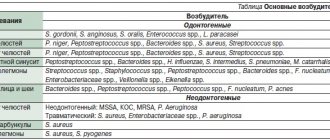
20.01.2017
Upper micrognathia or underdevelopment of the upper jaw is a rather rare type of deformation of the upper jaw, which can be caused by both endo and exogenous factors. Differential diagnosis of this pathology can be carried out in comparison with the false form, the cause of which is excessive development of the lower jaw.
Visually, underdevelopment of the upper jaw has the appearance of a mesial bite. Externally, true micrognathia is manifested by a sharp forward expression of the nose and retraction of the upper lip, and the expression of the nasolabial furrows. At the same time, functional malocclusion is expressed in difficulties in biting off food due to the lack of antagonists. Speech is often impaired. Diagnosis is carried out using tomography of the maxillofacial area.
Anomalies of dental development
The most common anomalies in the structure of hard tissues are systemic or local hypoplasia of permanent or temporary teeth. Systemic hypoplasia looks like a white or yellow spot with a smooth surface. It is impossible to determine it using x-rays. Pits or grooves appear in the image as areas of clearing.
Local hypoplasia develops most often due to injury to the follicle or against the background of chronic inflammation of the periodontium of a milk tooth - in a permanent tooth. Enamel hyperplasia is rare and appears on an x-ray as a more intense, dense shadow.
Mesial bite
Mesial occlusion or, as they also say, mesial occlusion is the second common malocclusion in the sagittal plane. And although mesial occlusion is less common than distal occlusion, there are no fewer questions and controversies surrounding its diagnosis and treatment.
Mesial occlusion is characterized by the fact that the closure of the dentition is visually observed in the so-called third class. When the anterior buccal cusp of the upper molar does not lie in the median fissure of the lower molar, but is located dorsally (posteriorly) from it. And the upper canine is positioned not between the lower canine and the lower first premolar, but also more dorsally. As a result, the normal relationships of the dentition are disrupted.
And we see that the lower row of teeth protrudes forward, more than expected, in relation to the upper teeth. But third grade closure is not a diagnosis. Just as the formulation itself is not a diagnosis - mesial occlusion or mesial occlusion. The closure of teeth, both in the third and, in principle, in any class, is just the closure of teeth. No more. Some external sign. It does not reflect the cause of any anomaly. Moreover, sometimes the closing of teeth even camouflages (hides, hides) the main, usually skeletal, problem. And therefore, just as in the case of treating distal occlusion, or any other problem, you should not make a diagnosis and build treatment tactics only by the type of closure of the teeth. This guideline is extremely unreliable and deceptive. Always and everywhere it is necessary to treat not the “third (or second) class”, but the very cause of the problem that led to this class of closure. Of course, this reason must first be determined. Well, more on that below.
For now, let’s look at the external signs that allow us to suspect mesial occlusion in a patient.
Mesial bite. Signs
At the level of the teeth, as already said, the lower teeth protrude forward in relation to the upper ones. The degree of their “protrusion” can vary from the closure of the upper and lower incisors “joint to joint” (the so-called straight bite)
or a slight “divergence” of the upper and lower incisors along the sagittal, or in other words, in the anteroposterior direction (reverse incisal overlap or reverse bite). Until there is a pronounced non-closure of the upper and lower incisors in the sagittal plane with the formation of a sagittal gap.
Only in this case, unlike distal occlusion, the “components” of the sagittal fissure (upper and lower teeth) have opposite (inverse) relationships. In the case of a pronounced sagittal gap and non-closure of the teeth, the diagnosis will sound like reverse incisal disocclusion (disocclusion - lack of closure). The vertical relationship of the teeth and jaws with mesial occlusion can be completely different: from a pronounced deep bite to, on the contrary, an open bite (vertical non-occlusion of the teeth).
On the face, as a rule, the lower third is enlarged due to the protruding lower jaw, and in some cases, the lower lip. And the upper lip, on the contrary, looks “sunken” (flat) because of this.
Also because of the protruding lower jaw, such a profile is called “energetic” or “masculine”. The most striking representatives of mesial occlusion with strongly pronounced facial signs of this anomaly are members of the Habsburg royal family.
Well, there are genetics, incest and other royal “pranks”... These issues will not be considered in this article... We are talking about other causes of mesial occlusion.
There is also a postural (at the level of posture) sign of mesial occlusion. This is the so-called posterior postural type of posture .
The body needs to somehow align itself in space and maintain balance when the lower jaw is forward. Read more about this in the article “Bite and Posture.”
But despite the general similarity of the external “pattern,” the causes of mesial occlusion can be completely different. Both by the root cause (which jaw, upper or lower, is to blame for the mesial bite), and by the level of occurrence (skeletal or dental).
Dental causes (dental-alveolar forms) of mesial occlusion
Let's start from smallest to largest. From the dental level. When can our lower teeth protrude in front of our upper teeth?
1. The lower dentition is elongated:
A) supernumerary (extra) tooth
B) lower macrodentia: the correlation between the sizes of the upper and lower teeth is disturbed - the lower teeth are larger in size than necessary for the given specific upper teeth
C) other reasons, for example, the tongue is located in the area of the lower incisors and brings them into protrusion (excessive forward tilt), lengthening the lower dentition
2. The upper dentition is shortened:
A) edentia (insufficient number) of upper teeth
Same patient, oral view:
B) upper microdentia: the situation is the opposite of that described in paragraph 1, subparagraph B, and the upper teeth are to blame - they are smaller than necessary for normal sagittal relationships with the lower ones
C) deformation of the upper dentition, its shortening, crowding of the upper teeth
These were “dental” reasons. But, as you know, teeth grow from the jaws. And therefore, the size of the jaws and their relationships, both among themselves and in relation to the skull, can also lead to various types of malocclusion. And mesial occlusion is no exception.
Skeletal forms (causes) of mesial occlusion
Let's consider the jaw (skeletal) causes of mesial occlusion. And I will deliberately start with the jaw... the upper one. Yes Yes. You heard right. In a huge number of cases of mesial occlusion, it is the upper jaw that is to blame. So. What could be the fault of the upper jaw with mesial occlusion:
1. Small, underdeveloped upper jaw. Usually the upper jaw is shortened in the anterior (premaxillary) region. This reason can always be suspected if there is crowding of the upper teeth. Or another indirect sign - the tongue is located behind the lower teeth or is laid between the dentition. Here even the appropriate diction may be “lisping.”
This is understandable: the tongue has no “native” place (on the palate), it finds its home wherever it happens to be.
2. The upper jaw is normal in size, but is in a posterior position. And this happens often. As always, the fault of the jaw lies either in size or position. Let us continue to list the jaw prerequisites for mesial occlusion. But now let’s list when the lower jaw is to blame. 3. Large lower jaw. Moreover, the increased size can be both in the chin and in the posterior segment (all this can be precisely determined by analyzing the lateral TRG according to Sassouni). But the branches of the lower jaw may also be enlarged...
4. The lower jaw is in an anterior position. As a rule, this position is forced. Due to the deformation of the dentition, the upper and lower teeth cannot normally close into a “lock” (it is simply inconvenient for them to close correctly). And the patient is forced to push the lower jaw forward. This very often happens in primary occlusion in children, when the primary fangs, with their sharp ends-tops, create such conditions for the forced position of the lower jaw.
Another reason for the anterior position of the lower jaw is rotation of the temporal bones of the skull. After all, as is known from anatomy, the head of the condyle of the lower jaw is “inserted” into the articular fossa of the temporal bone. And therefore, changes in the position of the temporal bone (articular fossa) affect, among other things, the position of the lower jaw.
And again, as we can see, the problem is either with the size (large) or with the position (front). Moreover, problems with the size and position of both jaws can be combined with each other in completely different variations. This creates, on the one hand, a great variety, and on the other, individuality of forms of mesial occlusion in each specific clinical case. And that is why there are no, and cannot be, universal (for all cases) methods of treating mesial occlusion. Just like any other malocclusion. Everything is decided individually...
By the way, when the jaws “diverge” along the sagittal, the sagittal gap described above does not always occur. Often it is simply absent due to protrusion (tilting forward) of the upper incisors. This is a kind of “dental” compensation for the mismatch of the jaws along the sagittal plane.
Diagnosis of mesial occlusion
The main causes of mesial occlusion were listed above. Both “dental” and skeletal (jaw). It remains only to add that these reasons can be combined with each other, well, in any variations. And these variations... well, count them yourself. Hence the moral: you always need to clearly know what is the cause of mesial occlusion in each specific case. Only then can we answer two original Russian questions: “Who is to blame?” and “What should I do?” Simply put, it immediately becomes clear what to treat and how to treat it. And the answer to this question can be given by analysis of TRG in the lateral projection. Because mesial occlusion is an anomaly in the sagittal plane. Well, analysis of the models, of course (the dental factor cannot be identified otherwise).
Mesial bite. Treatment.
Correction of mesial occlusion. This is where things get really messed up... And why? Because we don’t know how or don’t want to look for (identify) the reason for the teeth closing according to the third class (see above). And we strive to treat mesial occlusion without diagnostics, “by eye.” Relying only on its external manifestations. And that’s why we often “go in the wrong direction.” We are not treating what is needed. And not like that. For example, the upper jaw is short, and the lower teeth .
That's how it is in this case. The patient's mesial occlusion is caused by shortening of the upper jaw. And once, due to its shortening, the upper fangs, not fitting into the dental arch, “stuck out” from above. And the orthodontist removed the top 4 (which in itself is fraught with consequences, see here) to place the fangs. Thus, he “confirmed” and aggravated the shortening of the upper jaw by also shortening the upper dentition. The second orthodontist, when this patient came to him with a third class closure, instead of developing the upper jaw and upper dentition, also removed the lower 4ths. By adjusting the length (and number of teeth) to the defective length of the upper jaw. Thus, further aggravating the situation.
As a result, the teeth seem to be positioned correctly, first class.
But...Is this the result? And can this be called treatment ? Just take a look at the profile.
It is clearly flattened, which does not add aesthetics. The facial profile simply “screams” about the skeletal nature of the anomaly (you just need to be able to see it). So if you carry out a diagnosis, you will not be surprised that this patient needed to be treated not for a mesial bite, but for a distal bite camouflaged by the removal of the upper 4 teeth. This is how it happens...
Alas, this second would-be doctor was once me. Therefore, colleagues, do not step on the same rake, do not repeat the mistakes. Diagnose correctly. And do not treat according to the principle “what we see is what we eat,” basing your conclusions only on how (by what class) the teeth close. Everything is much more complicated and confusing. It’s a pity that you understand this only years later, having gained bitter experience...
How I identify and treat mesial occlusion (and other malocclusions) now is in the article “How this is done in our clinic.”
Or, again, the upper jaw (for example, it is in the posterior position ), and the “large” lower jaw . And she (the bottom one) has nothing to do with it at all.
But everything is simple in reality. Analysis of trg in a lateral projection (I really like the analysis according to Sassouni), competent interpretation of the data obtained - and it’s immediately clear what the reason is. This means that, in principle, there should be no difficulties with how to treat mesial occlusion.
Everything is logical. If the upper jaw is to blame (for example, it is short ), the mesial bite must be corrected by developing (increasing in length) the upper jaw. By the way, with development, the base of the upper jaw (read “living space” for teeth) will increase and their crowding and (or) protrusion will go away. Since both the first and second are options for placing teeth when there is a shortage of space on the jaw (this has been written about in detail here).
There are a great variety of devices for the development of the upper jaw. From a regular orthodontic plate.
Before fixed structures like this:
If you noticed, the patients in all the photos are adults. Not growing. Which, in general, did not affect the result in any way. Although it is clear that mesial occlusion is especially effectively treated in growing patients. In children and adolescents. So, moms and dads, if you notice a mesial bite in a child (the signs are listed above), you shouldn’t wait for the “sea weather” and that “it will go away on its own.” Don't hesitate to contact your orthodontist. After all, mesial occlusion in adults, however, is not treated as “fun” as in children.
If the upper dentition is short (for example, it is shortened due to edentia), then it can also be developed. And space for missing teeth can be obtained. As a result, the length of the upper dentition increases and this may be enough for the overlap of the front teeth to turn from reverse to normal.
If the reason for the shortening of the upper dentition is small teeth (smaller than necessary for a given patient), then the upper dentition should also be developed to the required length. And the resulting gaps can be closed by restoration or prosthetics. When the reason is precisely the violation of the size of the teeth , then the correction of the mesial bite should and is carried out due to the size (its increase) of the crowns of the teeth. Orthodontists should not be alarmed by this. It is better to approach the problem adequately than to try for years to close the gaps by “pulling” teeth with braces. If the problem (gaps between the teeth) lies “at the core” (the initial discrepancy between the sizes of the teeth and jaw, in favor of reducing the size of the teeth), then it is useless to “tighten” anything. All the same, the teeth will “scatter”.
If the upper jaw is normal in size, but is located posterior to the norm , and accordingly, this fact is the reason for the relationship of the jaws in the third class, then the position of the upper jaw must be changed. In other words, “pull it out” to the front. There are so-called face masks for this purpose. Dilyar's mask for example.
Well, a separate article has been written about face masks, their varieties and the nuances of their use (see here). I will only say that I personally use special masks to treat mesial bite. This is also written about in that article.
the lower dentition is to blame for third class occlusion , the logical conclusion suggests itself - to reduce its length. The length of the dentition can be reduced:
1. Distalization (movement back or dorsally) of the entire dentition. If there is somewhere to move, of course. For these purposes (so that there is somewhere to move) you can sacrifice your wisdom teeth. Separation of teeth (lower ones, of course, if we are talking about third class closure)
2. Removal of lower teeth , such as premolars. With further closing of the gaps. Unlike the removal of the upper premolars, the removal of the lower fours or fives does not have such dire consequences for the patient’s health. Provided that normal functional occlusion is formed at the end of orthodontic treatment, of course. And if such removal is justified.
If the lower jaw and its fault is in the anterior position . Here you need to work very carefully and thoughtfully. And not just “push” the lower jaw back, as in this video:
Such manipulations run the risk of driving the lower jaw (or rather, the temporomandibular joint through the lower jaw) into compression and causing TMJ dysfunction. With all the consequences...
In such cases (when there is an anterior position of the lower jaw), it is better to work together with a chiropractor. An osteopath, for example. So that it acts on the temporal bone (and we remember that it is the articular fossa of the temporal bone of the skull that is the natural “refuge” of the articular head of the lower jaw). And displacements (rotations) of the temporal bone (read articular fossa) can affect the position of the lower jaw. Or, if the reason for the forced position of the lower jaw is a block on the teeth (for example, on the primary fangs, as shown above), then this block must be eliminated and the lower jaw must be freed from the “trap” (for example, the same primary fangs must be polished)
Mesial bite. Operation
If the fault of the lower jaw is its large size (like the Habsburgs), then this is the very case when you can think about surgery. Think about it, colleagues. Just think for now. Instead of immediately sending the patient to a surgeon. Even if the “gap” in the jaws in the sagittal plane is very large and surgery is inevitable, the patient must be prepared for surgery for mesial occlusion. And preparation is the task of the orthodontist. Let's not forget about this.
Preparation for surgery for mesial occlusion should consist of a complete selection of all orthopedic (working with the jaws, their size and position) and “dental” capabilities (resources) of the patient. For example, along with an enlarged lower jaw, there may well be an underdeveloped or posteriorly positioned upper jaw. Before an operation to reduce the size of the lower jaw, it would not be a bad idea to develop or “pull” forward this “defective” upper jaw.
Firstly, for surgeons there is a completely different reference point (much more accurate).
Secondly, the patient is completely benefited: an underdeveloped upper jaw is a health problem in itself. Just as the upper jaw, “hammered” back (essentially into the base of the skull), is also a problem.
And thirdly, you have authority: they didn’t just discourage the patient from undergoing surgery, but did everything correctly.
And most importantly, very often in the process of such preparation it is possible to find compromise solutions when the patient, after looking at the result, changes his decision and refuses the operation. There are many such cases in my practice. And I consider this also a successful treatment. It is clear that we are not talking about a centimeter discrepancy between the jaws along the sagittal plane. But there were precedents. Not ideal, of course, in the end (because the “source” is far from ideal), but they refused the operation.
I repeat once again: practically the only indication for surgical treatment of mesial occlusion is the case when the closure in the third class (mesial occlusion) is caused by an increase in the size of the lower jaw. Moreover, the increase is significant, when no orthopedics (non-surgical work with the jaws) will help.
Mistakes in the treatment of mesial occlusion
Consider only the main errors and insinuations. Only those that are “widely distributed” among dentists and patients. Well, about the surgical option (and there are a lot of mistakes in treatment planning), they just talked about (when, in what cases is it appropriate). In the rest - no surgery. No problems with the position of the lower jaw. Neither “third class” problems caused by the upper jaw should be solved surgically. No matter how, all problems of closure in the third class should be solved with braces (or rather, only with braces).
Mesial bite. Treatment with braces
Photo of mesial bite correction with braces:
How many reasons are listed above that lead to teeth closing in the third class? A lot, right? But mesial bite with braces (or rather with the help of braces alone) can be corrected only when the teeth (dentition) are to blame. Or the top one is shortened. Or the lower one is elongated (macrodentia, supernumerary tooth). Those. in a very limited number of clinical cases. How many attempts do we see to cure mesial bite with braces alone? And can't be counted. Yes, take a look at any “bracket bearers” forum. There are dozens of them (if not more). And there are a lot of failures (now I hope it’s clear why). I can tell you from experience: there are an order of magnitude more skeletal causes of mesial malocclusion than “dental” ones. And the critical mass of skeletal causes is a “defective” (in size or position) upper jaw. By the way, have you noticed that in sagittal malocclusions (distal and mesial occlusions) the upper jaw plays a key “causal” role? And there is a reason for this - cranial disorders (but this is a topic for a separate article). But for the majority of us, mesial occlusion is still associated exclusively with a “large lower jaw.” With all the consequences... All errors are due to a lack of understanding of the reasons. And misunderstanding is due to poor diagnosis. Everything is simple, as we see.
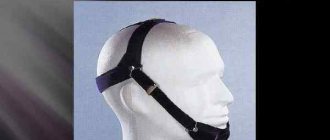
Is it possible to restrain the growth of the lower jaw? Chin sling
The first common innuendo regarding the treatment of mesial occlusion in children is an attempt to restrain the growth of the lower jaw. All these chin slings, face masks and other things that are not very convenient for the patient...
Many people try and hope, but no one has succeeded so far. You can't go against nature. She (nature) will take her course anyway. The bones will grow as much as they are designed to grow. So “containing growth” is absolutely futile. If only because the patient obviously will not wear all these sling masks around the clock (unless, of course, he is also a patient in a psychiatric hospital). So there is no benefit from such actions. Just as there is not and cannot be strict control over the round-the-clock wearing of a face mask or sling. But the harm... The harm can be tangible and real. After all, what happens if we put an obstacle (literally lean on it) on the lower jaw? It, of course, will not stop growing (why suddenly?). But it will begin to rotate (rotate) around a new support point. And here you can easily get an “elongated” face with an open bite. And compression of the TMJ. And other bad things, such as changes in posture, for example (and not for the better, of course). And this is all in addition to the already existing mesial occlusion. In general, the sling clearly poses more problems than it is worth.
And most importantly, sometimes you look, there’s a chin sling. Something like “holds back”. You carry out diagnostics, and the lower jaw is absolutely normal. Both positionally and dimensionally. And the person (patient) suffers. And again, it all comes down to “UNDERDIAGNOSIS.”
Conclusions:
In class 3 closure, skeletal causes than dental ones
If this is so, then it is impossible to treat mesial occlusion in isolation from the “context” (general skeletal problems of the body). See “Bite and Posture” and “The Tale of How Dentists Correct Posture.” And also “How it’s done in our clinic.”
Of the skeletal causes, the upper jaw : either the size is reduced or the position is posterior. In the first case, the upper jaw develops , in the second, it extends forward (a combination is possible, since problems of position and size often coexist peacefully with each other)
Restraining the growth of the lower jaw is a futile task and of little use for facial aesthetics and health in general.
Since dental causes causing mesial occlusion are less common than skeletal ones , in the vast majority of cases mesial occlusion cannot be cured with braces alone . Therefore, correction of mesial occlusion with braces in adults ... is unlikely. And it has little prospects.
Removal of the lower premolars in the treatment of mesial occlusion does not entail such detrimental consequences as the removal of the upper premolars in the treatment of distal occlusion
Surgically, mesial malocclusion is treated only when the lower jaw . And her fault lies specifically in her size - she’s big . There are few Habsburgs among us, frankly speaking (I don’t know whether it’s fortunate or vice versa...)
And one more thing... The main moral. And the only correct logical message (aka conclusion): never neglect diagnostics. First you need to understand the cause of the anomaly. And only then make some efforts to treat (correct) any malocclusion. Only in this case the efforts will not be in vain. And only then can you hope for a positive result.
I hope this article will help my colleagues and their patients in the treatment of mesial malocclusion. I wish everyone good luck! Photos of examples of mesial bite correction (before and after results) can be seen here.
And here you can read an article about distal occlusion.
Why is correct diagnosis of malocclusion important?
- You will understand the essence of the problem with your bite and will know how to treat it - You will not waste extra time and nerves on incorrect treatment - You will not waste money on incorrect treatment - You will not be forced to use unnecessary services
The most accurate diagnosis of mesial occlusion in Moscow with Dr. Filatov
Sign up for diagnostics
Social Like
Comments for the site
Cackl e
Anomalies in the number of teeth
The number of teeth may decrease due to the absence or death of rudiments, or increase. Primary adentia occurs mainly in the permanent dentition. With complete teeth, all teeth are missing; with partial teeth, the upper lateral incisors and lower second molars are missing. This happens with ectodermal dysplasia.
Supernumerary teeth are characterized by an irregularly shaped crown. They erupt for a long time and remain in the jaw. An x-ray - panoramic study - allows you to determine this or that anomaly.
Sometimes a tooth is missing from a row due to retention - retention of the tooth in the jaw bone. It is provoked by its incorrect initial position, lack of space or narrowing of the dentition. X-ray examination allows you to determine the position of the impacted tooth and its relationship with the surrounding anatomical formations. For this purpose, special techniques are used - tomography, oblique projections, etc.
Concept and reasons for origin
The term “small lower jaw” in dentistry and orthodontics has several interpretations with significant differences:
- Micrognathia (also microgenia) is a pathology manifested in the form of defective or delayed development of the entire lower jaw, as well as its individual fragments;
- Prognathia is an intensive growth of the upper part of the jaw apparatus, which results in the visual effect of insufficient development of the lower jaw.
Both pathologies manifest themselves in both infancy and adulthood. Clinical manifestations of the anomaly make it possible to detect the presence of abnormalities at the primary stages of development, which provides the possibility of preventive treatment.
In children
In infancy, improper formation of the lower jaw is caused by various factors, the main one of which is a violation of the uniform process of fetal development in the prenatal period. At this stage, the relationship of jaw proportions is established, which can be influenced by:
- improper maternal diet;
- presence of genetic predisposition;
- consumption of nicotine and alcohol products;
- exposure to serious illnesses with complications.
In the early stages of a child’s life, factors influencing the development of pathology are:
- late formation of bite;
- metabolic disorders in the body;
- early loss of baby teeth;
- bad habits (pacifiers, pacifiers);
- improper feeding.
The primary signs of small lower jaw syndrome in children are recession of the chin and lower lip, abnormal tooth growth and impaired sucking function. Timely identification of symptoms allows the anomaly to be stopped without the use of orthodontic treatment methods.
In adults
In older age, factors provoking the formation of pathology are:
- incorrect or incomplete treatment in childhood;
- receiving severe injuries to the jaw apparatus;
- disorders of the body's metabolic processes;
- pathologies formed in bone tissue (rickets, ostiomyelitis);
- abnormal development of the orbicularis oris muscle.
Characteristic manifestations of small lower jaw syndrome in adulthood are distortion of the patient’s facial features, deformation of the dentition, and problems with eating solid foods.
Anomalies of jaw development
These abnormalities may be congenital or occur after illness, injury, endocrine disorders, or radiation therapy.
- Congenital clefts
of the hard palate and alveolar process are recognized in clinical practice and are often caused by genetic causes. The pathology is often accompanied by dental anomalies, delayed development of permanent dentition, and deformation of the nasal cavity. - Cranioclavical dysostosis
is a congenital systemic disease, which is characterized by changes in the dental system. Due to anatomical pathologies, the upper jaw remains underdeveloped, and the hard palate is shortened; permanent teeth erupt by the age of 20-30, and many of them are impacted, supernumerary and dystopic. - Craniostenosis, or craniofacial dysostosis
, is premature synostosis of the sutures in the bones and base of the skull, when the skull is stretched vertically, intracranial pressure changes, and other pathological processes develop. - Maxillofacial dysostosis
- on X-ray images it is indicated by underdevelopment of both jaws, the zygomatic arch and bone, deformation of the orbits, as well as malocclusion and abnormal development of molars.
There are anomalies of the dental system caused by endocrine disorders. For example, in the category of children with incorrect functioning of the thyroid gland, delayed teething is diagnosed, multiple caries often develops, and underdevelopment of the jaws is also observed.
If there is a history of deficits in the functioning of the anterior lobe of the pituitary gland, the roots of baby teeth may not be resolved, but remain for life, interfering with the eruption of permanent ones. In turn, with hyperfunction of the pituitary gland, the roots grow too quickly, the time for eruption is reduced, and hypercementosis develops at the tips of the roots. Children with Down syndrome begin to erupt primary teeth at 4-5 years of age, but they often do not fall out until 14-15 years of age.
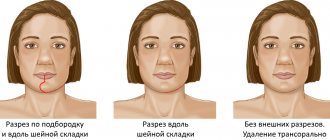
Underdevelopment of the upper jaw - a clinical case
A patient with skeletal asymmetry due to underdevelopment of the upper jaw came to us for further planning of orthognathic double-jaw surgery.
Rice. 1. Photo of the patient. Skeletal asymmetry. Underdevelopment of the upper jaw.
Rice. 2. Intraoral photograph of underdevelopment of the upper jaw.
Cone beam computed tomography (CBCT) was performed with further planning for orthognathic bimaxillary surgery.
Fig.3. Planning for orthognathic double-jaw surgery.
Types, types and forms of deep bite
The type of bite is determined by the level of overlap of the lower teeth:
- Mild degree.
The lower teeth are half visible.
- Average.
The lower teeth are 50–100% invisible.
- Severe degree.
The upper incisors cut into the soft tissue of the lower jaw, completely covering the lower teeth.
There are two types of deep bite:
- Distal.
This is the most common type of deep bite. With it, the lower jaw is slightly shifted back, and the lower teeth are not visible by approximately 1/3. The relationship of the distant teeth is disturbed. The patient has difficulty biting, chewing, nasal breathing, and sometimes experiences pain in the temporomandibular joint.
- Neutral.
With such a bite, the upper incisors also overlap the lower ones by 1/3, but the lateral teeth remain in place and their relationship does not suffer.
There are such forms of deep bite:
- Roof-shaped.
The upper front teeth protrude strongly forward, overlapping the lower ones.
- Blocking.
The upper incisors overlap the lower ones and are inclined backwards.
What happens if you don't correct a deep bite?
Complications of uncorrected deep bite:
- loosening of incisors,
- cracks and chips on the front teeth,
- abnormally rapid and uneven wear of enamel (especially lateral teeth),
- sensitivity of the anterior incisors to cold and food,
- gradual protrusion of the upper incisors,
- wedge-shaped defects.
Such defects appear due to the strong pressure of the lower front teeth on the upper palate.
There are also complications that do not directly affect the condition of the teeth:
- Trauma to the mucous membrane of the palate.
Constant friction of the lower incisors against the upper palate provokes persistent wounds. But the mucous membrane must constantly renew itself, which is why an excessive number of new cells appear. This, in turn, increases the risk of mutations and cancer.
- Disorders of the temporomandibular joint.
The patient can move the jaw limitedly, the muscles are stiff. People often experience pain in this area, hear crunching or clicking noises when chewing, and suffer from migraines. If this is not corrected, over time the patient will experience degenerative processes in the joint.