04.01.2020
The operation to remove the nerve of a tooth is familiar to almost everyone who treated teeth in Soviet times or in the 90s. Not surprisingly, most people associate this procedure with arsenic being placed inside the tooth, followed by pain for several days. The memories are terrifying... But is it worth it to be afraid of this procedure now, when the modern industry has made a significant leap forward and modern dental services have appeared in all cities.
The first thing worth saying is that arsenic is a thing of the past. In addition, dentists use modern equipment and innovative materials, including for removing the nerve of a tooth. As a result, the process takes much less time, and the procedure itself is absolutely painless.
Removing the nerve allows you to protect other teeth and maxillofacial tissue from further development of the inflammatory process and the appearance of infectious diseases of the oral cavity.
First, we suggest you figure out what the nerve of a tooth is and when can a dentist decide to remove it?
Why does deep caries develop?
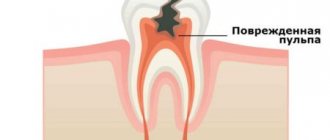
The process of tooth decay under the influence of microorganisms and other factors is caries. Its onset and development is caused by the activity of pathogenic microflora of the oral cavity, in particular the bacteria Streptococcus mutans. They feed on sugars from food, cause fermentation and produce acid. It corrodes tooth tissue, which leads first to demineralization of the enamel, then to deformation of its structure and the formation of carious cavities. Gradually, the process spreads deeper and affects dentin - the bone tissue under the tooth enamel.
Caries most often does not develop at lightning speed and goes through several stages. First, a barely noticeable chalky spot forms on the enamel - an area that is different in color from the rest of the tooth. This is the area of demineralization where the carious process began. Enamel loses the mineral compounds that make up its structure, becomes more fragile and less resistant to harmful influences. This is the initial stage of caries - the spot stage. People often miss it due to the lack of obvious symptoms. Then tooth decay continues, and the disease progresses to the stage of superficial caries. The tooth begins to react to hot/cold, sour/sweet, and a clear defect is noticeable in the enamel.
Without treatment, superficial caries progresses to intermediate caries when dentin begins to deteriorate. Symptoms become more pronounced, pain occurs not only as a reaction to an irritant, but also on its own. According to statistics, most patients seek help from a dentist at the stage of average caries.
But there are also people whom even acute toothache will not force them to go to the dentist. And then the most complex and advanced form can develop - deep caries. At this stage, the carious cavity is in close proximity to the dental pulp; at any moment, inflammation can spread to the dental nerve and lead to pulpitis, and then to periodontitis.
Causes of tooth pain after depulpation
Individual reaction of the body
It may appear in the first two days. Even after removal of the nerve, the tooth is still able to respond to strong pressure and thermal irritants, but not longer than 3-4 days. Poor quality of pulp extractors or inability to handle them
Instruments for pulp extraction are marked because they must correspond to the canal. Poor quality of canal cleaning
The presence of tissues damaged by caries will certainly lead to renewed pain and complications of the inflammatory process, so it is extremely important to remove them completely. Allergic reaction to filling materials
This rarely happens, especially if the doctor has determined in advance the patient’s body’s predisposition to allergies. Instrument fracture
If the instrument was damaged during the procedure and its remains lingered at the top of the root, they will cause pain. In the worst case, if there is already a filling, the tooth will need to be removed. Residual pulpitis
May affect one or more canals. The main symptom of such a secondary inflammatory process is aching pain, which then becomes acute. Relapse is possible with partial depulpation.
Treatment options for advanced caries
Treatment tactics for deep caries will depend on a number of factors. The dentist takes into account the patient’s condition, the presence of toothache, and complications.
Depending on these factors, treatment of caries with removal or preservation of the nerve may be recommended. In deep caries, the pulp (neurovascular bundle) is located in close proximity to the carious cavity. Between them there is only a thin layer of dentin. If the doctor is sure that the pulp is not infected, he can cure the carious lesion in one visit. If there is a possibility of developing pulpitis, then at least two visits will be required.
Contraindications
Before treatment, the doctor must collect medical history data, that is, all information about the patient’s health status. Contraindications to nerve removal may include:
- pregnancy (first and last trimesters);
- hepatitis, HIV infection;
- open form of tuberculosis;
- acute inflammatory diseases of the oral mucosa.
It is worth noting that in case of acute pain, some contraindications can be considered relative: the decision is made by the dentist.
Treatment without nerve removal
After making sure that the pulp is not infected, the dentist will not remove the dental nerve. In this case, treatment is carried out according to the following scheme:
- The patient is given an anesthetic injection, after making sure that he is not allergic to anesthesia.
- Using a drill, the tooth is prepared and all affected, necrotic tissue is removed.
- Next, the doctor carries out medicinal treatment of the tooth with antiseptic drugs.
- Thoroughly dry the prepared cavity with an air stream.
- A therapeutic or insulating pad with eugenol, calcium hydroxide or other substances is installed at the bottom of the cavity. This is the most important stage in the treatment of deep caries, because the lining protects the pulp from pressure and other negative influences from the filling, and also has an antimicrobial effect and stimulates the growth of the dentinal layer between the bottom of the cavity and the pulp. Installation of a gasket for deep caries is carried out in 95% of cases, although if the walls and bottom are sufficiently thick, the doctor may decide to fill the tooth without a therapeutic gasket
- The next step is installing the seal. Fillings made from light-curing composites are considered one of the most reliable and durable. This material is applied layer by layer to the tooth and each layer is illuminated with an ultraviolet lamp. Light fillings almost do not sag, have high strength and good aesthetic characteristics, therefore, when treating deep caries, it is recommended to use just such a filling material.
- At the last stage of treatment, the filling is aligned to the bite, polished and ground smooth, giving the tooth a natural anatomical shape.
If the dentist suspects infection of the pulp due to deep caries, he will not immediately place a permanent filling. After dissection and removal of the affected tissue, he will apply medication and install a temporary filling. If toothache does not appear within four days, then there is no pulpitis, and the doctor will replace the temporary filling with a permanent one. If increasing pain appears during this time, the patient probably has pulpitis. In this case, pulp inflammation is treated using the optimal method, and only after that the tooth is covered with a permanent filling.
After treatment of deep caries in a tooth with preserved pulp, moderate pain may be felt, which occurs when chewing and normally goes away after a couple of days. If the pain persists longer and intensifies, you should definitely consult a dentist.
Possible complications after depulpation
After the procedure, you may experience:
- Canal bleeding. The main reason for this phenomenon is the separation of the pulp by the pulp extractor. To avoid this problem, dentists practice gradual cutting of soft tissue using files and copious rinsing with an antiseptic. Only a doctor can stop canal bleeding.
- Short-term pain. Their duration may vary, but if they do not go away for a long time, it is necessary to re-open the canals and disinfect them.
- The appearance of a cyst, granuloma, gumboil or fistula.
- Facial paralysis. May occur due to improper application of material. If it protrudes beyond the upper part of the root, it will not only affect the tooth, but also compress the nerve of the jaw. That is why if you have pain in the chin area, you should immediately consult a dentist.
If disinfection is of poor quality during pulp removal, there is a risk of suppuration and the development of periodontal abscess. In this case, tooth extraction cannot be avoided.
How to treat deep caries with pulp damage?
Caries complicated by inflammation of the pulp is treated in several stages. In case of inflammation at an early stage, the dentist may try to preserve the pulp completely or partially, in which case antibiotic therapy is carried out. But most often, in case of pulpitis, the nerve is removed, and the root canals are cleaned and treated.
Further treatment tactics depend on the individual characteristics of the disease. Root canals are often filled, after which a filling is placed in the crown of the tooth. If your own tooth is severely damaged, a stump inlay or an artificial crown is installed.
Treating deep caries while preserving or removing the nerve is difficult, expensive and time-consuming. Therefore, we do not recommend starting the carious process to such an extent that the nerve needs to be removed. The best option is to consult a dentist at the first signs of the disease, and if there are no complaints, visit a professional examination twice a year.
What does tooth color change mean after pulp removal?
Nowadays, almost all private dental clinics adhere to international depulpation protocols, but outdated practices are still in use in budgetary medical institutions. The main reasons for tooth discoloration are improper preparation of the cavity for installation of a filling, poor quality of instrumentation of the canal and poor materials for filling. For example, when using endomethasone, the enamel turns yellow (a similar outcome is even prescribed in the instructions). If resorcinol-formalin paste was used for filling, the teeth may turn pink. Most often, this material is used in the treatment of baby teeth.
The nerves from wisdom teeth, which dentists call “problem eights,” are extremely rarely removed. Given their location and short service life, as well as the difficulty of cleaning from stone and plaque, they are easier to remove. As a rule, the figure eight is removed in case of incorrect eruption (if there is a slope towards the tongue or towards the cheek), tooth retention, carious lesions, pulpitis, changes in bite, displacement of the dentition.
After depulpation, you should adhere to the following recommendations:
- Avoid physical activity for the first 2 hours after the procedure.
- To avoid infection and injury to the tooth, do not eat food for 3 hours after pulp removal (you can drink warm water through a straw).
- For 5 days, exclude rough, solid foods from the diet.
- To avoid irritation of the oral mucosa, it is advisable not to smoke, drink alcoholic beverages, or eat spicy, cold or hot foods for at least 5 days.
- Rinse your mouth with antiseptics prescribed by your dentist for at least 1 day.
It is impossible to remove the dental nerve using folk remedies. Even if it can be destroyed, the pulp will need to be removed, and this can only be done with a special medical instrument.
When planning a visit to the dentist, remember that the longer you delay, the more difficult and expensive depulp removal will be. And do not forget that such intervention is recommended only if there are good reasons for it. Any dentist will try his best to keep the tooth “alive” if possible.
Activities before visiting the doctor
If the tooth hurts and it is obvious that nerve removal cannot be avoided, you should immediately make an appointment with the dentist. To relieve pain in the period before your visit to the office, you can perform a number of manipulations. Pain can be reduced or relieved by:
- Carefully remove food debris from the cavity in the tooth.
- Rinse with warm soda solution.
- Avoid chewing food on the affected side.
- Minimize exposure to high and low temperatures (including cold air).
- Mouth slightly open. If the bite is incorrect, closing the jaws may increase the pain.
- Painkillers.
PROMOTION
Inexpensive dentistry
Prices are 1.5-2 times lower
Second visit:
By the way, it is preferable to fill root canals without anesthesia, but this is not necessary. This is due to the fact that if a slight pain occurs when filling the canals, the doctor immediately understands that he has moved the gutta-percha pin beyond the apex of the root. Accordingly, the doctor can change the filling depth in time.
- Removing a temporary filling.
- Flushing the canals with antiseptics.
- Filling canals using gutta-percha and sealer - after the root canals have been washed and dried, it is necessary to seal them tightly.
This is done using gutta-percha pins of different sizes (Fig. 16) and a sealer (this is something like a paste). The pins are inserted into the root canals and compacted there. In Fig. 14-15 you can see the mouths of the root canals Before and After the canals were filled with gutta-percha. Read more about this stage in our article: → “Mechanical treatment and filling of canals for pulpitis”
- X-ray control of the filling ( required!!! ) if everything is OK on the x-ray, we proceed to the next stage.
But, if we see that the canal is not filled up to the apex, or the gutta-percha pins extend beyond the root into the surrounding tissues, it is necessary to remove all the gutta-percha pins and start filling the canals all over again. In Fig. 17-19 you can see well-sealed root canals (all root canals are sealed to the apex of the root). Unfortunately, it is worth noting that the vast majority of dentists, even if they see that the root canals are filled, do not redo the work. This is precisely what is connected with the percentage of poor-quality treatment of pulpitis that we announced at the beginning of the article (in 60-70% of cases). Type of high-quality filled root canals –
At the end of the visit, a temporary filling is placed, and the patient is warned that the tooth may begin to hurt after undergoing anesthesia. Good tablet analgesics will help relieve pain. A little pain is normal because... during instrumental work in canals, K-files slightly injure the tissue in the area of the root apex.