Causes
Unlike ordinary sore throat, herpetic sore throat is caused by viruses. Among the main provocateurs, it is worth highlighting the Coxsackie virus type A or B, serovars, and ESNO viruses. They can be infected by droplets, fecal-oral routes, through bodily contact, and unprocessed food.
The pathogen, entering the body, multiplies in the intestines and lymph nodes. The pathogen spreads through the lymph and blood and intensively accumulates in the pharyngeal ring and tonsils. On the third day, the condition of the infected person deteriorates sharply.
Is the disease contagious?
Regarding the contagiousness of glossitis, it is quite difficult to give a definite answer, since the disease has many different forms, which mainly depend on the root cause of the problem.
“You say that the disease is rarely transmitted, but my son brought this infection from kindergarten! The diagnosis is herpetic glossitis. The tongue was swollen, covered with tiny sores, the child cried in pain. After the examination, the therapist prescribed us tablets and rinses and advised us to buy pharmaceutical chamomile. In principle, I won’t say that the treatment took a very long time, maybe a couple of weeks, but the unpleasant impressions remained. In my family, neither I nor my sisters had this, so I was generally in a panic...”
Lydia D., Nizhny Novgorod, from correspondence on the woman.ru forum
Some forms of the disease can be transmitted by contact
. If the provoking factor is not an infection, then there will be no risk of transmission from the carrier to a healthy person. If the whole point is infection and spread of the fungus, then the disease can be transmitted, but not by airborne droplets, but as a result of direct contact of another person with the affected organ.
Symptoms
The following clinical picture appears sharply, acutely and violently:
- Within a few hours the temperature rises to 40°C.
- Chills and general weakness of the body appear.
- My head starts to hurt.
- When swallowing saliva or liquid, an unbearable sore throat develops.
- The color of the mucous membrane of the nasopharynx changes. After a few hours, the throat turns red, and the next day it becomes covered with many reddish blisters.
Acute symptoms last for 2-3 days, and then their intensity decreases.
What is ulcerative glossitis
Glossitis, as a rule, becomes a consequence of injury to the mucous membrane of the organ, as a result of which an open wound appears on its surface - a direct path for the penetration of bacteria and infections. This injury can be caused by accidental biting, trauma such as fish bones, exposure to overly spicy or acidic foods, or burns from eating excessively hot foods.
The photo shows ulcerative glossitis
The pathology itself is inflammatory in nature - painful ulcers appear on the surface of the tongue, the tissues of the organ swell, turn red, painful sensations and burning occur, and in the case of the ulcerative form, a dense coating of a grayish tint also forms. The result is unpleasant odor from the mouth, difficulties with eating and speaking.
Symptoms of herpetic sore throat in children
Children attending nurseries or kindergartens, as well as schoolchildren, get sick most often. In children in the first three years of life, herpetic sore throat is extremely difficult, since the first signs of the disease are similar to the flu.
In addition to the general signs of intoxication, children appear:
- Temperatures up to 41°C.
- Pronounced hyperemia of the mucous membranes of the mouth and pharynx. During examination, the tissues appear to be filled with blood.
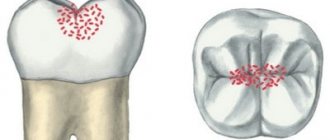
- A day later, 1-2 mm papules in the mouth, surrounded by a red rim. The next day they open, forming ulcers with crusts.
- Runny nose.
- Decreased appetite due to impossible pain.
- Enlarged lymph nodes located in the neck and ears.
If children have weak immunity, then sore throat occurs in waves, i.e. The deterioration of the condition is recorded after a few days, then it improves noticeably.
In addition, children experience stomach upset due to the fact that viruses irritate the mucous membrane of the digestive tract. The child complains of diarrhea and nausea.
Causes, symptoms and types of stomatitis on the tongue
Modern medicine has a huge variety of causes of stomatitis. As a rule, they are either bacterial or viral in nature. Not only adults, but also children can suffer from stomatitis on the tongue. Here are the most common causes of stomatitis on the tongue:
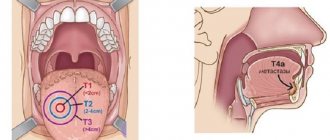
- Infectious diseases: diphtheria, influenza, scarlet fever, measles, acute respiratory infections. Such diseases are usually accompanied by acute stomatitis. Its development is facilitated by constant irritation of the mucous membrane during smoking, alcohol abuse, and regular consumption of too cold, hot or spicy foods. Among stomatitis caused by infection, herpetic stomatitis (herpetic sore throat) or stomatitis in the throat is distinguished. It is caused by various enteroviruses. In addition to stomatitis in the throat, this virus can cause enteroviral vesicular stomatitis with exanthema, acute hemorrhagic conjunctivitis, and aseptic (serous) meningitis. If you suspect that you have stomatitis in the throat or herpetic sore throat (white or grayish-yellow blisters in the throat), contact your doctor immediately to clarify the diagnosis.
- Diseases of the digestive system and stomach.
- Bad habits.
- Dental damage: tartar, caries, periodontitis, bleeding gums.
- Various types of damage: mechanical or chemical. For example, low-quality dentures, chipped teeth. Such violations can lead, first of all, to the appearance of stomatitis on the lip. The thin, delicate skin of this area is injured (burn, chapping, etc.), through microcracks in the thin and delicate skin of this area, an infection enters the body, causing stomatitis on the lip.
- Worm infestation.
- Weakened immunity, vitamin deficiency.
Characteristic signs that you have stomatitis are a white-yellow coating. Then gray spots appear on the tongue, reaching up to 0.5 mm in diameter. Sometimes they change shape or merge into one large spot. By the way, they may not hurt or bother you at all, and ulcers may not appear either. But, nevertheless, even if there are no pronounced symptoms of stomatitis, treatment is necessary, otherwise stomatitis can become acute. In addition, the lack of proper and timely treatment can provoke recurrent stomatitis - an inflammatory disease of the oral cavity that is chronic, but has periods of remissions and exacerbations. Sometimes it occurs as an independent disease.
One of the common manifestations of stomatitis in both children and adults is severe swelling of the tongue, which thickens and becomes covered with ulcers. After epithelial detachment, red, atrophied areas of skin remain, which cause a burning sensation. It becomes painful to eat and talk. One of the symptoms of the disease in a child is often tearfulness, moodiness, and restless behavior. If they appear, you should immediately consult a doctor. As a rule, stomatitis in children develops much faster and more painfully.
There are several types of stomatitis on the tongue:
- Catarrhal: characterized by high fever and profuse salivation, and may cause bad breath.
- Aphthous: the appearance of small ulcers (aphthous) that are covered with a yellowish coating.
- Ulcerative-necrotic: characterized by the appearance of ulcers covered with a gray coating.
Diagnosis and treatment
At the appointment, the ENT doctor will examine the patient and conduct an examination. Based on the diagnostic results, drug therapy is prescribed, including:
- Taking antipyretics based on paracetamol or ibuprofen.
- Taking antiviral drugs prescribed after identifying the exact pathogen.
- Taking antihistamines. The active substance helps relieve swelling and ease breathing.
- Resorption of lozenges, lozenges, use of local sprays. Their antiseptic and bactericidal properties reduce sore throat.
- Local use of antiviral ointments based on interferon.
- Taking immunostimulants to activate the body's defenses to fight the pathogen.
It must be emphasized that antibiotics are powerless for this type of tonsillitis, because they do not affect the reproduction of viruses.
Important to remember! Do not apply heat compresses to the throat. Heating promotes the further spread of viruses throughout the body.
In addition to taking medications, the patient must be isolated from others and observe strict quarantine. The infectious period lasts two weeks. You need to follow a diet and eat pureed liquid food, drink more liquid. Water not only prevents dehydration, but also relieves symptoms of intoxication. If you are sick, you should not smoke, drink boiling water or water from the refrigerator.
Since the throat is constantly injured, healing occurs within 10-14 days. Crusts and sores are washed off with saliva without any residue.
It is important to know! Do not touch the bubbles with your hands or try to squeeze them out.
Standard Treatments
Since the inflammatory process develops in an open form and is local in nature, rinsing for necrotic sore throat is necessary. One of the best options is to treat the tonsils with hydrogen peroxide (3 percent solution). Potassium permanganate, furacillin and potassium chloride also help well. You need to gargle as often as possible, at least 6 times a day.
Doctors prescribe antibacterial drugs for the progressive course of necrotizing tonsillitis. Groups of antibiotics can be as follows:
- penicillin;
- cephalosporin;
- macrolides.
The first group consists of all penicillin drugs (including amoxicillin), from the second group cefazolin is often prescribed. The third group is represented by erythro- and clarithromycin. It is she who is the safest of all the others. Side effects when using macrolides are minimal, so they can be prescribed in childhood.
The patient should also stay in bed and eat well. Antipyretics are used as symptomatic treatment.
If the sore throat is very severe or recurs, the issue of surgical removal of the tonsils should be raised.
Specific features of herpetic sore throat
Herpetic tonsillitis can be distinguished from other types of sore throat by the following characteristics:
- A rash appears on the upper and lower extremities and face if not treated in a timely manner.
- Numerous red blisters appear on the pharynx, adenoids, tongue, and palate. Gradually they develop into ulcers and open. A light transparent exudate emerges from the bubbles. Typically there are from 5 to 20 ulcers in the mouth. If treatment is not started in time, the ulcers merge with each other, forming large areas of damage to the mucous membrane of the throat and mouth. In this case, there is a high risk of complications.
Often, parents mistake herpangina for another disease and try to cure it on their own. Herpetic sore throat should not be confused with:
- Thrush. Candidiasis in the mouth appears as a cheesy coating.
- Herpetic stomatitis. Papules are similar, but with stomatitis they are localized on the gums and tongue.
- Purulent sore throat. Formations accumulate only on the tonsils and lacunae, and with herpetic disease they cover the entire nasopharynx. In addition, a runny nose is a distinctive symptom. With purulent tonsillitis there is no runny nose.
Traumatic factor
Every person can experience mechanical damage to the tongue. It could be:
- biting;
- regular use of a rough toothbrush;
- damage during dental therapy;
- tissue damage from teeth, dentures, braces;
- irritation from food or medications.
Treatment of tongue sores resulting from injury occurs quickly and without complications. For the first few days, the damaged mucous membrane will react to all irritants. But the reaction will become less and less every day, and over time it will completely disappear.
Complications
Unfortunately, this type of tonsillitis has dangerous negative consequences if the disease is started and left to chance. The greatest danger is from complications of the kidneys, brain and heart. Since the sore throat virus spreads through the flow of lymph and blood, inflammation can overtake certain parts of the brain, causing meningitis and encephalitis. Convulsions, persistent headache, increasing temperature are reasons to seek medical help again.
At the ENT CLINIC in Chertanovo, ENT doctors with extensive experience will carefully examine an adult and a small patient and immediately perform a serological and virological analysis to determine the causative agent. The technical equipment of our medical center allows us to obtain diagnostic results within a couple of hours. Thanks to this, therapeutic therapy is prescribed in a timely manner, with positive dynamics occurring the very next day.
Types of ulcers and their clinical manifestations
The appearance of suspicious neoplasms on the surface of an organ is always an alarm bell that cannot be ignored. In this case, the rashes may differ from each other, depending on the disease and the cause of its appearance. Let's consider various clinical manifestations of pathologies of the oral mucosa and find out what they may indicate.
White sores on the surface
If white or yellow ulcers appear on the back of the tongue, gums and inner surface of the cheeks, first of all you need to find out why they appeared. Most often, such a symptom indicates candidiasis (thrush) - it develops as a result of too intense proliferation of yeast fungi in the body.
The problem can be triggered by a sharp decline in immune defense or, for example, taking powerful medications, including antibiotics. With yeast glossitis, rather deep grooves form on the tongue, in which an abundant dense coating begins to accumulate. These symptoms are accompanied by itching and an unpleasant odor. The problem does not pose a serious threat if treatment with antifungal agents is started in time.
This is what leukoplakia of the tongue looks like
Another possible cause of white rashes is leukoplakia. The pathological process is accompanied by excessive growth of soft tissue cells and the appearance of whitish thickenings on the surface of the organ. This diagnosis is often made to heavy smokers, as well as to patients who experience constant trauma to the mucous membrane due to an incorrectly installed filling/crown or due to the crooked position of some teeth.
Reddish translucent bubbles
Almost colorless growths, often filled with blood, usually indicate problems in the digestive system or endocrine glands. Reddish blisters appear on the tip and root area of the tongue, as well as on the inner surface of the cheeks, including with atopic dermatitis.
It could also be due to infection or damage to the mucous membrane. So, for example, a single transparent blister may be the body’s reaction to a thermal burn. Bloody hematomas indicate sudden changes in blood pressure or vascular damage.
The photo shows a blister filled with blood.
Discolored blisters
As mentioned above, colorless neoplasms in the form of blisters most often appear after a burn to the mucous membrane. If small bubbles filled with serous fluid appear on the tongue or other part of the oral mucosa, this may indicate activation of the herpes virus in the body. Sometimes with scarlet fever, light gray rashes appear in the mouth, which gradually become brighter and spread to the throat.
This is what herpes looks like on the tongue
Ulcers on the lateral surfaces
The formation of ulcers is most often a consequence of organ injury. The wound becomes a favorable environment for the proliferation of bacteria, which often leads to the formation of a purulent boil. Sometimes a dark rash appears on the side surfaces, resembling a hematoma in its shape and appearance. This symptom indicates damage to the deeper layers of the epithelium and taste buds.
Ulcerative rashes due to stomatitis
In the first stages of the development of the disease, small rashes appear on the oral mucosa, more like a slight swelling. Gradually more pronounced aphthae appear, when damaged, a white or yellowish membrane with a red rim forms in their place. Such ulcers heal in just a couple of weeks and do not leave scars. Aphthous stomatitis can become chronic. In this case, periods of exacerbation usually bother the patient 1-2 times a year.
The photo shows stomatitis on the tongue
Afty Bednar
Erosive areas appear on the surface of the organ - a similar phenomenon is usually diagnosed in newborns and young children. The cause of canker sores is most often caused by minor injuries received during feeding, due to the habit of sucking the thumb while sleeping or putting foreign objects into the mouth. However, neoplasms, as a rule, are localized on the surface of the hard palate - erosion most often takes on an oval shape. The treatment prognosis is favorable if the problem is recognized in time, the traumatic factor is eliminated and antibacterial therapy is started.
Injuries and mechanical damage
Ulcers and erosions occur as a result of accidental biting, blow, bruise or permanent injury from an incorrectly installed filling or crown, or sharp elements of the braces system. If the integrity of the epithelium is not broken, a dark hematoma will appear on the surface of the mucosa - the result of interstitial hemorrhage. If the mucous membrane is damaged, a painful ulcer will appear at the causative site. The injury usually heals quickly on its own. If the scratch does not go away for a long time, it is better to consult a dentist, since there is a risk of infection of the wound and the development of complications.
Ulcers and erosions can occur as a result of accidental injury
Ulcerative-necrotizing gingivostomatitis
The causative agent of infection is anaerobic microflora, which forms on the palatine tonsils, in carious lesions and periodontal pockets. Therefore, this diagnosis often becomes a complication of sore throat, diseases of the upper respiratory tract, and pathologies of the hematopoietic organs. Ulcerative-necrotizing gingivostomatitis also develops against the background of heavy metal poisoning, infection with Koch's bacillus, the development of syphilis, AIDS and cancer.
The photo shows ulcerative necrotizing gingivostomatitis
After the incubation period, the patient is overcome by weakness, his temperature rises, his gums become covered with ulcers, and the mucosal tissues lose their elasticity and become loose. Often with this form of the disease, the lymph nodes become enlarged and painful.
Folk remedies - treatment at home
Traditional medicine is relevant only as an auxiliary therapy; with their help, you can quickly get rid of annoying symptoms and return to normal life. However, even in this case, you should not use certain home recipes on your own - first, consult your doctor and get his consent.
Chamomile decoction helps well in treatment
So, in order to speed up tissue restoration, it is recommended to make applications with rosehip oil and ointments with vitamin A - “Actovegin” or, for example, “Vinizol”. A chamomile decoction for rinsing or a light solution of hydrogen peroxide will help relieve severe inflammation. Tea tree oil has excellent wound healing properties.