Maxillofacial phlegmon: causes and dangers
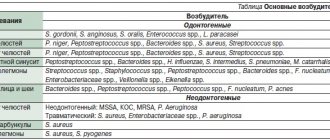
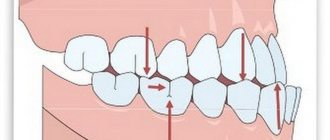
The vast majority of phlegmons (more than 90%) are odontogenic in nature, that is, they arise due to a tooth that is not treated in time, destroyed by caries or periodontitis. The causative agents of inflammation - staphylococci, streptococci, anaerobic and putrefactive microorganisms - penetrate from the affected tooth root into the tissues of the perimaxillary region due to the peculiarities of the outflow of lymph and venous blood. Another difference between phlegmon and an abscess is that it develops against the background of a significant decrease in immunity, while an abscess can form in a patient with normal protective reactions of the body.
Cellulitis of the maxillofacial area is a dangerous condition that requires serious surgical intervention. The severity of the patient’s condition is determined by the degree of neglect of the process and general intoxication of the body. In addition, nerve endings are concentrated in the jaw area, so a diffuse purulent inflammatory process brings unbearable pain and physical suffering to a person. Vital functions are impaired - swallowing, chewing, speaking, breathing. And a large number of venous plexuses favors the rapid spread of the process and its transition to vital organs and systems. The most severe complications of this disease:
- phlebitis;
- thrombophlebitis;
- mediastinitis,
- abscesses of internal organs;
- meningitis;
- meningoencephalitis;
- sepsis.
Cellulitis is especially severe in children or if it is caused by anaerobic microorganisms.
Prevention methods
Cellulitis, like any other disease, can be prevented. It is especially important to follow preventive measures for people who are at risk, with medical diagnoses such as HIV, AIDS, tuberculosis, and diabetes. The main prevention is to prevent skin injuries.
If there are purulent foci in the body, especially in the oral cavity (caries, purulent abscesses on the gums), they must be treated in a timely manner, preventing further development and rupture of purulent foci. If the skin is injured, the cut sites must be immediately treated with antiseptic solutions. You need to be especially careful when preparing fish. A bone injection can lead to the development of erysipelas, which, against the background of a weakened immune system, carries the risk of phlegmon formation.
Considering the rapid development of purulent inflammation, it is necessary to consult a doctor immediately if the skin at the site of the cut becomes red within 24 hours, the area around the wound begins to swell, hurt, a fever appears, and the temperature rises.
Traditional medicine methods can only be used with the permission of the attending physician, with an accurately established diagnosis. As a rule, various decoctions based on medicinal herbs are used in the form of compresses during the rehabilitation period and only as an additional means for faster healing.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Symptoms
Phlegmon of the perimaxillary region, unlike an abscess, develops rapidly and is characterized by severe intoxication. Its main clinical manifestations:
- infiltration on the affected area of the face or neck;
- hyperemia, swelling, soreness of the skin at the site of inflammation;
- high body temperature;
- rapid pulse;
- severe pain when chewing, swallowing, talking;
- spasm of the muscles responsible for opening and closing the mouth (trismus);
- increased salivation;
- weakness;
- chills;
- pale skin;
- loss of appetite;
- sleep disorders;
- enlargement of regional lymph nodes;
- facial asymmetry.
Periandibular phlegmon, photos of which can frighten impressionable people, is always accompanied by an increased number of leukocytes and neutrophils in the blood, a shift in the leukocyte formula to the left and an increased ESR value. The diagnostic sign of phlegmon in the blood serum is C-reactive protein. Protein and white blood cells also appear in the urine.
Boundaries of the pterygopalatine fossa : anterior - posterior surface of the body of the upper jaw and the orbital process of the palatine bone; posterior - the pterygoid process of the sphenoid bone, internal - the vertical plate of the palatine bone, upper - the lower surface of the body and the base of the greater wing of the sphenoid bone, the greater wing of the sphenoid bone.
Topography of the pterygopalatine fossa.
1 - pterygopalatine fossa; 2 - pterygoid process of the sphenoid bone; 3 - tubercle of the upper jaw. (From: Sinelnikov R.D. Atlas of Human Anatomy. - 1996. - M., T. 1 with changes).
The projection of the pterygopalatine fossa onto the skin is an equilateral triangle, the base of which is the middle third of a line drawn along the upper edge of the zygomatic arch from the upper edge of the tragus of the ear to the outer corner of the eye. From this line downwards at an angle of 60″, two of its sides are built.
Projection of the pterygopalatine fossa onto the skin
The pterygopalatine fossa lies in the depths between the upper jaw and the pterygoid process inward of the infratemporal fossa. The pterygopalatine fossa is connected to the infratemporal fossa by the falciform fissure. The pterygopalatine fossa communicates with the orbit through the inferior orbital fissure; with the nasal cavity - through the sphenopalatine foramen, which is located on the medial wall of the pterygopalatine fossa; with the oral cavity through the greater palatine canal, which opens with the greater and lesser palatine foramina; with the middle cranial fossa - through the round foramen; with the outer base of the skull - through the pterygoid canal. The main sources and routes of infection : foci of odontogenic infection in the area of large molars of the upper jaw, infection during tuberal anesthesia. Secondary damage as a result of the spread of infection along the extension from the pterygomaxillary space, from the temporal, buccal, parotid-masticatory areas. Objectively : the face is asymmetrical due to moderate swelling of the tissues of the lower eyelid. Hyperemia of the mucous membrane of the vault of the oral vestibule is determined. On palpation, an infiltrate is noted in the posterior part of the arch of the vestibule of the mouth behind the tubercle of the upper jaw, which is sharply painful. Mouth opening is moderately limited.
Appearance of a patient with phlegmon of the pterygopalatine fossa.
Ways of spread of infection: scales of the temporal bone, meninges, brain; orbit, dural sinuses, brain; pterygomaxillary space, peripharyngeal space, anterior mediastinum. The infratemporal fossa (fossa infratemporalis) is located deeper than the parotid-masticatory region . The boundaries of the infratemporal fossa: anterior - the tubercle of the upper jaw and the lower part of the temporal surface of the zygomatic bone, posterior - the styloid process of the temporal bone with the muscles extending from it and the anterior surface of the condylar process of the lower jaw; the outer is the inner surface of the branch of the lower jaw, the inner is the outer plate of the pterygoid process of the sphenoid bone, the upper is the crest of the greater wing of the sphenoid bone. On the inferomedial side, the infratemporal fossa is limited by the medial pterygoid muscle, which starts from the pterygoid fossa and attaches to the inner surface of the angle of the mandible. In the infratemporal fossa of the deep region of the face there are the lateral pterygoid muscle, the maxillary artery, the pterygoid venous plexus and branches of the mandibular nerve. The infratemporal fossa communicates medially with the pterygopalatine fossa. There are no anatomical structures separating these two spaces.
Topography of the infratemporal fossa.
1 - infratemporal crest; 2 - infratemporal fossa; 3 - pterygoid process of the sphenoid bone; 4 - tubercle of the upper jaw. (From: Sinelnikov R.D. Atlas of Human Anatomy). The main sources and routes of infection : foci of odontogenic infection in the area of 18,17,27,28 teeth, infection during tuberal anesthesia. Secondary damage as a result of the spread of infection along the extension from the pterygomaxillary space, from the temporal, buccal, parotid-masticatory areas. Objectively : the face is asymmetrical, the skin is hyperemic. Local signs of inflammation are very clearly revealed when examined from the oral cavity in the form of smoothness of the posterior fornix of the vestibule of the mouth, hyperemia of the mucous membrane. On palpation, an infiltrate is determined behind the tubercle of the upper jaw, which is sharply painful. Hyperemia of the mucous membrane of the vault of the oral vestibule is determined. Mouth opening is moderately limited. With phlegmon of the infratemporal and pterygopalatine fossae, in most cases an infiltrate is detected in the area of the transitional fold of the superoposterior part of the vestibule of the oral cavity; with phlegmon of the temporal region, this symptom is absent.
Appearance of a patient with phlegmon of the infratemporal fossa.
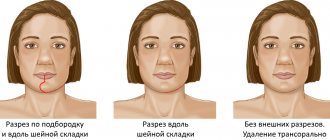
Routes of infection spread : temporal, parotid-masticatory areas, pterygomaxillary and peripharyngeal spaces, pterygopalatine fossa, orbit, dural sinuses, brain. Technique : for isolated lesions of the infratemporal and pterygopalatine fossae, an intraoral incision is used in the upper arch of the vestibule of the mouth slightly below the transitional fold of the mucous membrane at the level of the last two molars.
Scheme of the intraoral method of opening an abscess, phlegmon of the pterygopalatine and infratemporal fossae
Next, using a rasp, peel off the upper edges of the wound from the tubercle of the upper jaw and, with a curved clamp, bluntly pass behind the tubercle of the upper jaw into the pterygopalatine and infratemporal fossa to the place of accumulation of pus. The operation is completed by draining the abscess by introducing rubber glove graduates through the surgical wound in the mouth. An intraoral incision is rarely used. Phlegmon of the infratemporal fossa is usually combined with damage to the cellular spaces of adjacent anatomical areas. In such cases, drainage of the infratemporal cellular space is carried out from the operational access used to open the phlegmon of neighboring interested areas, i.e. external incisions.
“Operative surgery of abscesses, phlegmons of the head and neck,” Sergienko V.I. et al. 2005
You might be interested in:
- The following boundaries of the parotid-masticatory region are distinguished: upper - lower edge of the zygomatic arch and part of the temporal bone with the external auditory canal, lower ...
“>Abscesses and phlegmons of the parotid-masticatory area
- Borders of the infraorbital region: upper - lower edge of the orbit, lower - alveolar process of the upper jaw, outer - vertical line, drawn ...
">Abscesses and phlegmons of the infraorbital region
- The boundaries of the orbital area correspond to the walls of the orbital cavity with its contents. Walls of the orbital cavity: superior - orbital surface of the frontal co...
">Abscesses and phlegmons of the orbital area
- Borders of the buccal region: upper - the lower edge of the zygomatic bone, lower - the lower edge of the lower jaw, posterior - the anterior edge of the masticatory muscle, anterior ...
">Abscesses, phlegmon of the buccal area
- Opening an abscess, phlegmon of the pterygomaxillary space. The pterygomaxillary space is located between the inner surface of the branch of the…
“>Abscesses, phlegmons of the pterygomaxillary space
We recommend reading:
- Borders of the temporal region: superior and posterior - temporal line. lower - zygomatic arch, in front - zygomatic process of the frontal bone Borders...
“>Abscesses and phlegmons of the temporal region
Treatment
Despite the severity of the disease, in general, with timely treatment, perimandibular phlegmon has a favorable prognosis. Treatment is carried out only in a hospital setting, but at the initial stage everything is often limited to the use of conservative methods - antibiotic therapy, the prescription of restoratives, vitamins, and a special diet. But if the process has already started and the spread of infection is observed, complex surgical treatment is indicated, which includes the following points:
- opening the inflammation site under general anesthesia;
- cleansing the wound from pus;
- installation of drains for drainage of wound contents;
- daily treatment with bactericidal solutions;
- powerful antibiotic therapy - often a complex of several drugs is prescribed;
- detoxification of the body;
- use of antipyretic and painkillers;
- prescription of immunomodulating, restorative agents, vitamins;
- physiotherapy – ultraviolet irradiation, UHF, magnetic therapy, etc.
If treatment is successful and there are no complications, the patient’s recovery occurs on average in 14-21 days.
Putrefactive-necrotic phlegmon of the mouth, or Ludwig's angina
This pathology is similar in appearance to the previous disease, but its main difference is that with soft tissue necrosis there is no accumulation of pus. Symptoms of Ludwig's angina are very specific. This disease carries a huge danger, since sepsis can develop if you do not consult a doctor in a timely manner. Fortunately, the incidence is very low.
The specificity of Ludwig's angina is that basically only the muscles are the main point of damage. The perimuscular tissues may be in a state of inflammation, but it is the muscles that take the main “blow”. Their consistency becomes very dense and woody.
With this disease, patients complain of headaches and high fever. Moreover, in the first two days it may not reach high levels. However, every day the patient gets worse. Externally, a person’s face looks asymmetrical, the chin and neck are swollen. It is impossible to remove the tongue inside as the swelling prevents this from happening. There is a putrid odor and abundant gas formation from the source of infection.