Sore throat or acute tonsillitis is an inflammatory process that develops on the palatine tonsils, caused by an infectious infection. The main complaint with a sore throat is a sore throat. It occurs due to inflammation of the tissue of the pharynx, which leads to local swelling, which in turn compresses and irritates the nerve endings of the throat. A sore throat can also be a manifestation of acute pharyngitis and laryngitis. The difference between acute tonsillitis and these two diseases is that different tissues of the pharynx are involved in the process. In acute pharyngitis, the inflammatory process is observed in the area of the posterior wall of the pharynx. Laryngitis affects the tissues in the vocal cords area. And with tonsillitis - palatine tonsils. Only a doctor can diagnose the disease and select the correct treatment regimen, so if you experience symptoms of a sore throat, make an appointment with a pediatrician at our private medical clinic “Doctor Anna”.
Types of sore throat
There is a classification of angina according to external manifestations and forms of progression, among which the most common can be identified:
- Catarrhal. The tonsils are enlarged, red, and in places covered with mucus and pus. The tongue is covered with a white coating.
- Lacunar tonsillitis. It has similar manifestations to follicular, but is more severe. Both purulent spots and purulent plaque appear on the tonsils.
- Follicular. The symptoms are similar to the catarrhal form, but more pronounced. Yellowish-white purulent dots appear on the tonsils - this is what inflamed follicles look like.
- Phlegmonous. Purulent melting of the tonsils, which occurs with a weakened immune system, massive infection with microbes, or with improper treatment of milder forms of tonsillitis. Most often it is one-sided.
- Herpes sore throat. On the tonsils there are rashes in the form of blisters, redness, acute pain and fever. Develops when infected with the Coxsackie virus.
Follicular and lacunar forms refer to purulent tonsillitis. Pus accumulates in the tonsils, which is released when pressed.
Specific features of herpetic sore throat
Herpetic tonsillitis can be distinguished from other types of sore throat by the following characteristics:
- A rash appears on the upper and lower extremities and face if not treated in a timely manner.
- Numerous red blisters appear on the pharynx, adenoids, tongue, and palate. Gradually they develop into ulcers and open. A light transparent exudate emerges from the bubbles. Typically there are from 5 to 20 ulcers in the mouth. If treatment is not started in time, the ulcers merge with each other, forming large areas of damage to the mucous membrane of the throat and mouth. In this case, there is a high risk of complications.
Often, parents mistake herpangina for another disease and try to cure it on their own. Herpetic sore throat should not be confused with:
- Thrush. Candidiasis in the mouth appears as a cheesy coating.
- Herpetic stomatitis. Papules are similar, but with stomatitis they are localized on the gums and tongue.
- Purulent sore throat. Formations accumulate only on the tonsils and lacunae, and with herpetic disease they cover the entire nasopharynx. In addition, a runny nose is a distinctive symptom. With purulent tonsillitis there is no runny nose.
Causes of sore throat
The root cause of this disease is viruses and bacteria. The most common of them are beta-hemolytic streptococcus and staphylococcus. They can enter the body from the environment or from sources of chronic infection within the body itself. The immune system of a healthy person should suppress pathogenic microorganisms, but there are provoking factors for the development of sore throat:
- smoking;
- deficiency of vitamins and balanced nutrition;
- hypothermia;
- throat trauma;
- the presence of other inflammatory processes.
Factors in the development of sore throat
Sore throat is primarily an infectious disease. Inflammation of the tonsils can be caused by various microorganisms, primarily staphylococcus and streptococcus. In addition, the following factors can provoke a sore throat:
- hypothermia of the body;
- long exposure to polluted air;
- lack of sunlight;
- dampness;
- poor nutrition;
- unhealthy living conditions;
- overwork of a person.
Sore throat in children
Children, unlike adults, have a particularly difficult time with sore throat, which is accompanied by severe pain, high fever up to 39-40 degrees, difficulty swallowing and difficulty breathing. A child can become infected at school or kindergarten. The most dangerous form of the disease occurs in children under one year of age, so when it is diagnosed, the child is usually hospitalized. The disease begins with an increase in temperature, acute pain in the throat and the feeling of a lump when swallowing. Parents can palpate enlarged submandibular lymph nodes. Swelling of the airways causes difficulty breathing, which may cause the child to snore while sleeping. If a child has all the signs of a sore throat, self-medicating and using folk remedies is extremely dangerous, so you should definitely make an appointment with a pediatrician. For a speedy recovery, children should not only take all necessary medications and observe only bed rest, but also adhere to a special diet. It consists of eating a large amount of pureed and baked fruits and vegetables, soups, broths and a sufficient amount of liquid - fruit drink, tea, juice. It is recommended to exclude various seasonings and hot sauces, very hot foods, salty and fried foods.
Complications of GABHS-pharyngitis
In most cases, GABHS pharyngitis resolves without complications. Non-purulent complications include acute rheumatic fever, post-streptococcal glomerulonephritis, childhood autoimmune neuropsychiatric disorders associated with streptococcal infection. Purulent complications of streptococcal pharyngitis include necrotizing fasciitis and bacteremia.
The differential diagnosis of GABHS pharyngitis includes both infectious and non-infectious causes of pharyngitis.
The main viral diseases manifested by acute pharyngitis:
- infectious mononucleosis - Epstein-Barr virus (EBV) and cytomegalovirus. More common in adolescents and characterized by fever, severe pharyngitis (which lasts longer than GABHS pharyngitis), anterior and posterior cervical or diffuse lymphadenopathy. Periorbital edema, mild hepatomegaly, and splenomegaly may be present. Patients prescribed ampicillin, amoxicillin (sometimes other antibiotics) may develop a characteristic rash;
- primary HIV infection —may cause an acute retroviral syndrome (similar to infectious mononucleosis) in sexually active adolescents or rarely in sexually abused children. Clinical signs of primary HIV infection include severe cervical or generalized lymphadenopathy and complaints of fever, weight loss;
- herpes simplex virus - pharyngitis caused by the herpes simplex virus, manifested by blistering rashes on the mucous membrane, lips;
- influenza - characterized by fever, cough, headache and myalgia, which occur during seasonal epidemics;
- other viral diseases - enteroviruses, adenoviruses, rhinoviruses, coronaviruses, respiratory syncytial virus, parainfluenza viruses.
The main bacterial causes of pharyngitis:
- streptococci of groups C and G - there is still a debate about the role of these bacteria in the etiology of acute pharyngitis;
- n eisseria gonorrhoeae (gonorrhea) is a relatively rare cause of pharyngitis. Most cases are asymptomatic or symptoms are nonspecific (eg, pharyngeal congestion, swelling or exudate in the tonsil lacunae);
- f usobacterium necrophorum (Lemierre's syndrome) is the cause of most cases of purulent thrombophlebitis of the jugular vein. Clinical signs include strep throat, high fever (39°C), respiratory symptoms, unilateral neck swelling or pain;
- diphtheria - rare in developed countries, but important to consider in patients from endemic areas. Unlike GABHS pharyngitis, which has an acute onset, the onset of diphtheria symptoms usually occurs gradually. A distinctive feature of diphtheria is the formation of a gray filmy coating that adheres tightly to the mucous membrane of the nose and throat, the removal of which leads to bleeding;
- others - tularemia (Francisella tularensis), Arcanobacterium haemolyticum, Mycoplasma pneumoniae.
Non-infectious causes of pharyngitis are diagnosed based on medical history. This may be irritation or dryness of the pharynx, a foreign body (for example, a fish bone), chemical exposure, radiating pain due to dental abscess, acute otitis media.
Sore throat in adults
It is worth remembering that this disease is infectious in nature. Therefore, if treatment takes place at home, it is necessary to use individual cutlery and try to have less contact with others. In severe cases of acute tonsillitis, it is possible to place the patient in a hospital under the supervision of doctors. Every adult with a high degree of probability has suffered from a sore throat at least once. But, if it occurs frequently, the palatine tonsils increase in size, become looser, deformed, and their protective function—participation in the formation of immunity—is disrupted to such an extent that they themselves become a constant source of infection. In the tonsils, even without an exacerbation of the disease, pus, mucus and food waste begin to accumulate, and purulent plugs form, creating bad breath. All these manifestations are symptoms of chronic tonsillitis. This disease is dangerous because an inflammatory process constantly occurs in the tonsils, leading to frequent exacerbations. In this case, there is the greatest likelihood of complications for internal organs. A chronic process in the palatine tonsils reduces immunity, weakening the body and making it more susceptible to various infections.
Prevention of sore throat
In addition to general restorative therapy and measures aimed at preventing infection, preparations of bacterial origin, in particular complexes of antigens - lysates, the most common causative agents of inflammatory diseases of the upper respiratory tract, oral cavity and pharynx, have proven to be an effective means of preventing exacerbations in various forms of pharyngitis and recurrent tonsillitis. It is possible to use similar drugs with systemic action, but this group of drugs has a greater number of contraindications.
It should be noted that all patients suffering from chronic tonsillitis who have had more than 2 sore throats over the past 3 years are subject to mandatory follow-up in group D3, that is, 2 times a year.
Symptoms of a sore throat
There are a number of signs by which you can independently suspect the disease:
- sore throat when swallowing, may radiate to the ears;
- feeling of dry throat, sore throat;
- increased body temperature from slight to 39-40 degrees, impaired general condition, weakness, drowsiness, chills, headache;
- enlarged lymph nodes;
- changes in tonsils.
Even if the patient knows how to treat a sore throat, it is under no circumstances possible to squeeze out purulent plugs on your own, because with mechanical impact on the tonsil, it is possible to extract only a small fraction of the contents, the bulk remains inside, which sinks deeper under pressure, which is fraught with complications (abscess , edema, phlegmon of the neck, sepsis).
Diagnosis of sore throat
The success of treatment will depend on timely and competent diagnosis. The first stage of the examination is to examine the condition of the patient’s pharynx, during which the attending physician will assess the main signs of the disease: the degree of enlargement of the tonsils and the presence or absence of purulent plaque. It is also necessary to assess the degree of enlargement of the lymph nodes in the ears, neck and back of the head.
Taking blood tests will determine the degree of increase in leukocytes and ESR, characteristic of bacterial tonsillitis. With viral sore throat, the leukocyte level remains within normal limits or decreases slightly, and the erythrocyte sedimentation rate increases slightly.
To determine the causative agent of the disease, cultures of mucus from the oropharynx are examined in laboratory conditions. This is important for determining the class of the disease and competently prescribing medications for the treatment of sore throat. For complicated or particularly acute symptoms, the attending physician may prescribe an ultrasound of the neck.
Complications
It is necessary to take angina very seriously, since this disease can cause serious complications on the heart and joints in the form of rheumatism, the kidneys can be affected and glomerulonephritis occurs. If you ignore the problem, sore throat may develop into a chronic form, which is called chronic tonsillitis. Lack of timely treatment can lead to abscess of the retropharyngeal space, sinusitis and sinusitis, and otitis media. Purulent inflammation of the neck and inflammation of the mediastinal organs are very dangerous conditions, often resulting in death. Also characteristic are autoimmune lesions of the heart and kidneys, meningitis, sepsis, and rheumatoid arthritis.
Complications of sore throat
Complications can be early or late. Early ones (peritonsillitis, peritonsillar abscess, etc.) are caused by the spread of infection to neighboring organs and occur during illness. Late ones appear after 3-4 weeks and are of infectious-allergic origin (articular rheumatism, rheumatic carditis, streptococcal glomerulonephritis).
Attention! Complications of tonsillitis most often occur during self-medication. Only timely comprehensive treatment of sore throat under the supervision of an otolaryngologist will protect you from the serious consequences of the disease!
Diagnostics
You can independently suspect a disease in yourself or a child, first of all, by a sore throat and painful swallowing. Often the causes of pain are a cold or an acute respiratory viral infection, which lead to pharyngitis. If the pain is acute, this is a manifestation of a sore throat, but only a doctor can say for sure. There are different criteria for making a diagnosis. One of them is anapestic or collection of data, the causes of the disease, possible contacts with infected people, the presence of throat diseases in relatives. Next, a visual examination is carried out, during which the doctor evaluates the pharynx, tonsils, and performs pharyngoscopy. In order to identify the disease, the doctor takes swabs from the throat to determine the type of bacteria, as well as to determine sensitivity to various antibiotics. 2 hours before taking a smear, it is prohibited to consume food and various drinks. In addition, a general blood test, urine test and an electrocardiogram are performed to monitor treatment and monitor sudden complications. If leukocytosis and a neutrophilic shift are detected in the blood, this indicates a bacterial origin of the disease, and if there is a higher level of monocytes and eosinophils, we can speak of a viral infection.
Treatment of acute tonsillopharyngitis
Antibiotic therapy is recommended for any patient with symptomatic pharyngitis or tonsillopharyngitis who has a positive rapid antigen or culture test for group A streptococcus.
Empirical treatment is generally not recommended because there is significant overlap between the clinical features of GABHS pharyngitis and nonstreptococcal pharyngitis. Short delays in therapy (eg, while awaiting culture results) do not increase the incidence of complications, including acute rheumatic fever. However, it is unknown whether such treatment delays affect the incidence of other complications (eg, development of peritonsillar abscess).
If clinical suspicion for GABHS pharyngitis is high and test results cannot be obtained quickly, it is advisable to initiate antibiotic treatment while awaiting test results. If the diagnosis is not confirmed, antibiotics should be stopped.
Antibiotic treatment is not recommended for asymptomatic chronic GABHS carriers or for GABHS carriers with signs of acute viral pharyngitis.
Antibacterial therapy
The drug of choice for the treatment of GABHS pharyngitis is penicillin antibiotics. Penicillin is the only antibiotic that has been studied and shown to reduce the incidence of acute rheumatic fever. For complete eradication of GABHS, the duration of the course of antibacterial therapy is 10 days.
Amoxicillin is more preferable for young children. It can be given once daily using an extended-release form (suspension). In several randomized trials, amoxicillin suspension at a standard dose (once daily) was found to be as effective as penicillin taken orally.
In case of allergy to penicillins or poor tolerance, preference is given to cephalosporin antibiotics, lincosamides (clindamycin) and macrolides - the choice of drug depends on the type of allergic reaction to penicillin.
Studies that combined data from more than 5000 adults and children showed no clinically significant difference between cephalosporins, macrolides, or clindamycin compared with penicillin or amoxicillin in the resolution of GABHS tonsillitis symptoms. But no studies have assessed the use of alternatives to penicillin for the prevention of acute rheumatic fever. Thus, penicillin remains the drug of choice whenever possible.
Tetracyclines, sulfonamides and fluoroquinolones should not be used to treat streptococcal pharyngitis due to high resistance and high side effect profile.
Nonsteroidal anti-inflammatory drugs (ibuprofen) or acetaminophen (paracetamol) may be used to relieve fever and pain.
How is acute tonsillopharyngitis treated at the Rassvet clinic?
When diagnosing a sore throat, we always pay attention not only to the pharyngoscopy picture, but also to the presence of signs of a viral infection. This means we do not perform streptococcus tests on all patients with acute pharyngitis.
If there are signs of GABHS pharyngitis, we must perform a rapid test; if indicated, we take material for testing only for GABHS. Confirmation of streptococcal infection helps prevent unnecessary prescription of antibiotics for viral pharyngitis.
We do not prescribe throat swabs for flora. Streptococcal infection is one of the few causes of tonsillopharyngitis for which treatment with antibiotics is recommended. To this day, the need for antibacterial therapy for most other pathogens remains controversial. Other bacterial infections that strictly require treatment include diphtheria and gonorrhea.
We do not order an ASLO test on the first day of illness (ASLO - antistreptalizin-O, antibodies produced in response to the toxin of group A beta-hemolytic streptococcus). ASLO increases only 10-20 days after the onset of streptococcal infection. There is also no point in monitoring it every week, since this marker begins to decrease 3-5 weeks after the illness, but its levels can be higher than normal for up to a year.
We understand that the main goal of antibiotic therapy for streptococcal pharyngitis is to prevent complications. Treatment with antibiotics has been shown to reduce the severity of symptoms and speed recovery in patients with streptococcal pharyngitis, but even without antibiotic therapy, in most cases, symptoms resolve within three to five days.
We do not treat any plaque in the throat with antibiotics, since their presence does not equal streptococcal tonsillitis, nor vice versa.
Treatment
Treatment of sore throat is the responsibility of a therapist; you should contact him at the first suspicion of this disease, and in no case should you self-medicate. Different types of sore throat require different approaches to treatment; there is no universal cure. Many unqualified doctors for any throat disease, even mild sore throat, prescribe antibiotics to the patient, despite the fact that frequent use of these drugs leads to resistance and causes great harm to the body.
If the process is chronic, doctors suggest solving the problem radically by removing the tonsils. However, these approaches are incorrect, since an experienced specialist must first examine the patient and select a competent treatment regimen for him, trying in every possible way to avoid surgical intervention. You should turn to antibiotics as a last resort and only as prescribed by a doctor, because their prolonged and frequent use leads to a decrease in immunity. Also, many throat diseases are caused not by bacteria, but by viruses, against which antibiotics are powerless. Tonsils or tonsils should be removed only as a last resort, when the inflammation is very severe and no other treatment methods help. After all, the tonsils are the body’s protective gates, protecting it from any infections. Also, immune cells are produced in the tonsils; without them, immunity decreases and, if they are removed, the chances of contracting a particular infection increase. After such an operation, you can get quite serious problems with the heart and kidneys, and various allergic diseases can develop. Instead, the doctor may prescribe the use of Iodinol. This drug has a low cost in pharmacies and is much more effective than many expensive medications. With its help, it is recommended to prepare a solution with which to gargle regularly. But “Iodinol” has contraindications due to the fact that it affects the thyroid gland, therefore it is not suitable for autoimmune thyroiditis, pregnant women and nursing mothers. In this case, you can use inexpensive antiseptics such as Chlorhexidine and Miramistin. To treat tonsillitis, they also use a relatively inexpensive and very effective device for home use - a quartz ultraviolet irradiator with special throat attachments.
An important contribution to treatment is increasing immunity and drinking enough fluids. It is recommended to remove sweets and sugary, carbonated drinks from the diet, as sugar is a breeding ground for the development of microorganisms. In case of chronic illness, you should check the health of your teeth, because throat diseases often occur against the background of the fact that there is an infection in the oral cavity.
Treatment of sore throat
Sore throat is a fairly serious infectious disease that cannot be cured only by drinking herbal infusion and rinsing. Antibiotics for sore throat are mandatory. Treatment of sore throat in adults and children should be carried out under the guidance of a physician.
1 Diagnosis of sore throat
2 Diagnosis of sore throat
3 Diagnosis of sore throat
Our clinic uses all modern methods of diagnosis and treatment of ENT pathology. Otolaryngologists at MedicCity are professionals with extensive experience.
Attention! Sore throat is contagious, so the patient should be isolated from children and the elderly. He should have his own dishes and towel for the period of illness.
For mild cases, treatment of sore throat is outpatient. Severe forms of the disease require hospitalization in the infectious diseases department.
1 Diagnosis of sore throat
2 Diagnosis of sore throat
3 Diagnosis of sore throat
In the first days, bed rest, mild warm food, and plenty of fluids (fruit juices, compotes, milk, alkaline mineral water) are indicated. The prescription of antibacterial drugs is mandatory. Rinsing with antiseptic solutions and herbal decoctions is also used. Irrigation of the tonsils with various drugs is also prescribed. After a sore throat, it is necessary to follow a gentle regimen for some time to avoid complications.
Diagnosis and treatment
To make a diagnosis and determine treatment approaches, you need to consult an otolaryngologist. Diagnostics is carried out according to the following algorithm:
- collection of medical history and complaints;
- examination of the pharynx using special lighting (pharyngoscopy);
- general and biochemical blood test;
- bacteriological examination of a smear with the preparation of an antibiogram.
How to treat a purulent sore throat is determined by an ENT specialist. In severe cases, hospitalization is required. General medical recommendations include bed rest, drinking plenty of fluids, taking vitamins and restorative medications.
Specific treatment of the disease is a complex of procedures and medications:
- Drug treatment of the oral cavity.
Complex therapy necessarily includes gargling with antiseptic solutions. For this purpose, solutions of furatsilin, manganese, hydrogen peroxide, sea salt, and natural herbal decoctions (chamomile, calendula) are used. This procedure is aimed at removing pathogenic microorganisms from the throat and mouth. - Taking systemic antibacterial drugs.
A full course of antibiotic therapy allows you to get rid of pathogenic flora. Antibiotics and their dosages can only be determined and prescribed by a doctor. The most commonly used drugs are from the groups of penicillins, macrolides and cephalosporins. - Symptomatic therapy.
To alleviate the patient’s condition during the acute stage, the specialist prescribes symptomatic treatment in the form of antipyretics, antihistamines and anti-inflammatory drugs. Sometimes it is recommended to undergo physiotherapeutic procedures during the recovery period.
Correctly selected treatment helps to avoid serious consequences and ensures healing of the affected tissue areas without visible defects.
Causes and risk factors
If a person has a weakened immune system for some reason, the risk of necrotizing tonsillitis becomes higher. A major role in the development of the pathological process is played by the low local resistance of the flora to pathogenic agents. Protective substances in the nasopharynx cannot fight pathogenic bacteria or there are very few of them.
When the pathogen enters the nasopharynx, it quickly ends up in tissues with primary localization in the area of the palatine tonsils. Bacteria begin to produce toxins that destroy lymphoid tissue. Erosion and ulcers occur.
Also, the risk of necrotizing tonsillitis arises:
- with poor nutrition and malnutrition;
- with a pronounced lack of vitamins and minerals;
- for chronic intestinal infections and other protracted illnesses.
The risk of developing ulcerative membranous tonsillitis is high in patients suffering from leukemia and cancer. Poor oral hygiene can also lead to illness. Smoking for many years, infection with helminthic infestations, long-term treatment with antibacterial drugs and working with hazardous chemicals also contribute to the development of this disease. Stress and overwork aggravate the situation, as does any hypothermia. Among the foci of chronic infections, particularly noteworthy are progressive dental caries and other dental pathologies.
Complications and consequences
The advanced form of the disease leads to inflammatory damage to other organs, including the heart, kidneys, and joints. The most dangerous complications include:
- mediastinitis
– inflammation of the mediastinal tissue; - chronic bronchitis
- inflammatory damage to the bronchi; - sepsis –
spread of infection through the bloodstream; - arthritis -
inflammation of the joints; - glomerulonephritis is
a dangerous kidney disease; - purulent meningitis -
damage to the meninges; - peripharyngeal abscesses
- suppuration of the lymph nodes and tissue of the peripharyngeal space.
Timely access to a medical facility allows you to avoid negative health consequences.
Symptoms
The main manifestations of gumboil disease are pain in the area of the causative tooth and the appearance of swelling in the soft tissues of the face. If at the beginning of the disease the swelling is mild, then as the process progresses the swelling increases and can spread to the eye area, scalp or neck. As the symptoms of flux increase, pus from under the periosteum can spread through the fatty spaces closer to the skin - this is manifested by the fact that the skin turns red, becomes dense and hot to the touch. Further, the skin in the center of the flux softens, becomes thinner, and a fistula with purulent discharge may appear. In this case, pain may decrease somewhat, which is associated with a decrease in pressure in the flux cavity during the formation of a fistula tract.
In addition to pain, symptoms such as limited mouth opening or inability to open the mouth, and pain when swallowing may occur. If the flux is located deeply, facial swelling may be mild or not expressed at all, and the main manifestations will be limitations in mouth opening, pain in the flux area and pain when swallowing.
Signs and symptoms
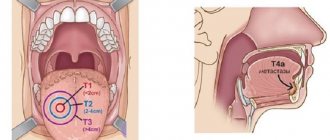
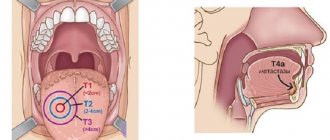
There are three forms of ulcerative membranous tonsillitis:
- Easy. The temperature is normal or subfebrile, the oral cavity is hyperemic, and there is plaque on the tonsils. The lymph nodes are not enlarged, and it is painful for the patient to swallow.
- Average. The temperature rises to 38, the throat hurts constantly, including when eating. The tonsils are inflamed and swollen, their surface is covered with dark spots, sometimes with a whitish tint. The spots are round, up to 1.5 cm in diameter, and can merge. When trying to remove the plaque, blood is found under the film.
- Heavy. Critical temperature readings reach 40, the tonsils are swollen, depigmented, swelling and inflammation involve the surrounding tissues.
Necrotizing tonsillitis can be a separate disease, but sometimes it is associated with ulcerative stomatitis, the causative agent of which is the same. An important diagnostic point: as a rule, only one of the tonsils becomes inflamed. A process localized on both sides is a rare occurrence.
The first symptoms of any sore throat include a feeling of discomfort and pain during swallowing. An objective examination shows that one tonsil is affected and a gray coating is visible on it. It is often compared to a candle drop. The flight includes:
- dead due to tissue necrosis;
- leukocytes;
- pathogenic microflora that caused the infection.
Ulcers with jagged edges become larger, and the patient’s mouth smells unpleasantly of rot. Fever can be expressed in different ways, depending on the stage of the process. In severe cases, enlargement and pain of regional lymph nodes are observed.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!
In the absence of treatment and the disease is neglected, the infection spreads from the tonsils to the entire soft palate. When coccal microflora is added, the patient’s general condition deteriorates in the form of high fever and severe sore throat.
If necrotizing tonsillitis is treated correctly, therapy will take approximately 14 days.