Obliteration - the word comes from the Latin “Obliteratio” (destruction).
In dentistry, this term refers to a pathological process during which the cavity or the entire root canal of a tooth begins to narrow or completely overgrow. As a result, it is less resistant to infections and more difficult to respond to endodontic treatment.
Dentists name several main causes of obliteration:
- Overgrowth of connective tissue, which leads to thickening of the walls.
- The presence of inflammatory processes,
- The presence of cancer, during which tumor growth occurs.
- Body changes associated with age.
- Consequences of poor quality treatment.
There are also several factors that lead to the accumulation of calcium salts in the tooth cavity. After which the patency of the tooth pulp and root canal is impaired.
Causes of obliteration of tooth canals
The main and most common causes of tooth root obliteration are:
- injuries;
- chronic inflammatory processes;
- age-related changes;
- poor quality treatment;
- the presence of cancer associated with the proliferation of connective tissue.
There are also factors that increase the likelihood of root canal obliteration. These include:
- malocclusion;
- heredity (in particular with marble disease and Stanton-Capdepont syndrome);
- metabolic and endocrine system disorders;
- exposure to chemicals on teeth over a long period of time;
- decreased functionality or inactivity of the tooth during chewing.
Cost of endodontics
| Name of service | Cost, rub. |
| Intracanal procedure for the treatment of pulpitis | |
| with root canal filling with pastes (for one canal) | 2500 |
| with root canal filling with gutta-percha (for one canal) | 2750 |
| Mechanical and medicinal treatment of one canal | 1320 |
| with root canal filling with thermoplastic gutta-percha Beefil, Termofil (for one root canal) | 2750 |
| passage of the obliterated canal | 2000 |
| use of the drug "Metapex" for 1 channel | 1650 |
| laser processing of 1 channel | 1200 |
| EDI (determination of pulp viability) | 400 |
| Removing a foreign body from the canal | 4150 |
| Intracanal procedure for the treatment of periodontitis | |
| with root canal filling with pastes (for one canal) | 2500 |
| with root canal filling with gutta-percha (for one canal) | 2750 |
| Mechanical and medicinal treatment of one canal | 1320 |
| with root canal filling with Beefil thermoplastic gutta-percha (for one root canal) | 2750 |
| Passage of the obliterated canal | 2000 |
| Use of the drug "Metapex" | 1650 |
| Laser treatment of one channel. | 1200 |
Obliteration of root canals. Clinical case.
A patient contacted us. The orthopantomogram image clearly shows complete obliteration of the lumen of the root canal of the 21st tooth.
Fig. 1 Complete obliteration of the root canal of the 21st tooth on an orthopantomogram
Diagnosis was made using cone beam computed tomography (CBCT).
Rice. 2 Sagittal section of the area of the 21st tooth on a CBCT image
Taking into account the skeletal asymmetry of the lower jaw in the image, the main cause of obliteration of the root canal in this case can be assumed to be trauma.
Rice. 3 Axial section of the upper jaw area with obliteration of the root canal of tooth 21
Treatment methods for root canal obliteration
Treatment of a tooth with root canal obliteration is quite difficult. Most often, in such cases, surgical removal of the part of the tooth affected by the pathological process is used, as well as chemical devitalization, in which tissue mummification is performed using special injections.
Treatment of root canal obliteration is a rather painful procedure, since due to the obstruction of the tooth patency, injection anesthesia is ineffective. The complexity of treatment causes the possibility of complications. These include perforation of the root canal and/or dental crown and possible pain due to incomplete elimination of canal obstruction.
Posted in Articles | Tags: 3-D CT, clinical case, CBCT
New technologies for problematic channels
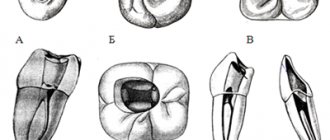
Pulpitis and periodontitis are still the main reasons for tooth extraction. Teeth with elements of destruction at the root apex are foci of chronic infection, sometimes leading to systemic diseases. Many authors attribute the presence of additional unopened canals and great difficulties in monitoring the passage of the canal and its filling as reasons for the low quality of canal sanitation. Back in 1970, Mayer presented reconstructed models of tooth roots, which show how many lateral branches a root canal can have and how extensive the apical delta can be (Fig. 1).
Currently, more and more supporters are gaining the point of view that modern instrumental-mechanical endodontics is fundamentally unable to solve the problems of combating root infection.
Fig. 1 Variants of the apical delta of root canals
Fig. 2 Cross sections of teeth showing difficult canals
By measuring electrical conductivity with the main hole well open and carefully insulated with varnish prof. A. Knappvost revealed that 70-90% of the flow of substances entering the pulp passes through the lateral (!) canals of the apical delta. The work of Noldin (1994) shows the shapes of channels that are poorly accessible to mechanical instruments (Fig. 2).
At the same time, only complete sterility of the entire canal system is a prerequisite for effective sanitation.
Based on the previously known methods of electrophoresis and iontophoresis of Prof. A. Knappvost has developed a technology for successfully resolving endodontic problems using a unique technology of depophoresis of a substance new to dentists - an aqueous suspension of copper-calcium hydroxide, which has exceptional bactericidal and physicochemical properties.
During treatment under the influence of an electric field, from the depot of the above-mentioned suspension created in the root canal, OH-ions and hydroxycuprate ions [Cu(OH)], which have a strong bactericidal effect, penetrate into the entire canal system, including secondary and lateral canals, up to the openings.
As a result of this, the following processes occur that underlie the therapeutic effect of electrophoresis:
- Proteolysis of biological tissue residues located in the canal system. (Professor A. Knappvost speaks of sterile oligopeptides and saponification mycelia, which, after leaving the canal system, are resorbed by the body).
- Killing remaining microorganisms by removing sulfur from amino acids. Fig. 3 At the apexes of the roots, copper “plugs” are clearly visible, tightly obliterating all exits of the apical delta to the cement surface
- Lining the unfilled part of the root canal, as well as all microcanals, with copper-calcium hydroxide, which ensures long-term sterility and also stimulates the formation of bone tissue in the area of microholes (Fig. 3).
- Stimulation of osteoblast activity in the periapical region as a result of alkalization.
Clinical practice
This method is suitable for the treatment of all gangrenous teeth. Especially for difficult-to-reach, partially obliterated and/or severely curved canals, the depophoresis method is the preferred and sometimes the only feasible alternative to traditional methods. After trephination of the tooth, the pulp chamber is opened in the usual way and the orifices of the canals are exposed. The canal is prepared over up to 2/3 of the length, and a width of ISO 35-50 is quite sufficient. It is advisable to expand the channel in the third closest to the mouth a little more in order to create a sufficient depot of the copper-calcium hydroxide suspension. We use the “Original II” device (Fig. 4). A negative needle electrode is inserted into the canal to a depth of 4-8 mm. (The electrode is not secured with any sticky wax.) The positive electrode is placed behind the cheek on the opposite side so that it does not touch the dentition. To reliably ensure the distance and for better conductivity, place a damp cotton swab between the electrode and the cheek. It is recommended to lubricate the corner of the patient's mouth with Vaseline. (The procedure is not performed in a physiotherapy room, but in the doctor’s chair).
Fig.4 Appearance of the “Original-11” device
Turn on the device and slowly increase the current until the patient signals, for example with his hand, that a feeling of warmth or tingling appears in the root area. (This is agreed upon with the patient in advance).
The current is reduced and increased again even more slowly, usually reaching 1 to 2 milliamps (mA). The session lasts 2-5 minutes. The required amount of electricity received by the patient is 5 mA X min.
Using the described method, you should influence each channel separately. During the procedure, bubbles are released from copper-calcium hydroxide into the cavity, which, especially if the tooth is covered with a crown, must be removed from time to time with a swab to avoid the discharge of electric current. Care should be taken that during depophoresis the needle electrode does not come into contact with the metal edge of the crown or filling. This will relieve the patient from unpleasant effects.
Finally, the channels and cavity are washed with distilled water or a 10% suspension of simple calcium hydroxide, but a diluted suspension of copper-calcium hydroxide itself can also be used).
As a tab until the next session, which is usually carried out after 8-10 days, after drying the canal, a fresh portion of copper-calcium hydroxide paste is injected. In most cases, three treatment sessions are sufficient to ensure treatment success. The patient must receive a total amount of electricity per channel (that is, the product of mA X minutes) equal to 15. After the last procedure, the entrance to the channel is filled with atatasamite, a special cement included in the kit (alkaline, copper-containing material). The rest of the canal (up to 1/3 of the apical part) is not filled with anything at all.!!)
Steps demonstrating gradual sterilization of canals
PSHa time between treatment sessions, according to the recommendations of prof. A. Knappvost, the cavity can be left open to prevent the development of pressure during the outflow of the still formed exudate. Recontamination is practically excluded due to the powerful disinfectant activity of medicalcium hydroxide.
Dr.S.Rocholl (Germany) says: “This method personally seemed unreliable to me at first. However, gradually I became convinced that it was completely justified. Currently, in my practice, I almost always use the depophoresis method. Only in rare absolutely “clear” cases after vital extirpation of single-rooted teeth with straight canals and in the absence of apical changes do I use traditional methods.”
Main differences between depophoresis and traditional methods
| Actions | Depophoresis | Mechanical-instrumental method |
| Channel search | No difference | No difference |
| Channel preparation | The apical third is not affected | Expansion throughout the depth of the canal up to the physiological opening |
| Canal sterilization | Complete sterility of the entire apical delta | Reducing the number of microbes in the main channel. The apical delta is unreachable. |
| Canal filling | Only the mouth of the canal | Filling for Pulpitis up to 1-1.5 mm to the apex, for periodontitis - completely |
| Subsequent audit | Hassle-free | Problematic |
| Risk of complications | Insignificantly small | Quite big |
| Treatment success | About 96% | 40-60% |
Indications for treatment using depophoresis
General indications
- functional ability of the tooth in perspective
- possibility of crown reconstruction
- sufficient tooth stability despite periradicular tissue changes (granulomas, cysts)
- satisfactory general condition of the patient (as for other types of endodontic treatment)
Specific indications
- canals with gangrenous contents 4 severely deformed root
- obliterated canals
- after unsuccessful treatment or in the presence of a crown, if most of the root filling can be removed
- channels with wide opening
- after the so-called vital extirpation
Advantages of depophoresis compared to other endodontic methods
- reliably proven treatment success in 96% of cases
- much less loss of tooth substance and therefore preservation of mechanical stability of the root
- much lower risk of perforation
- no need for channel measurement
- minimal risk of the healing or filling substance leaving the root apex
- reliable sterilization of the entire apical delta
- no need for root apex resection
- increase in indications for successfully predicted endodontic treatment - severely curved roots, obliterated canals, wide main opening
- treatment of canals that are not accessible to an instrumental approach
- low probability of hematogenous reinfection
- Osseoid closure of the hole leads to complete physiological cure
- exceptional efficiency (saving time, money, effort of the doctor and patient)
Clinical case 1
Chronic periodontitis 5 bottom left. Depophoresis sessions with copper-calcium hydroxide were performed. Additional filling with gutta-percha/silapex not up to the apex
After 6 months, significant reduction of the lesion
Clinical case 2
Chronic periodontitis 7 bottom left
Image 12 months after 3 sessions of depophoresis and incomplete filling with atacamite - gutta-percha