Removal or extraction of a diseased tooth is a surgical procedure, after which it is necessary to carefully monitor the condition of the gums at the site of intervention. After the procedure has been carried out, it is necessary to place a special turunda into the resulting cavity. To carry out this rather complex procedure, the surgeon’s professionalism alone is not enough, because the postoperative period is quite dangerous if proper care of the affected gum is not carried out at this time. In this case, if the treatment is insufficient, some kind of infection may get into the hole and cause complications.
To avoid any problems with healing, the doctor puts a special medicine in the socket of the extracted tooth. With its help, the wound is protected from infections and external influences. What medicine is put into the hole after tooth extraction? Let's talk about this in the article.
How is the affected tooth removed?
The procedure itself should only be performed by an experienced surgeon and only when other treatment methods can no longer help. There are a number of reasons that can trigger the removal of an affected tooth:
- if the crown of the tooth is completely destroyed;
- when the patient is indicated for prosthetics;
- if complications arise during the eruption of a wisdom tooth;
- if filling requires perforation of the root canal.
Important ! There are cases when there is every reason to remove a tooth, but the patient has contraindications to this. In such cases, most often the intervention is carried out within the walls of a hospital with subsequent monitoring of the patient’s condition.
There are a number of main contraindications to surgical tooth extraction. These include:
- previous heart attacks;
- high blood pressure;
- arrhythmia;
- blood diseases;
- mental problems or neurological diseases.
If no contraindications have been identified in a patient who needs surgical removal of the affected tooth, then he is referred to the procedure itself, which should be carried out according to the following scheme.
| Stage | Description |
| Visit doctor | Before performing the procedure, the doctor must find out whether the patient has allergic reactions to any anesthetics, cardiovascular pathologies, or whether the patient suffers from hypertension. |
| Anesthesia | After all the necessary information has been obtained, the patient is sent for anesthesia. A fairly large number of different means are currently used to remove teeth. Their duration of action is from forty minutes to three hours. |
| Preparation | Next comes preparation for the intervention itself: in order not to injure the gum during manipulation, it first peels off from the tooth bone by at least five millimeters. This procedure is carried out using a special tool. The surgeon places special forceps on the tooth, and then begins to swing the tooth itself with them in order to destroy the ligaments attached to the jaw bone. |
| Removal | The affected tooth itself is pulled out, that is, extraction. After the affected tooth has been removed, the resulting hole must be thoroughly examined. This is necessary so as not to leave tooth fragments or a cyst in the wound cavity. If the extraction of the affected tooth took place in the presence of flux, then after its removal the gums are cut in the right place and the pus is released. After this manipulation, a drainage is inserted into the wound cavity. |
| Treatment | After the procedure is completed, you need to treat the wound itself. If pus is found at the site of the lesion, then in this case the hole must be washed with an antiseptic solution, and then an anti-inflammatory agent should be placed in the wound. If the hole itself is too large after extracting the tooth, then a suture is necessary. |
| Consultation | After the procedure has been completely completed, before discharge, the doctor must instruct the patient in detail on how to care for the hole during the healing period, and also prescribe any medications if necessary. |
After the tooth is removed and before the patient goes home, the doctor inserts a special medicine into the tooth socket. It is necessary to protect the wound from various influences, as well as for faster and more proper healing. Some patients complain that the turunda with the medicine interferes greatly, but this will have to be endured.
Important ! If you remove the turunda ahead of time, serious complications may develop, which will have to be dealt with not only by the dentist, but also by other doctors.
The doctor prescribes exactly the medicine that is safe for every person. True, it does not have the most pleasant taste, but a person will have to ignore this factor if he wants the wound to heal as quickly as possible.
There are exceptional cases when it is simply impossible to remove the affected tooth according to the scheme above. The reason for this may be the following factors:
- if the tooth root is crooked;
- if the bone tissue of the tooth is too fragile;
- if the crown of the affected tooth is already completely destroyed;
- if the figure eight is in a position of incomplete eruption or in a horizontal position.
If a patient who needs tooth extraction has any of these characteristics, then the intervention is performed in a different way. First, the gum is cut and peeled away from the bone. After this, the specialist drills out the desired area using a drill, which creates access to the root of the required tooth.
Important ! In some cases, the partitions between the roots of the tooth are sawed, after which each root is removed one by one.
After such procedures, healing is more difficult and longer. Such an intervention may cause the patient to develop stomatitis. In many cases of such intervention, a secondary infection is attached to the affected area.
However, no matter which tooth is removed, medicine must be placed in the hole. This procedure is required.
Tooth extraction
Modern surgical dentistry allows, in most cases, to avoid tooth extraction. But, if a diseased tooth poses a threat to healthy ones, then the procedure is inevitable. The operation is performed under local anesthesia and takes up to 40 minutes. The dentist extracts the tooth along with its roots using forceps. If indicated, the doctor can use a dental bur to divide the tooth into parts and remove them separately.
When is tooth extraction necessary?
Indications for tooth extraction:
- A frequent indication for surgery is the need for sanitation of the oral cavity in the presence of chronic periodontitis in the acute stage, when it is impossible to eliminate the inflammatory focus at the apex of the tooth
- Removal is also carried out in order to avoid more serious complications. For example, in the presence of teeth that can cause a cyst, inflammation or neuritis of the trigeminal nerve
- If a tooth constantly injures the tongue or the mucous membrane of the cheek, interferes with a normal bite, if orthodontic treatment is impossible
- For extensive caries, when therapeutic or orthopedic restoration is impossible
- Teeth that are incorrectly positioned or have not fully erupted must also be removed.
How to prepare for tooth extraction? Is it painful?
Before the operation, the dental surgeon prescribes an X-ray examination (3D dental computed tomography) to the patient, studies the condition of diseased teeth, adjacent healthy teeth, and the location of their roots. Before removal, the patient is given an anesthetic by injection. Before the injection, an anesthetic gel is applied to the gums, so discomfort is minimized.
What to do after tooth extraction?
After the operation itself, no specific actions are required from the patient. It is advisable not to eat for 3 hours, not to touch the hole with your tongue and not to rinse your mouth.
To prevent subsequent displacement of adjacent teeth, it is advisable to install a denture. Even one missing tooth causes a redistribution of the chewing load and can lead to bone atrophy and displacement of adjacent teeth. Installing a dental implant helps avoid these changes. Sometimes an implant can be installed immediately after removal—simultaneous implantation. If the tooth extraction was associated with inflammation, then you should wait for the wound to heal and then install implants. In each specific case, the dentist will suggest the best methods of further treatment.
What should the patient do after the procedure?
After the procedure has been completed, the specialist must carefully explain to the patient his next steps, as well as the rules for caring for the wound during the healing period.
- The turunda or cotton wool that was left by the surgeon in the hole does not need to be removed by yourself. If the tampon placed by the doctor falls out ahead of schedule, the patient must return to the specialist to install a new turunda. If this is not done, an infection may enter the wound cavity.
- If after the procedure the cheek is very swollen, you can apply ice or a cold compress to it. After this procedure, it is forbidden to heat the affected area and apply hot compresses.
- You can eat food after tooth extraction only two hours after the procedure. It is recommended to eat only liquid and light foods that do not contain solid pieces.
- A blood clot forms in the hole where the tooth was pulled out. It is prohibited to remove it or touch it. The first time after the procedure, you must brush your teeth with caution and do not use any rinses.
- For 7 days after tooth extraction, it is prohibited to carry out other interventions in the oral cavity.
- During the healing period, it is not recommended to overheat, for example, take a steam bath, and also exercise with caution. It is also strongly recommended to stop drinking alcoholic beverages and smoking cigarettes for two days after the procedure.
- After tooth extraction, pain often occurs at the extraction site. In this case, quite often not only the hole, but the whole head as a whole can hurt. Also, the patient may experience pain while eating, regardless of which side of the teeth he chews on. Experts recommend coping with these problems with the help of painkillers, such as Pentalgin or Tempalgin. In this case, it is advisable to take the drug in combination with Suprastin.
Despite the fact that there is medicine in the hole, a person may still feel pain and some burning. Such unpleasant sensations will have to be ignored.
Important ! If the sensations intensify, it is recommended to consult a doctor again so that he can examine the wound and, if necessary, take action.
Turunda for endodontic therapy of pulpitis and periodontitis
Use: in medicine, namely in therapeutic dentistry. The essence of the invention: turunda is a base on which the composition of the composition is cured at 75-80oC, wt.%: carboxyl cation exchanger 9.4 - 13.8; polyvinyl alcohol 3.0 - 4.6; glycerin 6.1 - 9.2 and water 72.4 - 81.0. 1 table
The invention relates to medicine, namely to therapeutic dentistry, and can be used as a means for endodontic therapy of pulpitis and periodontitis by one-time temporary filling of the root canals of teeth in a clinical setting.
As a means for endodontic therapy of pulpitis and periodontitis in clinical settings, various drugs are used, injected into the root canals on cotton or paper turundas. Such drugs must have a full anti-inflammatory, antimicrobial, hyposensitizing, detoxification, analgesic, plastic-regenerative effect on periodontium. It is known for the endodontic treatment of pulpitis and periodontitis to use cotton turundas soaked in antimicrobial drugs (0.02% solution of furatsilin, 1% solution of iodinol, 2% alcohol tincture of iodine, 40% solution of hexamine, clove oil).The disadvantage of using cotton wool with medications is their low effectiveness (treatment period is 3-4 days) due to inactivation of the drugs in the root canal. In addition, some medications have an allergenic effect and contamination of cotton swabs during manufacturing cannot be ruled out. The closest in technical essence to the invention is the use of cotton swabs with sorbent for endodontic therapy of pulpitis and periodontitis, where activated carbon SKNP-2 is proposed as a sorbent, which is applied on a cotton swab after pre-treatment of the root canal. The disadvantage of using SKNP-2 charcoal applied to a cotton swab is the low effectiveness of treatment, since the sorbent is applied to the mouth of the root canal, and is not applied directly to the source of inflammation. Lack of contact with the source of inflammation reduces the therapeutic effect, since active sorption of intoxication products is excluded (cessation of pain in the patient within 3-6 hours, treatment period 1-2 days). The technical objective of the invention is to increase the therapeutic effect of turunda and reduce the treatment time for pulpitis and periodontitis. This is achieved by the fact that in the known turunda for endodontic therapy of pulpitis and periodontitis, containing a sorption component, the latter is used as a cation exchanger based on a copolymer of methyl acrylate and diethylene glycol divinyl ether in salt form and additionally polyvinyl alcohol, glycerin and water in the following ratio in initial mixture, wt. Carboxyl cation exchanger 9.4 13.8 Polyvinyl alcohol 3.0 4.6 Glycerin 6.1 9.2 Water 72.4 81.0 Carboxyl cation exchanger based on a copolymer of methyl acrylate and diethylene glycol divinyl ether, produced under the trademark KB-2E in the form granules with a grain size of 0.315 1.6 mm according to STP 6-07-437-92 and is intended for the manufacture of ophthalmic ion-exchange inserts. Carboxyl cation exchanger KB-2E is used in salt form, for example in Na or Ca form or their mixture in crushed form with particle size 0.1 to 100 microns (pulverized fraction). The indicated quantities of each of the components are optimal, and going beyond the given limit values reduces the therapeutic effect and increases the treatment period for pulpitis and periodontitis. When making turundas, a composition is obtained by mixing the initial components to a homogeneous mass, one at a time from the recipes given in the table (examples 1-3). The polymer composition is applied to a nylon or propylene base, passed through a die, producing bundles 1-2 mm thick, which are dried at room temperature, then cut into lengths of 17-23 mm and they are cured at 75-80oC. Ready-made turundas are assembled in an amount of 15 pieces, sterilized and used once. In the treatment of pulpitis and periodontitis, after the necessary endodontic treatment, medicinal treatment of the root canals is carried out with a 3% solution of hydrogen peroxide and a 1% solution iodinol, then the channels are dried and filled with the proposed turunda. A dry sterile cotton ball and an artificial dentin bandage with distilled water are applied to the mouth of the canals. The turunda is left in place for 24 hours, after which it is removed and the root canals are filled with an intradont. Below are examples of the treatment of pulpitis and periodontitis with turundas containing the sorption component carboxyl cation exchanger KB-2E, made from polymer compositions, according to examples 1 to 3 given in the table. The patient D. (30 years old) presented with acute arsenic periodontitis. Treatment was carried out with a turunda made from a polymer composition according to example 1. An hour after applying the turunda, pain relief was noted, and a day later painless percussion and unchanged mucosa were observed, which made it possible to complete treatment the next day. Patient K. (42 years old), who applied with chronic gangrenous pulpitis, root canals were treated with turundas containing a polymer composition according to example 2. During the first 10 minutes, the feeling of discomfort in the root canal disappeared; upon objective examination, percussion was painless; the next day after removal of the bandage and turunda, tooth treatment was completed. In patient S. (27 years old), who presented with acute apical periodontal disease (post-traumatic), 30 minutes after the application of turundas made from a polymer composition according to example 3, the pain subsided, and after 14 hours the root canals were sealed. When observing the treatment of 36 patients (16 cases pulpitis and 20 cases of periodontitis) pain relief was noted in case of pulpitis after 5-10 minutes, in case of periodontitis 30-40 minutes after applying turundas containing carboxyl cation exchange resin KB-2E, and in no case were there any symptoms of allergization. The proposed turundas are simple and convenient in use and storage and have anti-inflammatory, analgesic, anti-exudative, detoxification and hemostatic effects.
Claim
A product for endodontic therapy of pulpitis and peridontitis, consisting of a base and a sorbent, characterized in that the sorbent is a composition cured on the base at 75-80oC with the following composition, wt. Carboxylic cation exchanger 9.4 13.8 Polyvinyl alcohol 3.0 4.6 Glycerin 6.1 9.2 Water 72.4 81.0o
DRAWINGS
About the medicine
The medicine that is placed in the hole can be applied to a piece of gauze, which is subsequently inserted into the hole. In this case, after a certain amount of time indicated by the doctor, it needs to be taken out. This can be done either independently or during your next visit to the dentist. If this is not done in time, the process of putrefaction may begin, which will greatly complicate the situation. It is also not recommended to take out the gauze ahead of time, since food particles can get into the hole and the tongue can touch it, which will interrupt the healing process and also cause complications.
There is another way to install the medicine - in a hemostatic sponge. It already contains a medicine that helps disinfect the socket cavity and helps stop bleeding. You cannot take this sponge out - it will dissolve on its own. Most often this happens within 1-2 days, but in some cases the sponge may remain in the hole for 5-6 days. There is no need to be afraid of this. As a last resort, you can consult a doctor who will examine the wound and determine whether healing is proceeding normally.
Often the medicine in the sponge is very bitter, and this causes severe discomfort to the person. Unfortunately, nothing can be done about this, since getting rid of the sponge ahead of time is strictly contraindicated. To eliminate bitterness, you can drink sweet tea or juice.
Remember ! No circumstances can influence the ability to remove the medicine from the hole ahead of time. After 3-4 days, the surface of the hole will heal, and you will no longer have to experience discomfort.
People often wonder what kind of medicine is used for these purposes. Sometimes the gauze that is placed in the hole is treated with iodine - this will both disinfect the wound and prevent bleeding. The hemostatic sponge is already treated with a special substance consisting of boric acid, collagen and nitrofural, which helps stop the bleeding and protect the hole from various influences. But most often dentists use Alvozhil.
No other means are used for inserting into the hole.
How long does it take for a hole to heal?
The wound left after tooth extraction has a certain healing pattern.
- After the tooth extraction procedure is completed, the circular ligament located around the crown of the extracted tooth begins to contract.
- A short amount of time after the procedure, you may notice an accumulation of blood in the hole. The resulting clot helps protect the wound from infection or small food particles. Over time, the hole begins to become overgrown with fibrous tissue.
- After a certain amount of time, which depends on the characteristics of the human body, as well as on the correct care of the hole after the procedure, the surface of the wound heals and the affected area of the gum is restored.
- After this, over time, new epithelium grows on the surface of the gum, as well as the development of bone tissue at the site of tooth extraction.
Important ! The normal healing of the hole is facilitated by the medicine that is placed in the hole. Without it, the wound will not heal.
Many patients worry about the healing of the wound that remains after tooth extraction. The doctor must explain to the patient that the wound can heal completely only after two or three weeks, provided that all care rules are followed. If they were nevertheless broken or an infection was still able to penetrate the wound, then with repeated disinfection, complete restoration of the affected area will occur in five months.
What is allowed during the healing period?
- Non-solid semi-liquid food.
- Gentle oral hygiene.
What is prohibited during the healing period?
- Drinking alcohol and smoking cigarettes.
- Drinking liquids with a plastic straw.
- Harsh brushing of teeth in general and especially in the healing area.
- Eating dry and solid food.
- Sudden movements of the cheekbones for one week after the procedure.
Dressings used in dentistry
Gum dressings are composed of:
- soft - ointments, gels (actovegin, solcoseryl) - applied in a thin layer to the wound surface. This category includes bandages made of cotton wool, gauze, bandages;
- semi-solid - are made by applying a mixture of dentin paste and ointment to the prepared tissue surface. The bandage is applied to the wound and fixed by compressing the teeth. After 6 - 7 minutes it hardens and is securely attached to the desired area;
- solid - septopack (ready-made product) or independently prepared using dentol, repin. The components have a high degree of biological compatibility with the mucous membrane, their use significantly accelerates the wound healing process;
- collagen films - have anesthetic and antiseptic properties, promote rapid regeneration of soft tissues of the oral cavity;
- adhesive - are non-toxic compositions based on polyurethane. Once on the mucous membrane, the material polymerizes, creating a plastic, porous film.
Auxiliary medications for tooth extraction
If, after the tooth is removed, any complications begin at the intervention site, then modern pharmaceuticals can cope with them. With the help of various medications, the patient can not only eliminate the resulting secondary complications, but also strengthen his immunity as a whole. Quite often, specialists, to ensure against possible complications, in particular, various inflammations and suppurations, prescribe antibacterial drugs in the postoperative period. At the same time, the patient also needs to strengthen the immune system, which will help the wound heal faster. To do this, doctors prescribe vitamin complexes to the patient. Thus, in addition to the medicine placed in the hole and affecting its healing, the patient is recommended to take other drugs to speed up the process.
If during the procedure the patient was identified with any peculiarities or complications and tooth extraction was not without additional trauma, then a number of medications are prescribed in the postoperative period, since in this case there are additional risks of complications. The main thing is that the patient treats the postoperative period responsibly and does not neglect the doctor’s advice and the medications prescribed to him.
Important ! According to statistics, every third patient who has had a tooth removed needs to take antibiotics.
Taking antibiotics after the procedure
Dentists quite often resort to antibiotics in the postoperative period, especially after tooth extraction. But not every patient who has undergone tooth extraction requires antibiotics. They are prescribed only in the following cases:
- if the patient experiences inflammatory processes in the gum area;
- if the patient is elderly;
- if complications arise during the operation or features of the anatomy of the teeth are revealed, which contributes to more extensive trauma;
- if the patient has a reduced immune system or suffers from any blood diseases.
This list is not all of the reasons for prescribing antibiotics in the postoperative period, because each individual case has its own characteristics. An experienced dentist will be able to easily determine which patient needs to take medications after tooth extraction. The doctor must determine the duration of administration and dose individually for each case. Most often, the course of taking the drug after tooth extraction lasts from five to seven days. In rare complicated cases, treatment can last up to fifteen days. It is simply impossible to determine the average dose of antibiotics that is needed, since each individual drug has its own individual characteristics.
Important ! It is strongly recommended not to take antibiotics unless prescribed by a doctor.
In addition to antibiotics, your doctor may also prescribe medications to normalize the microflora after taking antibiotics. The most commonly prescribed drug is Linex, but sometimes other drugs from the group of probiotics are also prescribed.
What painkillers can be taken in the postoperative period?
Most often, when local anesthesia wears off after a tooth extraction procedure, the patient feels pain in the area of intervention. The best way to eliminate pain is to take NSAIDs. This group of drugs is the most effective in eliminating toothache.
- The drugs "Nurofen" or "Ibuprofen" cope well with pain after surgery. It is necessary to take the drug 500-800 mg three to four times a day, depending on the intensity of the pain.
- "Ketorol" is one of the most effective and powerful drugs from the NSAID group, which can eliminate pain after the procedure in a fairly short time. It is also used two tablets three to four times throughout the day.
Types of dressing material in dentistry
The following are widely used in dentistry:
- Absorbent cotton wool is used in therapeutic dentistry to dry the patient’s oral cavity during treatment. Cotton rolls are formed by twisting the material onto the handle of any dental instrument.
- White gauze is used to make napkins, balls, and strips for tamponade. The main condition is that the edges of the gauze are folded into the middle - this prevents fibers from getting into the wound. Used as a drying material for wounds.
The dressing material must be sterilized before use.
Basic rules of oral hygiene after tooth extraction
In order to prevent possible complications after the procedure, you need to strictly follow the rules of oral hygiene.
- Two to three days after tooth extraction, the mouth can be rinsed with a soda solution. It is diluted in the ratio of one teaspoon of soda to one glass of warm water. You can also rinse with other means that help faster healing, for example, Chlorhexidine. Rinsing should be done very carefully, as it can damage the integrity of the blood clot that has formed in the hole. Gentle rinsing is carried out by drawing a solution into the oral cavity. After this, you just need to hold the solution in your mouth for a while and then spit it out. This rinse will not harm the blood clot.
- Rinsing is necessary to prevent infection or food particles from entering the wound, which can cause suppuration.
There are a number of symptoms that indicate the presence of complications in the postoperative period. Among them:
- pain that does not subside for several days after the procedure. In the presence of such pain, even various painkillers cannot help;
- the patient notes continuous bleeding from the wound. In this case, the blood has a bright scarlet hue;
- The patient’s body temperature rises and remains for 24 hours after the tooth extraction procedure;
- slight swelling of the cheek after the procedure develops into severe swelling that spreads over the entire side of the face. The patient feels weak and drowsy;
- pus is leaking from the wound or the area around the wound has begun to darken. In this case, after a few days the patient experiences a persistent putrid odor from the mouth;
- the dentition may become mobile;
- divergence of applied sutures.
Important ! If the patient notices any of the listed symptoms, in this case it is necessary to urgently consult a doctor. If such complications are left unattended, they will soon develop into more serious pathologies that can threaten not only the patient’s health, but also his life.
After tooth extraction, pain appeared.
Due to the fact that I provide acute pain dentistry, I am often approached with complications after tooth extraction, pain after wisdom tooth removal, unsuccessful implantation and complications after root canal treatment, from other doctors and clinics.
The cause of pain after tooth extraction may be developed alveolitis of the tooth socket, rough and traumatic tooth extraction, or sharp bone edges of the tooth socket after extraction.
Alveolitis.
Alveolitis is a disease that, according to various authors, accounts for 24-35% of the number of cases of all complications occurring in patients after tooth extraction.
Quite often, alveolitis develops as a result of a traumatic tooth extraction operation, especially if the patient does not comply with the rules of oral hygiene.
Alveolitis is more often observed during a prolonged operation to remove a tooth or root, as well as with significant injury to the bone and mucous membrane, which subsequently become infected.
If, after removal of the tooth root, the edges of the socket remain sharp and exposed, then this contributes to the appearance of post-traumatic neuritis in the postoperative period and the development of alveolitis against its background.
For normal healing of a post-extraction wound, it is necessary to have a blood clot in the socket. To prevent the formation of dry sockets, you need to eliminate the causes that may prevent the formation of a blood clot.
The cause of the development of alveolitis may be excessive tissue infiltration with an anesthetic substance, which contributes to the formation of a large number of “dry sockets”.
The use of vasoconstrictor drugs administered together with local anesthetics leads to prolonged vasospasm and prevents the formation of a blood clot in the tooth socket.
Violation of the blood clotting process, tamponade of the hole with gauze strips, non-compliance by the patient with the doctor’s recommendations (rinsing the mouth after surgery, smoking, drinking alcohol) can also cause a violation of the formation of a blood clot. The destruction of a blood clot can occur due to the fibrinolytic effect of saliva.
The occurrence of a “dry socket”, and therefore alveolitis, can be facilitated by traumatic tooth extraction, improper detachment of the dentogingival ligament, and the wrong choice of instrument for the operation.
Microorganisms can penetrate into the post-extraction wound from odontogenic and non-odontogenic foci of chronic infection, which are located in the form of granuloma or granulation tissue on the mucous membrane of the oral cavity, nose, nasopharynx, as well as in the hole itself.
The main place of accumulation of staphylococci in the human body is the nasal cavity. Its high contamination with staphylococci is a stable indicator of the development of alveolitis, independent of the age and gender of patients.
With alveolitis, patients complain of constant aching pain that intensifies while eating. The socket of the extracted tooth usually gapes, the mucous membrane is hyperemic, swollen and painful. In some cases, the tooth socket may be filled with the remains of a blood clot, on the surface of which there are food debris. In the anamnesis - a tooth was removed, it hurts a lot, the removal took place 2 days ago.
In other cases, the hole may contain a disintegrated blood clot, food debris, or saliva. The patient's body temperature, as a rule, does not increase. Regional lymph nodes do not become inflamed.
Alveolitis develops on the 2nd or 3rd day after tooth extraction and lasts about 1 week. Patients usually report: “They removed a tooth and the hole hurts a lot after tooth extraction.”
With purulent-necrotic alveolitis, patients develop intense constant pain radiating along the branches of the trigeminal nerve, putrid breath, weakness, and malaise. Body temperature rises to 37.5-38.0° C. Asymmetry of the face resulting from swelling of the soft tissues on the side of the extracted tooth. Regional lymph nodes are enlarged and painful on palpation.
Opening the mouth causes pain. The mucous membrane around the tooth socket is hyperemic, swollen, painful, the alveolar process is thickened. The postoperative wound is filled with necrotic masses and covered with a dirty gray coating with a pungent, unpleasant odor. This form of inflammation of the socket develops, as a rule, 3-4 days after tooth extraction. A purulent-necrotic process occurs.
In patients with diabetes mellitus, alveolitis occurs with a more pronounced local inflammatory reaction and is characterized by “inhibition” of reparative processes in the area of complicated wounds.
Treatment of alveolitis.
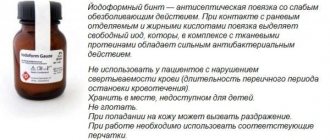
The hole is loosely filled with iodoform turunda, followed by its regular replacement with a similar turunda.
All manipulations in the treatment of alveolitis, sometimes, need to be carried out under local conduction anesthesia, since the latter, in addition to the analgesic effect, has a beneficial effect on the course of the inflammatory process.
The tooth socket should be washed with warm antiseptic solutions. Rinsing must be done under pressure using a syringe, bringing the curved needle to the bottom of the tooth socket and making sure that there are no remnants of a disintegrated blood clot, bone fragments or dental fragments left in it. Then the tooth socket is filled with iodoform turunda.
The first change of turunda is made after 1 day, and then after 3-4 days until the pain disappears and recovery.
Sharp bone edges of the socket.
Pain in the area of the postoperative wound can be caused by sharp protruding bone edges of the socket, which injure the mucous membrane located above them.
Most often, sharp bone edges in the area of a postoperative wound are formed after the removal of several adjacent teeth or during their atypical removal.
Patients complain of severe pain of a neuralgic nature, which most often appears 3-5 days after tooth extraction, when the approaching gingival edges seem to be pulled onto sharp areas of the alveolar bone. The pain intensifies while eating or when accidentally touching the tooth socket with your tongue.
When examining the area of the postoperative wound, a protruding, uneven edge of the alveoli is visible. There are no signs of inflammation, which distinguishes this complication from alveolitis. When palpating the protruding sharp bone edges, the patient feels a sharp pain, which decreases somewhat as the bone atrophies.
However, bone resorption occurs over a long period of time, so the pain does not disappear for a long time and patients should undergo an alveolectomy operation - removal of the protruding sharp bone edges of the alveoli.
Surgery is performed under local anesthesia. An incision is made over the protruding bone edge, and the mucoperiosteal flap is removed. Sharp bone edges are removed. The flap is placed in place and sutures are applied.
Prevention of the development of this complication is the removal of the protruding edges of the alveoli directly during the tooth extraction operation.
If you need advice about alveolitis after tooth extraction or you have pain after wisdom tooth removal, sign up for a free consultation by phone:
And.
Kharkov, st. Sumskaya, 71. Information on the topic: Dental surgeon Anesthesia in dentistry Tooth extraction Removal of a wisdom tooth Removal of a wisdom tooth on the upper jaw Removal of a wisdom tooth under anesthesia Complex tooth extraction Resection of the apex of the tooth root Periostitis treatment Complications after tooth extraction Dental implantation Surgeon implantologist
Prevention
There are a number of actions that the patient must take immediately after this procedure and which will allow him to prevent possible complications.
- After the extraction, the patient needs to tightly compress the dentition. This is necessary in order to press firmly on the tampon placed in the wound.
- The medicine should not be removed by yourself.
- The hole should not be touched with your tongue or fingers. This is necessary so as not to accidentally damage the blood clot that has formed in the wound.
- If the patient experiences unbearable pain, it can be relieved with the help of analgesics that were recommended by a specialist. The dosage should also be prescribed by the doctor, since each patient reacts individually to the tooth extraction procedure.
- During the period until the wound is completely healed, the patient should stop smoking. This process greatly interferes with the normal healing of the hole.
- If the patient detects symptoms of complications, then, without delay, he should consult a dentist.
The patient needs to be aware of symptoms that may indicate the occurrence of suppuration or any other complications. Having noticed any of the signs, the patient should immediately contact a specialist for advice and subsequent treatment. We must not forget that only proper maintenance of oral hygiene and compliance with all the necessary rules will help the wound heal much faster. You will find out the proportions of soda solution for rinsing teeth in the article.