are distinguished. The dorsal venous complex is ligated and divided, and apical dissection of the prostate and urethra is performed along the length (Fig. 7).
Figure 7. Mobilization of the prostate and urethra
Next, the Foley catheter is removed and a Hem-o-lock clip is placed on the urethra closer to the prostate to prevent urine or tumor cells from entering. Alternatively, a similar clip can be applied to the Foley catheter after tightening its balloon, which assists in traction of the bladder with the prostate (Fig. 8).
Figure 8. After cutting off the urethra, a clip is applied to the Foley catheter.
The released drug is placed in an endobag. The pelvis is washed with an antiseptic solution and hemostasis is performed by coagulation or suturing of bleeding vessels. After drainage is established, the drug is removed through the widened wound of one of the ports.
Removal of a dental cyst. Historically significant and modern methods of surgery for removing dental cysts
Initially, the most common method of treating cysts was their removal. For this purpose, 2 fundamentally different methods were used: cystotomy and cystectomy.
Cystotomy (or the PARCH-I method) has historical significance in the development and establishment of medicine. Today this method is practically not used, but previously it was indispensable for removing large cysts. To avoid complications and its severe consequences, a wide channel was created between the cyst cavity and the vestibule of the oral cavity by suturing the edges of the cyst shell with the oral mucosa.
Cystectomy (or PARCH-II method) involves complete excision/removal of the cyst. This surgical intervention is often simultaneously accompanied by the removal of the root apex, the source of the formation of the cyst containing infected apical deltas. Today this method is the most popular.
The main goal of cystectomy is complete sanitation of the cyst cavity, which is not possible without resection of the root apex. The fact is that the root pulp in its apical third has an apical delta with an unclear structure and very fine branching of the canals, even in single-rooted teeth. If such canals can be cleaned during tooth treatment, then during retreatment this is almost impossible, especially considering the narrowness of the lateral deltas. Removing the root apex, in addition, allows you to most effectively clean the cyst cavity behind the root. This is especially true for teeth 12 and 22, which have a more curved root system. The operation is carried out as follows: using a small incision on the gum, the surgeon very carefully reaches the surface of the bone located above the cystic cavity, removes the wall with a trephine or bur, making sure that the neighboring teeth are not damaged, and then removes the cyst shell and performs a resection of the root apex . Next, sanitation of the cystic cavity is carried out and its subsequent revision for residual cyst particles. After this, in some cases, retrograde filling is performed. The final step in the operation to remove cystic formations is filling the resulting cavity with osteoplastic material and suturing the wound.
In the case of the formation of a large cyst, amputation of the apex of the tooth root can be performed, or half of the tooth and damaged root can be removed (hemessection), and in the case of an interradicular cyst, this can be done by corono-radicular separation.
Stages of cystotomy
This type of surgery is less complicated compared to a completely removed cyst. The operation is easier and faster, with a minimum of contraindications. The main disadvantage is a defect in the oral cavity that requires special care.
Operation plan:
- local anesthesia;
- antimicrobial treatment of the oral cavity and mucous membranes;
- dissection of the gums up to the neoplasm;
- cutting the capsule wall, removing the contents, disinfection;
- connection of the walls of the cystic capsule with the soft tissues of the gums;
- treatment with drugs;
- applying a cotton swab with iodine.
At the end of the operation, an additional sinus is formed in the oral cavity, so hygienic treatment procedures must be carried out correctly, according to the recommendations of the attending physician. The treatment does not end there - the patient must undergo a course of antibiotics and anti-inflammatory drugs.
With proper care, complete healing of the wound and resorption of the capsule occurs within a year, but if the case was complex, then recovery can take up to two years.
Quality criteria for dental cyst removal
Despite the fact that cystectomy is a surgical intervention, the main indicator of the quality of treatment will be the sanitation of the root canals, including retrograde filling. Currently, in addition to eliminating the cyst shell itself, the unspoken rule has become the filling of its cavity with one or another osteoplastic materials, because this completely eliminates the possibility of blood clot suppuration, promotes rapid healing of the bone defect and improves the mechanical stability of the tooth.
Indications for tooth extraction with a cyst
As a rule, conservative treatment carried out on time or surgery to remove the cyst allows you to save the tooth. But this is not always possible. A tooth must be removed in the following cases:
— the presence of severe pain symptoms when drug treatment is ineffective; - purulent inflammatory process when it is impossible to drain it; — fracture of the coronal part of the tooth, without the possibility of restoration with anchor pins and/or stump inlays; — obstruction of root canals; — the presence of multiple damage to the roots of the tooth or large damage; the tooth is almost completely destroyed and orthopedic restoration is impossible; - no need for dental treatment due to the presence of a prosthetic plan agreed upon between the doctor and the patient.
Execution technique
Cystectomy is performed under general anesthesia, which not only anesthetizes, but also bleeds the surgical field. Next, the following activities are performed:
- bone exposure;
- gaining access to the cyst;
- removal of the formation (in case of union with the root, its resection is performed);
- filling;
- antibacterial treatment of the bone cavity;
- suturing.
To prevent the appearance of a hematoma, a pressure bandage is applied to the operated area, which is removed after 5-7 days.
Subsequently, the patient is prescribed treatment with anti-inflammatory, antiallergic and painkillers.
Price
The cost of treatment or removal of a dental cyst consists, like many other surgical interventions, of a number of factors. The complex of diagnostic procedures performed, types and methods of treatment, conservative preparation of canals, preoperative preparation, the operation itself, the osteoplastic materials used, postoperative observation - all this affects the final cost of treatment in these clinical situations.
A dental cyst is a serious pathology. In all cases, even in cases of complete absence of any symptoms, it poses a health hazard. With regular visits to the dentist, you can be sure: a dental cyst, if there is one, will be detected in time, and subsequent treatment will allow it to be eliminated without leaving a trace, preserving the health of the tooth.
According to antiplagiat.ru, the uniqueness of the text as of October 16, 2018 is 99.9%.
Key words, tags: X-rays, tooth extraction, orthopantomogram, periodontitis
Discussion
Robot-assisted RC is gradually taking its place in the surgical treatment of patients with muscle-invasive bladder cancer. Robot-assisted access makes it possible to reduce the number of intra- and postoperative complications, primarily to reduce the amount of blood loss, shorten the length of hospitalization and rehabilitation of patients 5, 8, 10, 11. The complexity of RC is aggravated by the comorbidity of patients, who are often elderly. RC is a long-term intervention that includes three defining stages: bladder removal, pelvic lymph node dissection and urine diversion 4, 6, 8. At the beginning of mastering the robot-assisted RC technique, we sought to comparatively simplify the operation, breaking each stage into small steps. When performing them, we tried to follow a certain order of execution, that is, we moved on to each subsequent stage after completing the previous one. There are several key benefits to this structured approach. Firstly, the RC technique is simplified and its results are improved. By working in one specific area, the surgeon's attention was focused on a single task at that time before moving on to the next step. It is important to achieve adequate hemostasis at all stages of RC, which provides good visualization and reduces the amount of blood loss. Even from our initial experience, we were convinced that a systematic approach to performing RC allowed us to reduce the operation time. Secondly, in our opinion, with a detailed description of the individual steps of the operation it is easy to teach young specialists and conduct adequate monitoring of training.
Open RC with extended lymph node dissection remains the gold standard for the treatment of bladder cancer, providing excellent local tumor control with a 50–70% five-year cancer-specific survival rate 13–16. The role of robotic surgery in the treatment of cancer continues to evolve with increasing popularity and is supported by good short- to mid-term results 10, 12, 17. RC is primarily performed for cancer, and therefore the effectiveness of any approach will be judged on the basis of long-term survival outcomes. Robot-assisted RC has been performed in some clinics for more than 15 years; data from robot-assisted RC with Kaplan-Meier analysis were published for 36 and 60 months, comparable to series after open RC 5, 8, 11. Thus, according to Collins JW et al. 8 The five-year cancer-specific survival rate was 67%.
RC through various approaches is associated with a certain number of perioperative complications and severe morbidity 13-16. According to various authors, with open RC their number ranges from 49% to 64% 6, 10, 13-17. Clavien-Dindo high-grade complications range from 13% to 40%, and 90-day mortality range from 0% to 4.5% 13, 16. Robot-assisted RC also has a high complication rate, but relatively fewer, according to compared with open RC 12, 18-20. Collins JW et al. 8 early complications (0-
30 days) was observed in 54 (47.8 %), grade 3 according to Clavien-Dindo - in 37 (32.7 %) patients. Late complications (more than 30 days) occurred in 30 (26.5%), grade 3
according to Clavien-Dindo - in 20 (17.7%), 1 (0.9%) patient died from pulmonary artery embolization. A recent meta-analysis showed that robot-assisted RC compared with open RC is associated with fewer perioperative complications, a higher number of lymph nodes removed, longer operative time, reduced blood loss and fewer blood transfusions, and a short hospital stay. 12 Further prospective studies of robotic outcome -assisted RC with a long period of observation will allow us to confirm the data of this analysis.