The working length of the root canal is the distance from the end point at the apex to the external landmark chosen by the doctor (tubercle, filling on the coronal part).
Doctors still cannot come to a consensus and say what should be taken as a guide: the physiological foramen (the transition of root cement into dentin), the apical foramen (the hole itself), the radiographic apex (the most distant point on the image) or the anatomical apex (the most distant area from the crown). The distance between them is up to 2 mm, and this is the difference between a well-sealed canal and the preservation of a source of infection.
The most important task is to find this end point, which is complicated due to the large number of different anatomical structures.
There are 4 methods for determining the working length of the root canal:
- x-ray
- tactile
- using an apex locator
- tabular
X-ray
The doctor determines the radiological apex from the image and the working length of the root canal is set 1 mm before it. The problem is that the channel is a three-dimensional structure, and the image is presented to us in a two-dimensional projection. There are cases when the doctor perforated the canal wall, while on the x-ray everything looks within normal limits. In almost 50% of all cases, the instrument is deeper than it appears in the photo.
Treatment of canals using chemicals
Chemical treatment is used when mechanical cleaning is not possible. Usually the procedure is performed using chemicals when the canals are too narrow or completely impassable. After chemical treatment, mechanical treatment can be carried out.
Previously, nitric and hydrochloric acids were used for the procedure. But later they abandoned these substances, since they burned the surrounding tooth tissues when they got on them. Today, calcium salts and chelating agents are used. They can be in liquid or gel form. Solutions of calcium salts penetrate well into narrow channels. The advantage of these substances is their antiseptic property. In addition, they contain EDTA, which provides good glide for instruments. Chemical treatment is carried out in several stages:
- The cavity in the tooth is thoroughly dried.
- A solution is placed in it and injected.
- After penetration of the chemical, the channel is expanded mechanically.
Solutions do not have a negative effect on surrounding tissues. Drugs must meet the following requirements:
- Have a bactericidal effect.
- Do not damage surrounding tissues upon contact.
- Do not cause allergies.
- Do not cause resistance in microorganisms.
- Have a quick effect.
- Be active in the presence of organic compounds.
- Do not have a strong odor.
Today it is almost impossible to select a substance that will meet all of the above requirements. The most popular drug used in dentistry for root canal treatment is sodium hypochloride. It is effective, has broad bactericidal activity, thanks to which it protects the tooth from various microorganisms.
After the treatment, filling is performed. For this purpose, high-quality materials are also selected that will retain their shape and volume in the canal cavity. This property will provide reliable protection against bacterial infection.
Tactile method
The least reliable option for determining the length of the root canal, the quality of such diagnostics depends on the doctor’s “insight” and his experience, which, you see, is an unacceptable argument. A thin instrument is inserted into the canal and the location of the hole is determined by touch. Another method is to use a paper point. Where it is saturated with blood or other contents is considered the exit point. If not a small part, but a significant area is saturated with blood, then it should be concluded that it has gone beyond the apex. This can also include pain. When the instrument goes beyond the top, the patient feels a prick, which is what the doctor focuses on.
The length of the canals of the teeth of the upper and lower jaw
To carry out high-quality endodontic treatment, it is important to know the length of the dental canal. The length of the tooth canals (the table below) depends on the size of the tooth itself. Determining such parameters is possible in several ways.
The initial preliminary assessment is carried out in a tabular manner (average canal length and its variability in mm depending on the tooth formula):
Sometimes the length of the tooth canals can be determined from an x-ray, but the x-ray image in most cases does not reflect the true size.
With an accuracy of 60-97%, the length is determined electrometrically (by changes in the electrical resistance of tissues) using an apex locator.
The tactile method is based on slowly immersing the probe into the canal until it jams.
According to the patient’s sensations (a slight “prick” when moving the instrument past the root apex), during treatment without anesthesia, the length of the canal is also determined approximately.
Using a combination of several approaches is effective.
Apex locator
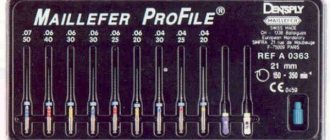
The electronic method is considered the most reliable of all mentioned. The most popular brands of devices are: Russian Geosoft (EndoEst), Japanese NSK (iPex), German VDW (Raypex).
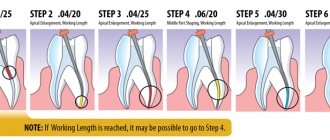
Determination of the working length of the root canal:
- one wire with a hook at the end is hung on the patient’s lip
- diagnostic tool (for example, K-file) is installed in the holder
- then the doctor slowly moves it along the canal; numbers are displayed on the device screen indicating how much is left to the top. An intermittent beep will also sound. Some models have a graphic display: green - far, yellow - close, red - in place
- When the instrument reaches its destination, APEX will appear on the screen and the alarm will beep continuously.
Determination of the working length of the root canal
Back in 1965, Seltzer and Bender showed that the quality of endodontic treatment depends on three mandatory components - thorough cleaning of the canal, sterilization and its complete obturation. The basis of successful endodontic treatment is the correct determination of the working length of the root canal. If this stage of treatment is neglected, it becomes impossible to carry out all subsequent stages in a high-quality manner, and as a result, the quality of the entire endodontic treatment is significantly reduced.
The working length of the root canal is the distance between the external landmark on the tooth crown and the apical border. In the anatomy of the apex, three structures are important: the apex proper (radiographic apex), the large apical foramen, and the apical constriction. The apical constriction zone is recommended as the physiological apical level for instrumentation and root canal filling. The apical constriction is the area of the apical part of the root canal with the smallest diameter (Ricucci & Langeland 1998). Microscopic and morphometric studies of root canals have shown that, as a rule, the apical narrowing does not coincide with the dentino-cemental boundary, as previously thought. From the apical constriction to the large apical foramen, a funnel-shaped expansion of the root canal occurs, which is not possible to carefully treat. According to a number of authors, in 75% of cases the apical foramen is deviated from the main axis of the tooth. This means that the radiographically determined apex and apical constriction are often located at different levels, so serious inaccuracies can arise when using radiographs alone to determine the working length of the root canal.
There are several methods for determining the working length of the root canal: tabular, tactile, radiological, red dot (paper point) method, patient reaction, electronic (using apex locators)
According to statistics, during the initial passage of the root canal, the dentist can tactilely determine the apical constriction in 75% of cases. When treating non-vital teeth, one can additionally be guided by the patient’s reaction to the advancement of the instrument in the root canal. When reaching the apical foramen, the patient feels a slight prick.
One of the popular methods for determining working length is x-ray. In this case, control radiographs are taken at the stage of endodontic treatment with the instrument inserted and during the process of filling the root canal. However, the position of the apical constriction varies significantly and may change depending on the patient’s age, parafunction of the masticatory muscles, apical resorption and other factors. According to histomorphometric measurements carried out by Dummer et al. (1984), the average distance between the apical constriction and the anatomical tip is 0.51 mm. In more than 92% of cases, the apical narrowing is 0.5 mm from the anatomical and 1.0 mm from the radiographic apex. Based on the anatomy of the apex, researchers recommend root canal treatment 0.5-2 mm from the radiographic apex of the root, since the zone of apical constriction is in this range with the greatest statistical probability. The radiograph is a two-dimensional image and does not reproduce the entire anatomy of the apical part of the root; layering and distortion of the image are often noted. Chunn et al. (1981) found that 43% of the files found at the apex on radiographs were actually located behind the apex (in the periodontium). When interpreting radiographic data, a potential error is the subjectivity of the investigator. Therefore, it is not advisable to be guided only by this method of determining the working length.
During the process of drying the root canal, blood on a paper point can also help determine the working length (red dot method). Blood on the tip of the paper point indicates excessive expansion of the apical foramen and extension of the instrument beyond the apex. The size of the blood spot corresponds to the length by which the working length of the canal should be reduced. This method is also not objective and depends on the characteristics of the clinical situation.
The apex location method is based on the constancy of electrical resistance of tissues. Since the hard tissues of the tooth have a higher resistance than the mucous membrane of the oral cavity and periodontal tissue, the electrical circuit between the electrodes placed on the lip and in the canal remains open until the file reaches the periodontal tissue. Apex locators of the first generations worked only in a dry and clean channel and determined the strength of direct current. Starting from the third generation, apex locators determine impedance using alternating currents of different frequencies (starting from 5 frequencies of apex locators of the 3rd generation, to dual-frequency apex locators of the 5th generation). The impedance is lowest in the region of apical constriction and greatest in the region of the greater apical foramen. Thus, all modern apex locators measure precisely this point of drop in resistance. Therefore, no apex locator can measure the length of the root canal, we cannot get a metric result even if the apex locator has a millimeter scale.
The fifth generation apex locators include Raypex 5 (VDW). Raypex 5 features digital impedance measurement technology, clear LCD color display and improved measurement accuracy. The device runs on battery power.
The lip electrode is attached to the lip opposite the tooth being examined. The root canal should be moist, but excess fluid in the tooth cavity is undesirable. The doctor can observe the progress of the file on the device display. Once the file reaches the apical third of the canal, an enlarged image of the apex appears on the screen indicating the position of the file in relation to the apical foramen. A graphical representation of the position of the instrument apex is accompanied by a sound signal of varying intensity depending on its approach to the apex.
In the image of the apical third of the canal, several segments of different colors are highlighted: green indicates the zone of apical constriction, yellow indicates the large apical foramen, red indicates the instrument extends beyond the apex, and a continuous sound signal is heard. As a rule, for vital teeth, it is recommended to treat the root canal to the green zone. In the case of non-vital teeth and periodontitis, it is recommended to treat the root canal to the yellow area. Thus, an enlarged image of the apical part of the root canal with graduated sections allows the dentist to decide at what level to complete the canal treatment. In addition, the dentist can independently set the so-called “virtual apex” - a point in the apical zone, upon reaching which the frequency of apex locator sound signals will sharply increase.
An additional advantage of working with the Raypex 5 apex locator is the presence of a demo mode, which allows you to quickly master working with it, as well as explain the principle of operation to the patient. In addition, the convenient folding body allows for easy viewing of the display from any angle.
The undoubted advantage of measuring the root canal using an apex locator is its significantly greater accuracy compared to that using radiography. Studies evaluating apex locators have shown an accuracy of determining the working length within 0.5 mm of the apical foramen in 75 - 93.4% of cases.
Errors in determining the working length of the root canal using an apex locator can be associated with contact of electrodes with metal structures in the oral cavity, the presence of perforation, a broken instrument, an open apex or apical resorption, the presence of a large amount of liquid in the tooth cavity, as well as when the battery charge is less than 50 %.
Examination of the length of the root canal with an apex locator in combination with x-ray examination is the most complete. You cannot completely trust only one method for determining working length. It is advisable to combine several methods at once.
Bibliography:
- Barer G.M., Antanyan A.A. Objectification of the clinical and laboratory method for studying apex locators / “Cathedra”, No. 7, 2003
- Dr. Ben Johnson How far do you want the root canal to go: just below the apex, just at the apex, or beyond the apex? / Dentsply News No. 12 / March 2006
- R. Beer, M. Bauman, S. Kim Endodontology - M, 2004
- S. Cohen, R. Burns Endodontics - St. Petersburg, 2000
- Smirnova M. A., Shpak T. D. Modern technologies in endodontics. Atlas-review - St. Petersburg, 2007
- Harald Schlepper Accurate length determination / DPRE, march 2007
- Harald Schlepper Was ein moderner apexlocator kann / Newsletter, No. 2, 2008
- KT Wrbas, AA Ziegler, MJ Altenburger & JF Schirrmeister In vivo comparison of working length determination with two electronic apex locators / International Endodontic Journal, No. 40, 133–138, 2007
- Kumar S.S. et al. A simple model to demonstrate the working of electronic apex locators / Endodontology, Vol. 16, 2004
- R. Mounce Determination of true working length / Endodontic practice, March 2007, p. 17-19
Article provided by Pharmgeocom LLC
Table method
Over a long period of clinical observations, doctors have accumulated an extensive database on the working length of root canals. So, if there are no other options, you can take a conventional cutter and check the readings in the table. If there is no apex locator and x-ray, then this method should be supplemented with tactile. However, the anatomy of each person is individual, so the reliability of the table values is also not high.
So what is the most effective method for determining the working length of a root canal?
Alas, there is no one ideal technique. At the moment, it is customary to rely on the “apex locator + x-ray” combination.
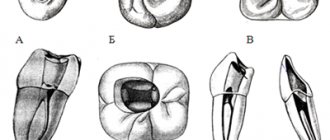
How many canals are there in the 5th, 6th, 7th and other teeth of the upper and lower jaw, what is the length
Teeth differ from each other in shape, structure, and number of roots.
The space inside the root is called the root canal. The number of roots has a relationship with the load that falls on the tooth, but the number of canals in the tooth does not have a direct relationship with the number of roots. And even in the same tooth, the number of canals may vary among different people. The key to high-quality endodontic treatment is the accurate determination of the tooth canals: their number, length, shape.
Typically, the deeper a tooth is in the mouth, the more canals it has. The number of canals in the teeth of the upper and lower jaws differs: the upper teeth have more of them.
A preliminary assessment of the number of canals in a tooth is carried out according to the table (the probability of a certain number of roots depending on the location of the tooth):
Thus, the canals of the 24th tooth (the left quad in the upper jaw) in 85% of cases are determined by the number 2. That is. This tooth usually has only two canals. But 9% of people can only have 1 channel, and 6% have 3 channels. On the other hand, the “seven” of the lower jaw most often (77%) has 3 canals in the teeth. We can judge with the greatest confidence how many canals there are in the front tooth on the upper jaw - only 1.
It is statistically impossible to answer the question of how many canals there are in a wisdom tooth: for the upper ones, the number varies from one to five, for the lower ones – about three.
The exact number can only be found out when opening the tooth or based on the results of radiography (targeted, for a specific tooth, or orthopantogram, to assess the condition of all teeth).
Paper point method
This method is based on moistening the paper point while slightly extending it beyond the working length of the root canal. When the paper point is in a dried canal and does not reach the apical foramen, it is removed dry. If a paper point inserted into a dry canal passes through the apical foramen, it will be withdrawn with fluid (blood, pus, serum, mucus) on the part of the post that has protruded beyond the canal. Under the influence of capillary forces, the liquid will move higher, and the level of moisture in the pin will spread to the part that is not in contact with the liquid.
Technique
Insert a paper point into the dried canal 0.5 mm shorter than the working length determined by the electronic apex locator. If the pin is dry when removed, you need to push it deeper into the canal until it reaches the liquid, and then mark the length of the dry part of the pin. Next, take a pin of shorter length than the one marked and check it. To prevent the appearance of capillarity, the pin should not remain in contact with the canal walls for too long.
Flaws:
- Inflamed, altered, enlarged and bleeding root tip;
- Care is required to remove the pin in time before it becomes too wet;
- Moistened apex.
Tips and Tricks
- Always measure working length on preoperative radiographs;
- Check the working length at all stages of endodontic treatment: from exploration to glide path creation and canal formation. The more curved the channel, the greater the tendency to reduce the working length;
- Carry out preliminary passages of channels;
- Be alert to the presence of metal restorations, which may cause false apex locator readings;
- Determination of the working length should be made gradually using the apex locator scale;
- The device must have close contact with the canal walls for correct interpretation; in the presence of wide canals, larger files are used;
- Do not measure the device readings when the channel humidity is high.
The translation was made specifically for the
Stomatologija forum. su. Please, when copying material, do not forget to provide a link to the current page.
Patency of dental canals
In addition to the number and length, important information is the patency of the root canals, which depends on the degree and location of the curvature. If the curvature is less than 25 degrees, then the canal is instrumentally accessible, from 25 to 50 degrees it is difficult to access (the so-called difficult tooth canals), and over 50 degrees it is inaccessible. When the curvature is localized near the mouth of the canal, it is possible to expand the latter and improve patency.
If the examination reveals a too narrow, deep canal in the tooth, a CT scan may be required to clarify its configuration. Treatment of complex teeth requires particularly painstaking work, which can be made easier with the help of a microscope.
Sometimes the doctor cannot find the canal in the tooth. This situation is usually associated with obliteration (narrowing or overgrowing) of the canals due to an inflammatory or tumor process, incorrect treatment in the past, or age-related changes.
Remember that only a specialist can assess the condition of the root canals and, depending on their structural features, determine treatment tactics.
Periodontal Sensitivity Method
This method is based on the patient's pain response when the K-file reaches working length and touches the periodontal tissue.
Flaws:
- Any method based on the patient experiencing pain is not an ideal solution.
- Difficult interpretation in the presence of tissue inflammation - hydrostatic pressure created in the canal can cause unexpected moderate to severe pain. In this case, when pain occurs, the tip of the file may be a few mm away from the apical constriction.
- A difficult interpretation in the presence of tissue necrosis is that the K-file exiting the canal and passing through the apical foramen may not cause any unpleasant or painful reactions. This happens especially often with periapical lesions, since tissue vascularization is reduced. However, vital pulp may remain in the most apical part of the canal, even in the presence of extensive lesions.
X-ray method
This technique is based on the preparation of the root canal and its obturation at the level of the radiographic apex.
Advantages:
- The determination is not random, subjective or statistical;
- Easily recognized on a correctly taken intraoperative x-ray;
- In 50% of cases, the canal ends at the level of the anatomical apex, which is clearly visible on the radiograph;
- In the case where the canal ends lateral to the geometric root apex (M/D), the radiographic method is also effective.
Flaws:
- If the apical foramen is displaced in a different direction, this is not noticeable on the radiograph, then instrumentation at the level of the radiological apex leads to exit beyond the root canal;
- The 2D image reduces or flattens the buccolingual dimension;
- The effect of a minimum dose of radiation, which is unacceptable during pregnancy;
- Difficulty in performing in some patients;
- Image overlay in multi-rooted teeth and with complex anatomical structure.