Pneumonia or pneumonia is a viral disease that affects the lung tissue and interferes with the normal exchange of oxygen between air and blood. Inflammatory secretions that enter the alveoli do not allow the body to receive a sufficient amount of oxygen. And if the disease affects most of the lungs, acute respiratory failure develops.
Pneumonia affects people with weak immune systems, children and the elderly. Every year in Russia alone, 1.5 million people suffer from the disease, and 30% of them are young children and people over 70 years of age.
But pneumonia can and should be treated! And it is recommended to do this using an integrated approach. Treatment of any disease begins with a correct diagnosis. Therefore, at the first signs of the development of pathology, seek the advice of a specialist.
What are the first symptoms of pneumonia, how to approach treatment correctly and comprehensively, and what is required to diagnose the disease, we will tell you in this article.
Causes of pneumonia
Pneumonia develops when bacteria and viruses, as well as foreign agents, enter the lungs and affect part or all of the lung tissue. Pathological agents enter the human body through the respiratory route, and rarely through the blood.
Why does the disease develop quickly in the body of a person with reduced immunity? Bacteria are constantly present in our body, but protective mechanisms do not allow them to multiply, causing pathology. But if the immune system is weakened, harmful microflora increases in population, which leads to the appearance of an inflammatory process.
Viral pneumonia also often develops against the background of the spread of colds of the upper respiratory tract (bronchitis, tracheitis). Pneumonia can also be caused by hypothermia, stress, overwork, or smoking abuse. The risk of developing the disease increases in people with chronic diseases and obesity.
Factors influencing adaptation time
The individual characteristics of a person, his psychotype and desire, influence how quickly he can get used to removable dentures.
Other factors include:
- How well the design fits in the mouth. If the restoration does not adhere well to the palate, it causes constant discomfort. It is difficult to get used to such a prosthesis. It shrinks and damages the mucous membranes.
- Is there any pain? It's hard to feel like your artificial jaw is yours when you're constantly in pain.
- Prosthesis design. It is easier to get used to clasp dentures than to plate dentures. It will take longer to get used to the upper denture.
- Quality of manufacture of dentures. The gag reflex will not go away if the distal (back) edge is too long and irritates the palate. A poorly fitted restoration rubs the gums and causes discomfort when chewing. This design needs correction.
Getting used to removable dentures occurs much faster if the denture is not your first. Usually it takes 3-5 days
.
Signs of pneumonia in an adult
When the disease appears, a person’s body temperature rises, which can reach 38°, there is general weakness throughout the body, a headache, the patient wants to lie down and relax. After a few days, a strong paroxysmal cough appears and sputum appears.
Pain in the chest, especially at the site of inflammation, as well as the appearance of shortness of breath indicate the seriousness of the situation and clearly indicate pneumonia.
General signs are listed here, but the nature and timing of their manifestation may differ depending on the type of pneumonia. With viral pneumonia, the first symptoms appear quickly and the patient feels a sharp deterioration in health. From the very beginning of the disease, muscle pain, high body temperature, severe headache, and a painful dry cough are observed.
Bacterial pneumonia, on the contrary, develops gradually. The disease begins only 2 weeks after the first symptoms appear. After this, there is a sharp relief, an improvement in the general condition of the patient, then the temperature rises sharply again, a headache occurs, the cough intensifies, and purulent sputum appears.
One of the serious types of the disease is atypical bilateral pneumonia, which extensively affects the lung tissue and develops respiratory failure. In terms of its symptoms, bilateral pneumonia resembles a cold viral infection, and the characteristic wheezing is not yet heard in the lungs. Many begin to treat themselves, which aggravates the condition.
At first, the sick person thinks that his condition has improved, the symptoms of the pathology begin to go away. But then the cough worsens and the second wave of the disease begins.
Symptoms may vary slightly in older people. First of all, a dry cough and shortness of breath appear during minor physical exertion on the body or even at rest. Often the disease occurs without fever in older people.
How to quickly get used to dentures
Simple recommendations will help you go through all 3 phases of addiction much faster. However, it should be remembered that the main thing is the psychological attitude. It will help you endure discomfort more easily and fight the temptation to remove the prosthesis. Visualizing a new smile, imagining changes in appearance and life, and thinking about what problems a new jaw will solve promote emotional and physical relaxation and accelerated adaptation. This is especially true for the upper jaw, because it is more difficult to get used to a denture with a palate. It takes up a lot of space, blocks the taste buds, and is very disturbing.
The following will help you get used to dentures faster:
- Diet
. In the first days after installation of the restoration, it is better to avoid solid foods. Porridge, puree soups, curds and yoghurts will help you survive the most difficult first days until chewing function is restored. - Slow chewing
. Be sure to involve both sides in the process to evenly distribute the load. - Adhesive preparations
. Creams and gels like Corega (Corega) help to better fix the jaw while the muscular system gets used to the restructuring. - Reduced physical stress
on the jaw. At first, it is better to cut food into pieces and avoid biting. - Conversations and reading aloud
. Diction after dental prosthetics will be restored faster if you talk a lot. The more you train, the faster the phonetic apparatus will adapt to the new state. You can slowly count to 100. Read prose and poetry, gradually increasing the pace. Talk with loved ones.
Dentists' advice: do not remove the structure at night during the adjustment period. This also promotes faster adaptation to dentures.
Is pneumonia contagious?
The inflammatory process in the pulmonary system most often appears due to the multiplication of the virus and as a complication of influenza or acute respiratory viral infection. In such cases, it is impossible to get sick from pneumonia itself, but it is easy to catch the disease that became the root cause. That is, pneumonia itself is not contagious, and the development of inflammation in the lungs is an independent complication that arose against the background of a weakened immune system and improper self-medication.
Can pneumonia go away on its own without treatment?
Pneumonia or pneumonia is one of the most dangerous and common diseases of the respiratory system. The danger is that specialists do not always have time to make a diagnosis in time. People do not go to the doctor with a cough and fever, but prefer to stay at home for a couple of days until the disease spreads. The condition can worsen to bilateral pneumonia, which carries severe consequences, long-term treatment or chronic diseases.
A hundred years ago, before the discovery of penicillin, pneumonia took the lives of those who fell ill. Science and medicine do not stand still - our lives have changed dramatically in a hundred years. People have antibiotics in every medicine cabinet, and hospitals carry out operations using modern equipment. However, according to the Russian Academy of Sciences, pneumonia is still on the list of the deadliest infectious diseases and should not be underestimated.
Pneumonia will not go away on its own. This disease can lead to death, so seeing a doctor is vital. Treatment for pneumonia should be prescribed by a doctor. It is he who determines whether antibiotics are needed and which ones, and also decides on the severity of the disease.
With pneumonia there is always a high temperature and a strong cough, is this true?
This is a very big and dangerous misconception. Errors in diagnosing the disease are one of the main causes of mortality from pneumonia. According to doctors, up to 30% of cases of pneumonia are not diagnosed or detected too late, since people do not see the need to see a doctor before a high temperature appears. As a result, this leads to a deterioration in the person’s condition and the development of severe complications. Asymptomatic, hidden, but real pneumonia often develops in children and the elderly. The main and most dangerous problem in diagnosing pneumonia in elderly patients is that the disease successfully disguises itself as various chronic diseases. In this case, it passes without the most important marker of the disease for us - without fever. How then do you understand that pneumonia is going away in an adult? - Monitor your body, and promptly consult a doctor if your health worsens.
If you have what signs you should consult a doctor?
- increased sweating;
- weakness;
- dyspnea.
By the way, the myth that pneumonia is necessarily accompanied by a severe cough is just a myth. This problem is mostly characteristic not of the older generation, but of children. There are often cases when pneumonia progresses, but there is no cough. If you do not consult a doctor in time and do not make a diagnosis, the child may experience chronic consequences.
Pneumonia in children can be identified by the following symptoms:
- shortness of breath and chest pain when moving;
- pain when turning the body
- inability to take a deep breath;
- tachycardia;
- exercise intolerance;
- fast fatiguability;
- weakness;
- the person looks pale, but with a bright, unhealthy blush.
How is pneumonia transmitted?
The disease can be transmitted in different ways, including:
- Airborne method. During the disease, droplets form on the mucous membrane of the mouth and nose, which spread through the air during sneezing and coughing. You can become infected by airborne droplets in any public place: hospital, store, public transport. The pathogenic agent spreads through the air along with particles of mucus, sputum, and saliva.
- Contact. The infection is also transmitted through contact - shaking hands, hugging, kissing. People become infected when they touch contaminated objects or when they touch their mouth, eyes, or nose with dirty hands.
- Domestic. The infection can be transmitted through shared towels, dishes and bedding. Therefore, the patient needs to be provided with personal hygiene items, and, if possible, change and wash them more often.
- Fecal. The virus survives up to two days in fecal matter with normal bowel movements. You can easily acquire the disease from improper toilet cleaning or personal hygiene. To prevent infection, especially from young children, it is important to constantly wash your hands after cleaning the child's potty, change diapers frequently and thoroughly wash the area where bowel movements occur.
However, personal hygiene items must be handled very carefully. It has been proven that the viral microorganism can survive up to 4 hours on any surface. Morbid bacteria are not afraid of frost; even with bleach it can be destroyed only five minutes after direct treatment.
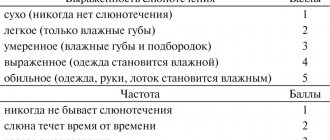
Xerostomia and hypofunction of the salivary glands: diagnosis and treatment
Hypofunction of the salivary glands, which is manifested by a lack of saliva, can be caused by the influence of a huge number of factors. Causes of xerostomia (a feeling of dry mouth), and therefore hypofunction of the salivary glands, include mouth breathing, smoking tobacco or marijuana, candidiasis, menopause, aging, dehydration, diabetes, radiation therapy and a number of other general somatic disorders (depression, stress, autoimmune neuropathy, CREST syndrome, eosinophilic myalgia syndrome, HIV/AIDS, Lyme disease, lymphoma, multiple sclerosis, Parkinson's disease, primary billiard cirrhosis, primary fibromyalgia, rheumatoid arthritis, Sjögren's syndrome, lupus, SOX syndrome, goiter, hyperlipidemia type 5). At the same time, completely unsubstantiated medications can often be used to stimulate salivation. Complaints of dry mouth are more common among older patients; approximately 80% of patients with xerostomia are people 80 years of age and older, who, in addition to dryness, experience signs of burning and taste disturbances, even when taking certain prescribed medications.
In order to determine the cause of hypofunction of the salivary glands, doctors have to resort to a laboratory blood test, and at times, to a biopsy of the salivary glands, the results of which can make a diagnosis of Sjögren's syndrome, amyloidosis, and sarcoidosis.
Clinical features associated with saliva
Hypofunction of glands
A patient with hypofunction of the salivary glands or with a feeling of dry mouth is characterized by the presence of a number of clinical signs and symptoms. The latter include impaired sensitivity and speech function, burning in the tongue and mucous membranes for no reason, as well as upon contact with certain foods, oral candidiasis, signs of biting the cheeks, cheilitis, caries, erosion and abrasion of dental tissues, dysphagia, food getting stuck between teeth, gingivitis and periodontitis, halitosis, GERD, general weight loss. Such clinical symptoms begin to develop when salivation decreases by at least 50%, and patients may experience both individual symptoms of the lesion and complexes of such symptoms.
When salivation is impaired, saliva parameters also change. It becomes white, foamy, thick, sticky and fibrous. Because of this, the patient may feel the presence of a kind of salivary film on the teeth and mucous membranes. Sometimes patients complain of an excessive amount of saliva in the mouth, which is caused by the fact that its density increases. Normally, the rate of salivation reaches 2-3 ml for 5 minutes; when it increases to more than 1 ml for a minute, sialorrhea is diagnosed. In patients with signs of dry mouth, the normal level of salivation is reduced by approximately one-fold.
With reduced salivation, the oral mucosa becomes dry and during diagnostics, gloves, rollers and even dental mirrors may stick to it. Filiform papillae and fissures may be visualized on the back of the tongue, the presence of which allows a diagnosis of a hairy tongue to be made (photo 1). In the cervical areas of the tooth, areas of carious lesions are often visualized (photo 2), small erythematous spots are diagnosed on the buccal mucosa, where bite marks from the teeth may also be present (photo 3). Patients may also have signs of gingivitis, recession, and periodontitis (Figure 4).
Photo 1. Whitish filiform papillae in a patient with xerostomia. There is also an odor from the mouth.
Photo 2. Carious and associated lesions in a patient with xerostomia.
Photo 3. Traces of biting the cheek.
Photo 4. Signs of gingivitis with severe hypofunction of the salivary glands.
The questionnaire for diagnosing xerostomia was designed specifically to assess existing disorders from a subjective point of view. It includes 11 statements (“I feel dry mouth”, “I have difficulty eating”, “I wake up at night to drink water”, “I feel dry mouth when I eat”, “I drink water to make it easier to swallow food”, “I have difficulty swallowing certain foods”, “The skin on my face seems too dry”, “My eyes feel dry”, “My lips feel dry”, “I have a feeling of dryness in the nasal cavity”), which patients rate using 5 possible options: (1) Never, (2) Hardly ever, (3) Sometimes (4) Quite often or (5) Very often . A score of 11 indicates the presence of moderate xerostomia, while a score of 55 indicates severe xerostomia. If the patient has already been diagnosed with xerostomia, the doctor may ask a few additional questions: Do you think the volume of saliva in the oral cavity is sufficient for you? Do you feel dry when eating? What complications do you experience when swallowing? Do you drink water to make it easier to swallow food? How often?
Objective diagnosis
Patients with mild xerostomia may not experience dry mouth at all, but they may also experience other symptoms of the disorder. As one of the tests to objectify the symptoms of xerostomia, it is recommended to evaluate the rate of salivation at least once a year. Moreover, such an assessment can be carried out both with stimulation of salivation and without any stimulation of the process. To diagnose the rate of salivation, the doctor uses a tube, a separatory funnel, strips for determining pH, and strips for conducting a Schirmer tensile test. The volume of salivary secretion after stimulation can be determined after the patient has chewed paraffin for 1 minute. These data can be compared with data obtained without stimulation, as well as data after administration of a specific drug that stimulates salivation.
Assessment of salivary flow can also be performed using Schirmer strips and pH strips before and after administration of 5 mg pilocarpine. Two hours before the test, the patient should not eat, drink, chew gum, or even brush his teeth. Diagnosis of unstimulated salivation is carried out in the dental chair with the patient in the coachman position, with his hands on the armrests. The patient holds the measuring funnel and tube on his lips, while his eyes should be open, but blinking is not prohibited. Within 5 minutes, saliva should simply flow into the flask and tube. After this, the collected volume of saliva is divided by 5, thus allowing you to set the rate of salivation per minute. Normal average values are 0.3-0.4 ml/minute.
Thus, hypofunction of the salivary glands is diagnosed when the saliva flow rate is less than 0.3 ml/min. When this indicator is less than 0.1 ml/min, then a severe form of hypofunction of the salivary glands is recorded. Normally, the pH of saliva is 7-7.5, that is, it is neutral or somewhat alkaline. A low rate of salivation provokes the development of dental erosion, irritation of the mucous membrane and a burning sensation. When the rate of salivation is normalized, pH values are usually normalized, and vice versa - with hypofunction of the salivary glands, the pH of saliva becomes more acidic.
Treatment
Saliva is a complex fluid consisting of enzymes, proteins, minerals and other components that help maintain a healthy oral cavity. Thus, normalization of salivation is an integral aspect of the complex treatment of dental patients. For patients who cannot control salivary stimulation, saliva substitutes or saliva analogues in the form of lubricants are used. The specific treatment for xerostomia depends on the underlying causative disease. The goal of such therapy is to relieve the symptoms of dry mouth, and to ensure the prevention of associated complications in the form of caries, candidiasis and other lesions. In addition, treatment of xerostomia also helps to slow down the complete loss of salivary gland function, and sometimes even promotes its restoration. At least in autoimmune diseases, with the help of salivary stimulants, it is possible to maintain a certain level of salivary gland function for as long as possible, and a drug such as rituximab even helps restore the structure of the salivary glands in Sjogren's syndrome. Taking dietary supplements such as coenzyme Q10 100 mg per day for 1 month also helps increase salivation and reduces the development of symptoms of dry mouth. Treatment of pharmacologically induced xerostomia is carried out in the same way as treatment of other forms of this disease. This form of pathology, as a rule, is reversible, but the dentist must take into account what kind of drug it was caused by, and what part he takes in the treatment of general somatic pathology. Control of the main symptom of dry mouth can be carried out with pilocarpine or cevimeline, as well as other drugs, depending on the current state of the pathology. The future in the treatment of xerostomia clearly involves genetic engineering, the use of stem cells and tissue engineering, but the principles of therapy remain the same: normalization, optimization of salivary flow, ensuring adequate hydration of the oral cavity and creating conditions for lubrication of all oral structures.
Normalization/optimization of salivary flow rate
Ideally, treatment of hypofunction of the salivary glands involves restoring their function and the physiological rate and volume of salivation. One treatment option is to stimulate saliva production by taking appropriate medications. The latter allow you to increase the initial level of salivation, thus also reducing the risk of developing subsequent complications (caries and candidiasis). Improvement in salivary flow rate can be achieved by taking pilocarpine 5 to 7.5 mg in tablet form three to four times daily or capsule 30 to 60 mg three times daily. Pilocarpine and cevimeline are salivary stimulants that the FDA prescribes for the treatment of dry mouth symptoms. By their nature they are muscarinic agonists. They increase saliva flow and reduce the feeling of dry mouth. The most common side effects with these medications are sweating, frequent urination, and gastrointestinal discomfort. These drugs should not be taken for uncontrolled asthma, narrow-angle glaucoma and acute iritis. They should also be prescribed with caution to patients with severe forms of cardiovascular disorders, Parkinson's disease, asthma or chronic obstructive pulmonary disease.
Polycarpine and cevimeline are cholinergic agonists that stimulate muscarinic-type receptors in the structure of the salivary glands and, to some extent, in the structure of other exocrine glands. Pilocarpine usually begins to work within 20 to 30 minutes, lasts 3 to 5 hours, and has no residual effect. Taking pilocarpine 20-30 minutes before meals with a glass of water allows you to achieve an optimal level of salivation already at the time of eating, facilitating the processes of chewing and swallowing. Taking the drug before bedtime will help relieve symptoms in those patients who are most bothered by dry mouth at night. Cevimeline begins to act in 30-90 minutes and provides an effect for 6-8 hours. This drug, unlike pilocarpine, has a residual effect, and over time, patients experience a higher salivary flow rate. Patients may also notice increased swallowing after starting to take the salivary stimulant. The fact is that the frequency of swallowing decreases with hypofunction of the salivary glands, and returns to normal during the treatment of xerostomia.
Normally, the patient swallows up to 2000 times a day. If the patient cannot restore the speed or required volume of salivation, he may be prescribed artificial saliva. Such drugs are Caphosol (EUSA Pharma), NeutraSal (OraPharma) and SalivaMAX (Forward Science); Aquoral (Mission Pharmacal). They help relieve dry mouth due to certain diseases, inflammation, medications, chemotherapy and radiotherapy, stress, and aging. Aquoral, in addition to relieving xerostomia, also helps solve difficulties with swallowing, speech and changes in taste.
Hydration
Dehydration of the oral cavity is associated with a reduced level of salivation, but the latter may be associated with general dehydration of the entire body. The loss of about 8% of the human body’s water, which is about 4 liters of fluid, provokes the development of an almost complete absence of salivation. Even after rehydration, the function of the salivary glands is restored only after 24 hours. During this period, saliva can be replaced by drinking 64-80 ounces of drinks that do not contain alcohol or coffee. The volume of fluid required can also be determined by dividing the patient's weight (in pounds) by two to obtain the number of ounces of fluid that should be drunk daily.
Oral lubrication
Since salivary stimulants do not restore the physiological function of saliva, sometimes patients find it necessary to use additional lubricants to relieve discomfort during speech or swallowing. These types of drugs include ACT Dry (Chattem Inc.), Allday Dry Mouth Spray (Elevate Oral Care), Biotene Oralblance (GlaxoSmithKline), Entertainer Secret Throat Relief (KLI Corp.), MedActive Oral Relief (MedActive Oral Pharmaceuticals, LLC), MighTeaFlow (Camellix), MI Paste (GC America), Moi-Stir Mouth Moistening Spray (Kingswood Labs, Inc.), Mouthe Kote (Parnell), Oasis (Gebauer Consumer Healthcare), Orajel (Church and Dwight, Inc.), Salese ( Nuvora Inc.), Salivart Synthetic Salica (Gebauer Consumer Healthcare), SalivaSure Saliva Substiture Tablets (Scandinavian Pure and Naturals), Spry Rain mouth spray (Xlear, Inc.), Stoppers4 Dry Mouth Spray (Woodridge Labs), Xerostom products (Practicon) . Patients may be encouraged to try new products to find the ones that work best for them. Rinsing the mouth with salt water or salt water (1/2 teaspoon) and sodium bicarbonate (1/2 teaspoon) diluted in 8 ounces of water helps cleanse the mouth, neutralize acids, and remove plaque. A drop of mineral oil or glycerin placed on the tongue can completely spread throughout the oral mucosa and improve the patient's comfort level. Oral care recommendations also include drinking plenty of water, brushing your teeth at least twice a day, chewing sugar-free gum, visiting your dentist regularly, and not smoking, caffeine, or alcohol.
Stimulation of salivation - electrical stimulation
Transcutaneous electrical nerve stimulation (TENS) applied to the parotid gland for 5 minutes increased salivary flow in 68-81% of patients in the study. Various types of TENS machines are available for this purpose and have been approved by the FDA. They are portable analogues of the ballpoint pen shape that produce electrical impulses. These can already be purchased in Europe and Australia; in the USA they have not yet undergone final certification procedures.
Behavioral changes
The dentist's recommendations for treating xerostomia may require changes in certain aspects of the person's behavior. The latter include drinking water more often, using various fluoride-containing topical preparations, as well as various rinses, avoiding sugar-containing chewing gum, and using saliva-replacing gel-lubricants, sprays, and moisturizers. These products can be used as often as needed because they do not react with prescription medications and generally have no side effects unless the patient is sensitive to a particular ingredient. Studies have shown that patients prefer to use saliva stimulating drugs rather than salivary substitutes. In addition, dentists may recommend that patients with dry mouth rinse with salt water, eat ice chips, and swallow small amounts of liquid frequently.
In addition, chewing also stimulates the flow of saliva, so eating certain foods daily, such as raw carrots, can help treat xerostomia. You should avoid cigarettes, alcohol, caffeine and spicy, salty or acidic foods, as well as refined carbohydrates (sugar) in your diet if you have symptoms of dry mouth. Patients with xerostomia should take good oral care through frequent brushing, flossing, and fluoride-containing toothpastes and gels. For selected patients at increased risk of developing dental caries, mouth guards can be made for overnight fluoridation treatments. Moisturizing gels can also be used once or twice within an hour of bedtime to reduce the level of discomfort after the mouth guard.
conclusions
Patients with xerostomia or hypofunction of the salivary glands can be diagnosed based on the presence of certain clinical symptoms and the results obtained during an objective diagnosis of the level and condition of salivation. Current treatment options for xerostomia include taking certain medications to manage symptoms and prevent potential complications. Such medications include salivary stimulants, artificial saliva, lubricants, rinses, sprays and gels. Stimulation of salivation can also be achieved through electrical stimulation. Treatments such as gene therapy, stem cell therapy or tissue engineering may become the mainstay in the future for correcting salivary gland dysfunction.
Author: Susan L. Zunt, DDS, MS
Pneumonia and bronchitis: what is the difference?
Both diseases affect the human respiratory system, which means they have similar symptoms. It is often difficult to distinguish the two pathologies from each other.
| Pneumonia | Bronchitis |
| In most cases, it is accompanied by a sharp increase in temperature to 38-39° and a feverish state. There is a slight increase in temperature. | Accompanied by a strong dry cough. In some cases, sputum may appear greenish or streaked with blood. Wet cough, sputum is light in color. |
| When listening to the chest, “wet” rales are heard. | When listening to the chest, “dry” wheezing is heard. |
How is pneumonia diagnosed?
If a child suffers from the disease, you should seek examination from a pediatrician. If you are an adult, make an appointment with a therapist who will refer you to a specialist if necessary. The doctor will conduct an external examination, collect anamnesis, study the medical history and learn about the symptoms of the disease.
You will be sent for laboratory tests:
- General blood analysis;
- General urine analysis;
- Sputum analysis is carried out to determine the inflammatory process in the body, as well as the causative agent of pneumonia and its sensitivity to antibiotics.
Among the diagnostic research methods you will be prescribed:
- Chest X-ray - shadows appear in the images in areas of tissue damage;
- Computed tomography and magnetic resonance imaging are used as additional measures when other methods do not allow an accurate diagnosis.
Methods for treating pneumonia
If pneumonia is bacterial in nature, antibiotics are prescribed. Their effectiveness can be assessed after 48-72 hours. If the temperature subsides, the cough becomes less frequent, and the patient begins to feel better, the treatment continues. You cannot interrupt the course of medications, and it is important to take them correctly as prescribed by your doctor. If antibiotics do not help, another treatment is prescribed or changed to a drug from another group.
For viral pneumonia, antibiotics are not effective, so antiviral drugs are prescribed. Vitamins and immunomodulators can be prescribed as auxiliary substances.
Once the patient's body temperature has returned to normal, physical therapy can be prescribed. It allows you to remove phlegm from the lungs. For this purpose, herbal medicines are often taken, for example, licorice root or complex breast mixtures.
Along with drug treatment, patients need bed rest, meals containing protein and vitamins, and plenty of warm drinks. For the best effect, therapeutic methods are recommended - electrophoresis, inhalation, massage, magnetic therapy, etc.