7 January 2020
47930
2
4 out of 5
A sequestered hernia is a severe complication of osteochondrosis, which is the last stage of development of an intervertebral hernia in any part of the spine. This term means the separation of part of the nucleus pulposus of the disc into the spinal canal, which closely borders the most sensitive anatomical structure to any influence - the spinal cord. There are also numerous nerve roots, the compression of which can lead to paresis or paralysis.
Disc anatomy
Sequestered hernias are diagnosed in 10% of patients with a previously diagnosed protrusion or intervertebral hernia.
Ostiomyelitis - general information
Osteomyelitis
(from the Latin osteon bone + myelos bone marrow + itis inflammation)
is
an inflammation of the bone marrow, which usually affects all elements of the bone (periosteum, spongy and compact substance). According to statistics, osteomyelitis after injuries and operations accounts for 6.5% of all diseases of the musculoskeletal system. Most often it affects the femur and humerus, lower leg bones, vertebrae, mandibular joints and upper jaw. After open fractures of the diaphysis of long bones, post-traumatic osteomyelitis occurs in 16.3% of cases. Men suffer from osteomyelitis more often than women, children and the elderly - more often than young and middle-aged people.
ICD-10
M86
Osteomyelitis
Classification
There are nonspecific and specific osteomyelitis. Nonspecific osteomyelitis is caused by pyogenic bacteria: Staphylococcus aureus (90% of cases), streptococcus, Escherichia coli, and less commonly, fungi. Specific osteomyelitis occurs with tuberculosis of bones and joints, brucellosis, syphilis, etc.
Depending on the path by which microbes penetrate the bone, endogenous (hematogenous) and exogenous osteomyelitis are distinguished. In hematogenous osteomyelitis, pathogens of purulent infection are introduced through the blood from a remote focus (furuncle, felon, abscess, phlegmon, infected wound or abrasion, tonsillitis, sinusitis, carious teeth, etc.). With exogenous osteomyelitis, the infection penetrates the bone during injury, surgery, or spreads from surrounding organs and soft tissues.
In the initial stages, exogenous and endogenous osteomyelitis differ not only in origin, but also in manifestations. Then the differences are smoothed out and both forms of the disease proceed in the same way. The following forms of exogenous osteomyelitis are distinguished:
- post-traumatic (after open fractures);
- gunshot (after gunshot fractures);
- postoperative (after wires or bone surgeries);
- contact (during the transition of inflammation from surrounding tissues).
As a rule, osteomyelitis is initially acute. In favorable cases it ends with recovery, in unfavorable cases it becomes chronic. In atypical forms of osteomyelitis (Brodie's abscess, Ollier's albuminous osteomyelitis, Garre's sclerosing osteomyelitis) and some infectious diseases (syphilis, tuberculosis, etc.) there is no acute phase of inflammation, the process is primarily chronic.
Acute osteomyelitis
Manifestations of acute osteomyelitis depend on the route of infection, the general condition of the body, the extent of traumatic damage to the bone and surrounding soft tissues. On radiographs, changes are visible 2-3 weeks after the onset of the disease.
Chronic osteomyelitis
With small foci of inflammation, complex and timely treatment, mainly in young patients, restoration of bone tissue prevails over its destruction. Foci of necrosis are completely replaced by newly formed bone, and recovery occurs. If this does not happen (in approximately 30% of cases), acute osteomyelitis becomes chronic.
By about 4 weeks, in all forms of acute osteomyelitis, sequestration occurs - the formation of a dead area of bone surrounded by altered bone tissue. At 2-3 months of the disease, the sequestra are finally separated, a cavity is formed at the site of bone destruction and the process becomes chronic.
Distinctive signs of osteomyelitis and periostitis
| Osteomyelitis | Periostitis |
| The infiltrate may cover half the jaw | The infiltrate is localized in the area of one “causal” tooth |
| Paresthesia along the nerve | No paresthesia |
| Pain when percussing adjacent intact teeth | There may be pain when percussing adjacent teeth, but it is not pronounced |
| 1-2 days after opening the abscess and removing the tooth, the purulence intensifies, the patient’s condition does not improve | On the 2nd day after the removal of the “causal” tooth, signs of inflammation quickly subside, the discharge of pus decreases or stops |
| The temperature is elevated even after opening the abscess | Temperature quickly returns to normal after surgery |
Treatment for acute odontogenic osteomyelitis of the jaw should be aimed at eliminating the purulent-inflammatory focus in the bone and soft tissues. Treatment steps include:
- mandatory removal of the “causal” tooth;
- opening of soft tissue infiltrates of the peri-maxillary region (in this case, the incisions can be both intra- and extraoral; they must be wide for good outflow of purulent exudate);
- insertion of rubber drainage into the wound;
- prescription of antibacterial therapy with antibiotics (long-term) with microflora monitoring every 5-7 days;
- combination of antibiotics with sulfonamide drugs, nitrofuran drugs, antihistamines;
- Plenty of fluids, vitamins and dairy-vegetable foods are recommended;
- prescription of physiotherapeutic procedures (UHF, microwave, UV irradiation).
Chronic stage of osteomyelitis of the jaws . In this case, antibacterial, anti-inflammatory treatment and sequestrectomy . With prolonged treatment of osteomyelitis, an exacerbation may occur with the formation of sequestration. A sequestrum is an area of dead bone tissue that occurs due to osteomyelitis at the site of infection in the bone. It is surrounded by sclerotic bone with fibrous tissue, which appears as denser areas of bone on x-ray. The formation of such a site can cause irritation of surrounding tissues and the formation of pus, which begins to be released through the fistula.
The sequestra of the upper jaw are removed 3-4 weeks after the onset of the disease, the lower - after 5-8 weeks. Sequestrectomy is performed from the oral cavity under reliable anesthesia. After the sequestrectomy operation, the cavity is filled with a hemostatic sponge with a dry antibiotic. The wound is sutured, leaving an outlet hole. If the surgeon is confident that necrotic tissue will be completely removed, bone grafts are inserted into the cavity. Otherwise, the cavity is loosely filled with a tampon with iodoform emulsion, which is changed as the cavity is filled with connective tissue every 4-5 days. Secondary sutures are placed on the wound. Teeth whose pulp has died are treated, if possible, or removed if it is impossible to save them. After surgical treatment, physiotherapy is prescribed (electrophoresis, UHF field, microwaves).
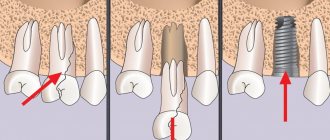
This is interesting: The inevitability of dental implant removal and the essence of the procedure
Request a consultation
Symptoms of the disease
A sequestered hernia will make itself felt with the following symptoms:
- pain syndrome that is constant in nature, intensifying with changes in body position;
- pain may radiate to the limbs or other parts of the body, depending on the location of the hernia;
- sensory disturbances due to pinched nerve fibers;
- autonomic disorders;
- reflex muscle contraction in the area of inflammation;
- aseptic inflammation, which can lead to osteomyelitis.
Manifestations of the disease largely depend on the location of the sequestered hernia.
The concept and essence of sequestrectomy
A surgical method aimed at removing fragments of jaw bone tissue affected by necrosis is called sequestrectomy, and these areas are called sequesters.
The anomaly is a consequence of osteomyelitis, a fairly common dental disease.
The surgical decision in this case is a necessary measure. Its goal is to restore the normal functioning of the dentofacial apparatus , return the patient to health and improve the quality of life.
The essence of the procedure is to free, by curettage, the affected fragments from a focal infection - osteomyelitis, concentrated deep inside the bone tissue.
If the sequestration is not cleared of purulent masses, over time they will simply melt the bone, which threatens the person with a jaw fracture.
Basic principles of sequestrectomy
- Sequestrectomy is always performed under local anesthesia, or even general anesthesia
- During the operation, it is necessary to create a wide, flat opening, which in subsequent stages will not interfere with the outflow of purulent contents
- It is necessary to remove exactly the amount of bone tissue that will allow you to completely get rid of the sequester without damaging it or leaving part in a healthy jaw
- Fistula tracts should be completely excised
- The restored bone tissue should be treated with the utmost care, since the recovery process after surgery will depend on it
- Bone grafting, that is, filling the cavities formed during the operation with a special substance, is carried out later, when the infection has been completely eliminated
Indications for sequestrectomy
The main indication for sequestrectomy is chronic osteomyelitis in the presence of the following in the oral cavity and jaw:
- Ulcers
- Sequesters
- Osteomyelitis cavities
- False joints
- Purulent fistulas
Sequestrectomy is also used if the disease often recurs, is accompanied by severe pain, intoxication, or even disruption of the jaw. In addition, sequestrectomy is simply necessary if the affected area has become malignant, or pathology of other systems and organs has occurred due to purulent chronic inflammation. All this is possible if you do not treat osteomyelitis for a long time.
Sequestrectomy - treatment of osteomyelitis
Contraindications to sequestrectomy
- Severe general condition of the patient due to any health problems;
- Chronic diseases that can worsen due to surgery or cause complications.
In any case, the decision about whether or not to perform a sequestrectomy is made by the attending physician.
Diagnostics and sequestrectomy in the clinic
Radiography is the most reliable diagnostic method. Before performing the operation, our specialists study radiographs taken in different projections.
The doctor will prescribe a fistulography before sequestrectomy. This is an X-ray study using a contrast agent, which allows you to accurately determine the extent and nature of fistulas, the size and shape of osteomyelitic cavities, that is, the specialist gets a complete picture of disorders in bone tissue and centers of destruction. Sometimes, along with bone destruction, new bone appears.
Most often, sequestrectomy is performed using local anesthetics. At the clinic, specialists use high-quality German anesthetics to ensure that the operation takes place without pain and stress.
- When performing a sequestrectomy, the doctor will create a wide opening through which pus can flow freely. Next, an experienced dental surgeon will remove the affected bone tissue, thereby completely ridding the jaw of sequestration. Healthy bone tissue will not be damaged. Fistula tracts are removed by excision. Filling of the cavities that arose during the operation with a special substance is carried out only after the source of infection has been completely eliminated.
- After applying anesthesia, the sequesters are carefully scraped out with a special instrument. Access to the affected areas in some cases is carried out from the oral cavity. The resulting cavity is filled with a biomaterial that activates bone formation. This substance contains antiseptic or antibacterial components. The wound is completely sutured by a specialist.
- If the upper jaw is affected, inflammation is often present in the maxillary sinus. Then, in fact, two simultaneous operations are indicated: sequestrectomy and sinus surgery. These are very difficult cases. If the lower jaw is affected, access to the affected area is made extraorally.
- After administering the anesthetic, the surgeon will cut the lower jaw in the right places, remove pathogenic bone elements, put a bone-forming and disinfectant substance into the resulting cavities, and tightly suture the wound. Sutures are removed approximately one week after surgery.
- If necessary, a specialist can cover the wound with an antiseptic bandage or place a catheter in the cavity to flush it with antibiotics. In difficult cases, it is possible to immobilize the lower jaw using plaster or plastic.
Treatment of sequestered hernia
The presence of a sequester in the spinal canal is a “time bomb”. A mobile formation with sharp edges poses a constant threat and can lead to permanent disability. Since metabolic processes do not occur in it, the sequestration resolves very slowly, therefore conservative treatment for a sequestered hernia is rarely carried out due to its ineffectiveness and danger due to the development of complications.
The structure of the intervertebral disc
Any attempts to “straighten” the sequestration are dangerous and cannot be crowned with success. Replacing surgical intervention with conservative methods very rarely bears fruit, but more often lulls the patient’s vigilance. The continued threat of damage to the spinal cord and nerves of the cauda equina while continuing to perform movements with a large amplitude leads to the development of complications, which becomes a reason for emergency surgery and an increased risk of disability.
Thus, with a sequestered hernia, surgery becomes the only way to preserve the patient’s motor ability and eliminate the constant threat. As part of the preparation for it, injections of NSAIDs, muscle relaxants and wearing a semi-rigid corset are prescribed. Sometimes blockades are performed to relieve very severe pain, but they can blur the symptoms, as a result of which the patient will not immediately notice signs of the onset of complications.
Development of sciatica due to disc herniation
If during this period complications still begin to develop, emergency surgery is required. They say something like this:
- severe pain that cannot be eliminated with medication;
- an increase in the area of numbness and an increase in paresthesia;
- increased weakness in the arms and legs;
- the appearance of signs of a local inflammatory process.
For uncomplicated sequestered hernia, the operation is performed under general anesthesia using the following types of operations:
- removal of sequestration;
- removal of the modified disc;
- installation of a prosthesis or implant instead to preserve the full functions of the spine (if this is not possible, spinal fusion is performed).
Removal of sequestration and disk
Microdiscectomy, open discectomy, and laminectomy can be used to remove the separated portion of the nucleus pulposus. The type of surgical intervention is selected based on the position of the sequester in the spinal canal. If the MRI results show relative accessibility, a minimally traumatic operation is performed - microdiscectomy.
It involves making an incision up to 2 cm in the projection of the localization of the sequestered hernia. The neurosurgeon sequentially exposes the vertebrae and facet joints. He then pushes back the ligamentum flavum and the compressed nerve and removes the sequester.
Operation microdiscectomy
If it is located in a hard-to-reach place, doctors have to resort to more traumatic procedures. Discectomy is similar to microdiscectomy, but involves creating a large access. This expands the surgical field and significantly increases the surgeon’s capabilities, but rehabilitation will be longer, and the recovery period will be up to 3 weeks. If the vertebral arches interfere greatly with getting to the sequestrum, they can be removed, i.e., laminectomy.
Prosthetics and spinal fusion
Removal of the intervertebral disc results in the formation of free space between the vertebral bodies. To close this defect, a transpedicular fixation technique can be used, i.e. installing a cage selected by size into the resulting cavity and fixing it with titanium structures to the vertebral bodies.
The most affordable way to preserve the integrity of the spine is to perform spinal fusion, i.e. fusion of the vertebrae with each other. But the use of this technique limits the mobility of the operated spinal motion segment; the patient does not lose the ability to bend or turn with normal amplitude, but will not be able to stand on a bridge.
M6L disc prosthesis
To preserve the natural biomechanics of the spine, disc replacement is used. The best endoprostheses today are considered to be M6. They are completely biocompatible and allow all the same movements as a normal intervertebral disc. They are designed in his image and likeness, but require the surgeon to accurately master the installation technique. At the same time, during their installation there are practically no risks of developing undesirable consequences, and their high strength and wear resistance ensure that there is no need in the future for repeated surgery to replace the prosthesis.
Types of sequesters
The indication for surgery is the presence of dead bone areas. During diagnosis and examination, it is important to correctly determine the type of sequestration in order to plan the course of the operation. The number, size and shape of sequesters depend on a number of factors - the extent of the lesion, the severity of the purulent process, the location of the lesion, the type of bone, the ability of the microorganism that caused the lesion to quickly destroy tissue.
This is interesting: What does a moving fragment mean and how does tooth wall removal occur?
Main types of sequesters:
- cortical – the thin bone plate under the periosteum becomes necrotic;
- central - the deep layers of the bone are affected, which receive nutrition from the diaphyseal vessels, while the surface layers remain alive;
- penetrating – affects part of the circumference of the cylindrical bone;
- total - typical for tubular bones, the entire bone is affected (it is detected immediately on an x-ray due to the characteristic picture);
- circular - the diaphysis is necrotic along the entire circumference, but in width it takes up little space;
- spongy - formed in tubular and flat bones, spongy tissue necrotizes.
How sequestra develop in chronic osteomyelitis
When osteomyelitis begins to become chronic, a sequestration box is formed. In chronic osteomyelitis, several such boxes (cavities) may form, while sequesters may or may not be present in them, but liquid pus and granulations are always present.
The boxes can be interconnected by intraosseous narrow channels, which are also infected, or be independent of each other. There are holes in the sequestration box through which pus exits into the fistula tracts. During the operation, the surgeon must clean out all cavities filled with infected contents, as well as the passages that can unite them, since they are also infected.
Acute phases, accompanied by the leakage of pus from the fistulas, pain, and fever, are replaced by remissions. Remissions last for weeks or years, but do not speak of self-healing - sooner or later a new acute phase begins. The duration of remission depends on the size and number of sequesters (and their presence in general), the size of the cavities where they are contained, the age of the patient, the type of bone that is affected, the patient’s immunity, and the activity of microorganisms that contaminate the capsules. If there is sequestration in the capsule, then the period of remission will not last long.
The remission phase is characterized by:
- weakening or complete disappearance of pain symptoms;
- improved general condition;
- bringing body temperature to normal;
- disappearance of leukocytosis;
- a decrease in ESR;
- reducing the secreted pus or closing the fistulas (if the granulations are scarred and pus stops forming).
Remission occurs after sequestration is completely completed, the capsule has formed, and periosteal bone layers have appeared.
What is a sequestered hernia
Normally, aging of intervertebral discs occurs evenly and gradually. But under the influence of aggravating factors, which include a sedentary lifestyle, obesity, heavy physical work, the load on them is distributed unevenly. The result is the development of osteochondrosis, focal dystrophic-degenerative changes in the discs and, as a consequence, first protrusion and then hernia.
Pathogenesis of disc herniation development
It can have different localization. Therefore, median, foraminal, paramedian intervertebral hernias are distinguished. If the negative effect of external factors is not eliminated, part of the nucleus pulposus, the sequestrum, is separated. It gains the opportunity to move freely along the spinal canal, which significantly complicates the diagnosis of the disease and treatment, and also poses a serious danger to the spinal cord.
Types of hernias by location
In this case, after separation of the sequester, the process of necrotization of the intervertebral disc automatically starts, since the only mechanism of its nutrition – diffuse – is disrupted. The sequester itself is also beginning to undergo changes. It becomes dehydrated, its ends become sharpened and acquire the features of traumatic cutting edges.
Since a separated particle of cartilage can either go up or down, it can easily compress the dural sac, provoke an inflammatory process, the addition of edema, and most importantly, spinal cord stenosis, injury and compression of the nerve roots. This creates a risk:
- impaired blood supply to neural structures;
- compression and ischemia of nerves;
- development of persistent paralysis;
- the appearance of severe pain.
Sequestrated disc herniation
Even a local inflammatory process can cause dysfunction of the spinal cord. After all, it is inevitably accompanied by edema, which leads to increased pressure in the central canal, reactive ischemia, epiduritis, nerve conduction disturbances, paresis or paralysis.
A sequestered hernia can be a consequence of an intervertebral hernia in any part of the spine. Since they most often form in the lumbar and cervical region, a sequestered hernia also most often originates from a disc herniation L4–L5, L5–S1, C5–C6.
Intervention techniques
Surgery is performed in two ways:
- intraoral;
- outer.
The doctor decides which of the two options to prefer, based on the specific clinical picture of the progression of the disease and the anatomical structure of the maxillofacial apparatus.
Fragments of the lower and upper alveoli are excised through the internal oral cavity. The surgeon makes a cavity trapezoidal incision and creates a periosteal flap.
Next, sequesters and granulation areas of the affected tissue are removed. This is done using a special sharp dental spoon.
After this, a biocompatible component impregnated with an antibiotic and a disinfectant composition is placed into the treated area. The formed flap is returned to its place and sutured.
Using this technology, the upper jaw body is operated on - in this case, the surgeon has an additional need to simultaneously treat the maxillary sinus.
The external option is justified for amputation of the lower jaw body and is carried out as follows:
- An external incision is made strictly at the level of the lower edge of the jaw . It should go below the border by about 2 cm.
- Having gained access to the sequester, you need to understand its size - fragments that are too large are first crushed with special scissors, and then amputated separately with a sharp spoon.
- In this case, the surface layer of the granulation areas is carefully excised.
- The formed internal cavity becomes a bed for laying bone material , after which the place is sutured in a layer-by-layer manner, and a drainage is attached to the wound for 24 hours.
Symptoms
The main sign of a hernia entering the final stage of its development is the rapid increase in neurological symptoms. Moreover, its character directly depends on in which part of the spine the degenerative-dystrophic process initially occurred.
With a sequestered cervical hernia, there is acute and severe pain in the neck and head, radiating to the shoulder girdle and arms, surges in blood pressure, weakness in the fingers, and numbness of the skin. The clinical picture often resembles a spinal stroke, i.e., there is also impaired sensitivity and mobility of the hands. If, nevertheless, a sequestered hernia provokes damage to the spinal cord, the following will be observed:
Osteocondritis of the spine
- a rapidly increasing decrease in susceptibility to pain and temperature stimuli in one half of the body or both;
- severe weakness in the legs or half of the body;
- complete lack of sensitivity below the location of the sequestered hernia, paralysis and urination disorder.
In the thoracic region, sequestered hernias rarely occur, due to the presence of a rib corset consisting of twelve pairs of ribs and the muscular-ligamentous apparatus of the chest.
Sequestered herniated intervertebral discs L4–L5, L5–S1
Most often, a sequestered hernia forms in the lumbar spine, at the level of L4–L5, L5–S1. Since the spinal cord ends at the level of the 2nd lumbar vertebra, there is initially no threat of damage. But there is another danger - damage to the structures of the cauda equina. It is a plexus of nerves, visually resembling hairs collected at one point. Each of them is responsible for the innervation of a specific area, as a result of which a sequestered disc herniation at L4–L5 and L5–S1 can cause:
Disc herniation L4-L5, L5-S1
- powerful shooting pains, aggravated by sneezing, coughing, crying or straining;
- spread of pain to the buttocks, perineum, anterior, posterior and lateral surfaces of the thighs, legs, knees and feet;
- numbness, decrease or complete loss of sensitivity of the areas for the innervation of which the affected nerve is responsible;
- decreased severity of tendon reflexes;
- decrease in muscle strength of the lower extremities;
- impaired control over emptying the bladder and rectum;
- sexual impotence in men.
The higher the sequester is located, the greater the danger it poses.
The appearance of symptoms of cauda syndrome (weakness in the legs, difficulty urinating, defecating, numbness in the perineum) is a reason to immediately call an ambulance and hospitalize the patient in a neurosurgical hospital for emergency surgery.
Preparatory stage
To determine the scope of intervention and select access to the affected tissue, a preliminary examination is carried out. This may include:
- X-ray;
- computed tomography;
- fistulography;
- skeletal scan.
Studies show the activity and stage of development of inflammation and help find previously undetected foci. CT and fistulography help to fully assess the condition of the bone structure and the tissues adjacent to it.
In addition to hardware tests, laboratory tests will also be required - a general blood test, determination of immune status, culture data and others at the discretion of the doctor.
Preoperative preparation, if necessary, lasts about 11-12 days and may include the following methods:
- sanitation of the skin in the area of surgery;
- the use of immune drugs, antigenic stimulants, hemosorption, lymphosorption to activate specific/nonspecific immunity;
- improving the functioning of major organs and systems;
- detoxification of the body;
- rinsing with antiseptic solutions/enzymes to reduce inflammation;
- physiotherapy.
Washing the fistula before surgery and the bone cavity after it with solutions of proteolytic enzymes is of great importance. The destruction of necrosis and pus using enzymes is carried out with particular efficiency, especially if after sanitation the fistula is washed with an antiseptic. Rinsing is carried out until impurities of pus disappear from the exiting liquid. This method allows you to reduce the bacterial contamination of the injury and increase the chances of a high-quality and effective operation.
Diagnostics
The best method to detect the problem is an MRI. But to obtain objective data and assess the sequestered hernia in terms of size and degree of influence on surrounding structures, it is necessary to perform a study on a tomograph with a magnetic field strength of 1.5 Tesla. or higher.
MRI machine
Computed tomography can be used as an additional research method. X-rays will be useless, since they can only show the structure of bone structures.
Anesthesia
Most often, sequestrectomy is performed with the use of local anesthetics. As a rule, the specialist chooses conduction or infiltration anesthesia.
This is interesting: Collagen membrane for teeth: features and advantages
In the first case, an anesthetic is injected into the sheath of a large nerve trunk or surrounding tissue. Thus, the specialist is able to achieve a blockade of the nerve processes in the area of the intended operation.
In the second, the doctor impregnates the tissue with an anesthetic solution during injection, while the anesthetic substance acts on the nerve fibers that innervate directly in the working area. In other words, “freezing” manages to disrupt the conduction of a nerve impulse in the right place.
For effective anesthesia, modern local anesthetics are used:
- Septanest;
- Articaine, Artifrin forte (Ultracaine);
- Alfacaine, Primacaine, Ubestizin.
Surgical technique
In acute hematogenous osteomyelitis, it is impossible to determine the size of the sequesters that will form in the future, so at this stage it is only possible to organize the unimpeded outflow of pus from the cavity. When a capsule is formed and the sequester is completely separated from the bone, sequesternecrectomy can be performed.
Sequesternecrectomy is the process of removing areas of necrosis from the bone, and it is part of a more complex and lengthy operation that includes several stages:
- exposure of the bone with which it is planned to work;
- excision of the passages through which pus approaches the fistulas;
- separation of the periosteum;
- trepanation of the anterior wall of the capsule;
- removal of sequestration, granulations, pus - extensive total sequestration is removed using a saw and nippers, incompletely rejected areas - with a chisel, large sequestration - with tweezers or sequestration forceps, small ones - by scraping with a bone spoon until a healthy layer of bone is reached;
- resection of the cavity walls within healthy tissue - a groove of sufficient size is formed, ensuring a tight fit of the soft tissues;
- tamponade of the cavity with bone chips and adjacent muscles;
- plastic – allogeneic, autogenous or xenogeneic materials are used for bone grafting;
- suturing with drainage or complete.
If radical treatment of the bone cavity is impossible, and an extensive purulent-necrotic process develops in it, suturing is performed with drainage. To do this, a tube is left in the wound, which is used for several purposes: removing pus, washing, administering medications against the growth of bacteria. If the operation is performed on a limb, it must be fixed with a plaster cast.
Surgeries for chronic odontogenic osteomyelitis of the jaws deserve special mention. In this case, anesthesia is used both general and local. The technology, in a general sense, looks the same as when working with any other bones - tissue is exfoliated, the bone structure is trepanned, sequestra are removed, and the cavity is cleaned. When stripping, it is important not to miss blind branches of the cavity or pockets. The cavity can subsequently be filled with a special sponge containing antibiotics. When stitching, a graduate is left.
If a large enough piece is removed from the jaw, it can be filled with crushed muscle, preserved cartilage, allogeneic freeze-dried bone, and other materials. It is possible to install a bone graft during surgery or subsequently in case of functional or aesthetic disorders caused by sequestrectomy.
Rehabilitation period
On average, the rehabilitation period lasts about two weeks. Immediately after the operation, the patient is prescribed vitamin therapy, antiallergic and painkillers.
To speed up recovery, bone formation stimulants are often used . As a rule, these are preparations based on calcium, fluoride salts and other substances useful for bone tissue.
If the wound site becomes suppurated or the patient’s general condition worsens, the specialist prescribes medications from the group of antibiotics.
The condition of the wound is monitored daily. Antiseptic treatment is carried out.
If no complications arise within a week, the suture material should be removed.
5 days after sequestrectomy, doctors consider treatment with ultrasound, electrophoresis, and laser appropriate.
During the entire rehabilitation period, the patient is prohibited from:
- evade compliance with medical orders;
- overwork and increase physical activity;
- violate the diet recommended by a specialist.
Possible complications
A number of unwanted problems can hinder full recovery:
- The specific structure of the bone, resembling a sponge built from bone beams with cells between them, porous fragments, and a large number of thin-walled blood vessels complicate recovery with regular bleeding. The problem is eliminated with long-term conservative treatment.
- Dehiscence of suture material. The complication occurs due to the patient’s failure to comply with rehabilitation rules (diet, decreased physical activity). Under such circumstances, doctors resort to re-suturing the wound area.
- Resumption of clinical manifestations of the disease (relapse). They develop due to the penetration of an infectious agent into the deep layers of the bone and are accompanied by the massive formation of purulent foci.
Such a negative consequence occurs in unsanitary conditions or due to medical errors during the operation.To eliminate the problem, repeated surgical intervention is necessary to eliminate the source of infection. The result is confirmed by antibiotic therapy.