Pericoronitis, or a total inflammatory process of the gums caused by infection in the oral cavity. Most often it occurs at the time of tooth eruption, especially with the growth of wisdom teeth. The process is accompanied by severe swelling of the gums, severe pain, especially when opening the mouth, as well as an unpleasant odor and unusual taste from the mouth. In addition, pericoronitis is accompanied by a state of general weakness, less often by a rise in temperature to a low-grade level. Some people also note discomfort in the digestive tract (diarrhea, among others).
Causes of pericoronitis
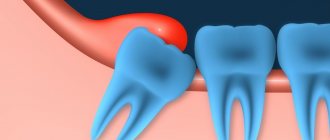
As the tooth erupts, it rests on the mucous membrane. He does not always immediately overcome this barrier. A tooth can remain under the gum from 4 weeks to 6 months or more, gradually lifting and injuring the gum. This leads to the fact that the gums cease to protect the tissues from pathogenic bacteria and small food particles; they easily penetrate under it and provoke an inflammatory reaction.
The inability to perform hygiene under the hood is the main mechanism of pericoronitis. But other factors can increase the risk of inflammation or worsen the situation:
- anatomical features of the structure of bone tissue and gums - thickened periosteum or gums, lack of space in the jaw;
- violations of the rules of oral hygiene - in this case, it is easier for bacteria to begin to actively multiply;
- trauma - damage to periodontal tissues by solid food particles, excessive brushing with bristles during cleaning;
- chronic diseases of the oral cavity - erosions and ulcers, stomatitis, gingivitis, caries, pulpitis, periodontitis, including near the erupting tooth;
- dystopic or impacted tooth, eruption at an angle, impossibility of complete eruption.
More often, pericoronitis is observed in the area of erupting eights or wisdom teeth. This is due to the fact that they appear in adulthood, when the dentition is formed and the jaw has stopped growing. At the end of the dentition there is simply no room left for a large tooth, and therefore the figure eight grows at an angle or is partially hidden by the gum. If wisdom teeth begin to erupt before the age of 20, the process is usually easy. At older ages, the process is more often complicated by pericoronitis.
Ask a Question
Development of acute pericoronitis
Acute Pericoronitis is considered as a type of acute periodontitis with primary symptoms of damage to the gum tissue. Damaged tissues located above the crown of a growing tooth involve in the inflammatory process all areas of the gums located near the resulting lesion. This course of the process is most often observed during the growth and eruption of the third, less often, fourth large molars of the lower jaw.
As a reason, experts consider both the lack of space for the formation of new teeth due to the development of a short jaw, and the abnormal development of the dental crown itself, which has assumed an incorrect location in the dentition.
Symptoms of pericoronitis
Pericoronitis of the tooth begins with pain in the gum area, which intensifies with pressure. You can usually notice discomfort when chewing or brushing your teeth. The gum area becomes swollen and red, and subsequently an unpleasant odor appears from the mouth.
In the absence of timely medical assistance, other manifestations also occur:
- spread of pain radiating to the ear, temple;
- difficulty swallowing, sore throat;
- speech difficulties;
- limitation of mouth opening due to swelling of the peripharyngeal area;
- enlarged lymph nodes;
- low-grade fever;
- swelling of the cheek due to inflammation.
A person experiences difficulty chewing food and may suffer from a general deterioration in health and headaches.
Symptoms may subside after some time, which means that the disease has entered a chronic stage. Purulent complications may also occur, and if a passage opens in the gum to remove purulent contents, the acute pain goes away. However, the inflammatory process persists.
Recommendations for patients
If an incision or excision of the hood was performed in the treatment of pericoronitis, it will be necessary to follow several preparatory and postoperative measures that will speed up healing and reduce the risk of complications.
- For two to three hours after the intervention, do not take food, hot drinks, or alcoholic drinks.
- On the day of the operation, do not go to the bathhouse, sauna, take a hot bath, or be in the sun or in a hot room.
- Limit physical activity the day before and on the day of treatment.
- During these days and the next three days, it is recommended to follow a diet, exclude alcohol, spicy, very hot foods.
- Before the intervention, you should not eat foods with a strong smell.
- Smokers should quit cigarettes the day before the hood excision, on the day of surgery, and two days after.
- For sanitation (cleaning and disinfection), you can use a mouth rinse with antiseptic solutions.
- After the intervention, the doctor will prescribe medications that accelerate healing.
- Do not apply warm compresses or ointments containing bee, snake, etc. venom.
- If after excision of the hood or placement of therapeutic turundas there is pain, severe swelling, increased discomfort, pain in the area of the submandibular lymph nodes, you need to consult a doctor to identify the cause and take action.
Types and forms of the disease
There are acute and chronic pericoronitis. Acute, in turn, is classified into the following types:
- Catarrhal. The disease begins with swelling and redness of the gums, pain, and itching. This is the simplest form of the disease.
- Ulcerative. It is characterized by the formation of ulcerations covered with a white coating on the mucous membrane of the gums, necrotization of tissue along the edges of the ulcer.
- Purulent. In the area of inflammation, serous and subsequently purulent contents are released. It is characterized by throbbing pain, general intoxication of the body, and bad breath.
Chronic pericoronitis is a consequence of an untreated acute period. With it, the symptoms become less pronounced, but serous or purulent contents continue to form. It can lead to the formation of a pathological passage through which the contents are discharged into the oral cavity. Chronic pericoronitis is characterized by periodic exacerbations; they can be provoked by tooth movement and other unfavorable factors, a general decrease in the body's defenses.
In the chronic form, lymphadenitis is often observed. The mucous membrane, even in the absence of unpleasant symptoms, is swollen and has a reddish tint. Despite the absence of serious difficulties when speaking, chewing, or opening the mouth, it is important to get help from a dentist, since the risk of complications is quite high, and the disease may not go away on its own.
Varieties
The process may differ in its severity, degree of complexity, and location. Taking these points into account, several types of pericoronitis are distinguished - acute, retromolar, isolated purulent, ulcerative, catarrhal.
Catarrhal
This case can be observed in most cases as it is the initial stage of the disease. If you consult a doctor in a timely manner, a person can avoid advanced, complex forms of pericoronitis. The symptoms are a little easier here. If a person seeks professional help in time, he will be able to stop the inflammation quickly.
Ulcerative
The reason for the appearance of this type of disease is the gum, which was inflamed and infected with fusosprirochaetes. The main symptom is a necrotic ulcerative rim along the edges of the gums. If a person removes the plaque on the teeth that covers the gums, the bleeding will become stronger. At this stage, surgical intervention is not allowed. Ulcerative pericoronitis should be treated using conservative methods.
Purulent isolated subacute
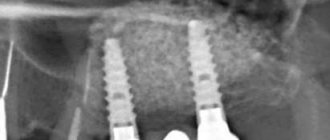
This type of disease suggests that it is a chronic form. At this stage, in the place where the tooth erupts, there is severe pain of a constant nature. And as a person chews and swallows food, it becomes stronger. Usually the temperature rises, regional lymph nodes become enlarged, and there is an inability to open the mouth. If you press down on the gum hood, pus will flow out of it. With the help of an X-ray examination, you can see that the bone tissue near the wisdom tooth is resorbing.
Retromolar periostitis
An abscess is already forming here. The symptoms resemble the previous version, but they are more pronounced at this stage. The patient's condition becomes much worse. The dentist must examine the mouth visually by forcefully opening the mouth. This type of disease involves inflammation and changes in soft tissues; it is observed in those places where the tooth erupts. If there is an infiltrate there, then the doctor makes such a diagnosis.
Acute periostitis
This type of pericoronitis has all the symptoms listed above. If it is not treated on time, the disease can become chronic. If pericoronitis persists for a long time, purulent periostatitis may occur. This condition usually appears when the lower third molars erupt.
Diagnosis of pericoronitis
Manifestations of acute pericoronitis may resemble pulpitis and periodontitis. But even an untrained person can distinguish these diseases from each other. Thus, with acute pulpitis, throbbing pain does not interfere with opening the mouth, and the gums often remain calm, without swelling and redness.
With periodontitis, swelling and redness of the gums are common symptoms. But periodontitis develops under a fully erupted tooth and is most often a consequence of advanced caries. With pericoronaritis, the tooth has not fully erupted.
A dentist can make an accurate diagnosis. Radiography is mandatory - a targeted image will help to accurately assess the condition of the tissues, the position of the erupting tooth in the jaw, the extent of the spread of the inflammatory process, and also exclude diseases with similar symptoms.
What is pericoronitis
Pericoronitis is a process during which the gum tissue becomes inflamed. A similar complication occurs when the tooth is difficult to cut and takes a long time. Pericoronitis is usually noted in relation to the wisdom teeth, which are located below. And here it is important to start treating the disease in time to avoid the acute stage.
Because there is no room for such teeth, they erupt incorrectly. When the gums are injured over a long period, inflammation begins. There are cases when the tooth has not fully erupted and is almost invisible. Pericoronitis can also develop here.
What happens if pericoronitis is not treated?
It is important to understand that pericoronitis will not go away on its own. Even if after 4-5 days the symptoms subside, this does not mean that the inflammatory process is over. From time to time the disease will go into the acute stage and cause a lot of inconvenience. In addition, pericoronitis can cause serious complications.
- Periostitis, or flux, as well as osteomyelitis. The spread of the inflammatory process to the periosteum and bone tissue can be explained by a decrease in local and general protective forces and other factors. Such complications will require serious medical intervention.
- Mobility of adjacent teeth.
- Cellulitis, abscess, lymphadenitis.
- Formation of fistula tract, cysts. The appearance of ulcerative stomatitis.
- Damage to nearby tissues, otitis, pharyngitis and other inflammatory complications in the area of ENT organs.
- Sepsis.
Therefore, treatment of pericoronitis is mandatory, regardless of the area in which the inflammation has spread. Lack of timely medical care can lead to inflammatory consequences and even loss of healthy adjacent teeth.
Prevention and prognosis
There are no specific preventive measures to prevent the development of pericoronitis. The only preventive measure is regular visits to the dentist - which will make it possible to diagnose the disease at the initial stage of development, as well as cure dental diseases that provoke the occurrence of an inflammatory process in the gum tissue.
The prognosis of pericoronitis in the vast majority of situations is favorable - timely therapy begins to achieve complete recovery, and complications develop quite rarely. However, patients should not forget about the tendency of the disease to relapse and become chronic.
Surgical methods of treatment
Treatment of pericoronitis is almost always surgical. And if we talk about molars and premolars, dentists choose the tactic of excision of the gingival hood. But treatment in the area of eights is almost always performed by removing wisdom teeth, and further we will explain why.
Excision of the gingival hood opens access to the growing tooth; this measure allows not only to remove excess inflamed tissue and thoroughly rinse the area, but also to help the tooth erupt completely and take its correct place in the dentition. This method has several conditions or indications:
- integrity of the crown and root system of the erupting tooth;
- correct location of the tooth in the bone tissue of the jaw;
- availability of sufficient space for complete tooth eruption in the row.
That is, this approach is used in all cases where the gums are the only obstacle to normal tooth eruption. If a unit of the dentition is not very healthy, for example, caries is observed, the integrity of the crown is compromised, or there are diseases of the root system, then the decision is made individually. If it is advisable to preserve the tooth, the doctor will also perform an intervention and take measures to eliminate the pathology.
Impacted and dystopic teeth, as well as situations in which complete tooth eruption will inevitably lead to malocclusion or displacement of adjacent teeth are indications for a different type of surgical treatment. The doctor may suggest tooth extraction, and in cases of disease above the “eight” level, this is almost always the only option to solve the problem.
The fact is that wisdom teeth do not bear a functional load, very often erupt at an angle, interfere with neighboring teeth and increase the risk of complications, including bite defects. Therefore, it is considered appropriate to remove the “eight” and further measures to eliminate inflammation in the soft tissues.
The only exceptions are cases when the “eight” could potentially be used as a support for a prosthesis or be important in planned orthodontic treatment.
In general, the following cases and features are indications for removal of both the hood and the tooth:
- excision of the hood has already been performed previously, but the inflammation has not gone away and/or has intensified, there is no effect from the treatment;
- the tooth does not have enough space in the dentition;
- impacted, dystopic tooth, the preservation of which jeopardizes the health of neighboring teeth and the oral cavity;
- the gingival hood grows over the erupting tooth again (this rarely happens);
- the tooth is affected by caries/destroyed, its treatment and preservation are impractical.
Since it requires the removal of a tooth that has not yet fully erupted, the procedure is considered a complex extraction. Most often, it requires preliminary dissection of the gums and extraction of the tooth from deep-lying tissues. Therefore, in many cases, sutures will be required on the gums, which will speed up tissue healing.
Surgical treatment of pericoronitis is performed under local anesthesia, so the procedure will not cause discomfort. An obligatory step is washing the mucous membrane with antiseptic solutions.
Removal of tissue hanging over the tooth can be done with conventional instruments or a laser.
Classification
Pericoronitis is divided into acute, which occurs most often, and a rarer form - chronic pericoronitis. According to the flow, the following types of pericoronitis are distinguished:
Catarrhal – characterized by slight swelling and pain when touched; Purulent - constant pain and the presence of purulent discharge; Ulcerative – leads to the formation of ulcerative defects on the gums;
Retromolar is distinguished as a separate form - it is distinguished by its location, which does not allow it to be easily seen and treated, which makes it difficult to combat this disease and increases the likelihood of complications.
Laser treatment
Laser excision of the hood provides better results. The main advantages include:
- lower risk of inflammatory complications, including secondary wound infection;
- coagulating effect of the laser - no risk of bleeding;
- short recovery period;
- reduction of pain after intervention;
- no need to additionally treat intervention areas with turundas and antiseptics.
There are few contraindications for laser intervention, one of them being cancer.
Diet for the treatment of pericoronitis
Proper nutrition is part of the treatment of pericoronitis; compliance with certain rules is required not only after surgery to excise the hood, but also after removal of a wisdom tooth. To speed up the healing of the mucous membrane, it is recommended:
- Exclude rough foods from the menu, for example, crackers, chips, nuts.
- Raw vegetables and fruits need to be washed well so that there is no soil or other particles left on them that can become a source of infection.
- Do not consume spicy, sour and salty foods, carbonated drinks, or alcohol.
- The temperature of food and drinks should be around 37°C; hot and cold food is prohibited.
- It is better to chop all food before consumption, especially raw carrots, apples, and cucumbers. You need to try to introduce more soft and liquid dishes into the menu.
It is also recommended to follow these rules:
- After the operation is completed, you must refrain from eating for 2-3 hours.
- While eating, do not open your mouth wide to prevent the sutures from coming apart.
- Do not chew on the side of the surgical procedure.
Otherwise, there are no restrictions; after a few days, provided the mucous membrane has successfully healed, you can return to your normal diet.
Surgical intervention: removal of the dental hood
The following techniques are used in dental practice:
- Pericoronarotomy. The procedure is performed under local anesthesia. It involves removing the gingival hood in order to eliminate purulent exudate.
- Pericoronarectomy. A surgical intervention that involves complete excision of the overhanging tissue. With this technique, the lateral surfaces of the tooth may be exposed.
- Extirpation. Extraction of an element of the dentition by sawing and subsequent removal of the pocket and dental unit. The hood is removed from the tooth and all manipulations are performed under local anesthesia.
Dentists at the Alpha Dent clinic provide professional treatment of pericoronitis. They are ready to provide qualified assistance of any level of complexity, will help solve the problem, speed up recovery and shorten the rehabilitation period.
Excision of the hood over the wisdom tooth
If there is an acute period of the disease or it develops again, the doctor usually recommends a simple surgical operation - excision of the hood. This is the name given to the muco-subperiosteal flap, which partially covers the tooth. A pocket is formed under it, in which food debris accumulates. By rotting, they turn into a nutrient substrate for pathogens. The situation is aggravated by constant mechanical impact on the gums.
Careful excision of the hood over the wisdom tooth allows you to open the surface of the molar and eliminate the source of infection.
Procedure to complete:
- Primary elimination of inflammation with medications.
- Anesthesia (usually local) and excision of the hood with a surgical scalpel.
- Antiseptic treatment.
After excision of the mucous hood is completed, patients are advised to refrain from food and hot drinks for 1-2 hours, as they can cause pain and infection of the wound. To completely eliminate the consequences of the disease, the doctor prescribes anti-inflammatory drugs, rinses, and physiotherapeutic procedures.