Manifestation of periodontitis
Periodontitis is not difficult to recognize. It manifests itself in the form of periodontal inflammation. These are the tissues surrounding the root of the tooth. They are located next to the alveolar socket. The disease manifests itself in the form of unpleasant sensations when eating and chewing any food. Hot and cold foods sometimes cause acute, unbearable pain.
Outwardly, in the early stages, the disease may not manifest itself. But in a neglected state, blisters appear on the gums, and pus gradually leaks from the deep periodontal tissues and enters the oral cavity.
At the first symptoms, the main thing is to prevent inflammation from developing further. Exacerbation can lead to subsequent tooth extraction.
Subsequent development of the disease can contribute to the appearance of:
- dental granuloma;
- cysts;
- sepsis;
- osteomelitis.
The first signs of periodontitis:
- Swelling of the gums.
- An enlarged lymph node in the area where the source of the disease is located.
- Severe pain at the point of touching the affected area of the tooth (near the root tissue).
- Constant pain when eating food, especially hot food, including drinks.
- Feeling unwell in too hot weather.
- Weakening of gum tissue.
- Loose teeth.
The inflammatory process develops gradually. At first, the patient feels mild pain when chewing food. He then notices how his gums have become looser, especially in the affected areas. The appearance of granules on the surface of periodontal tissue can develop into the development of a fistula, pus from which will periodically leak into the oral cavity. After this, the patient will feel better, but then the disease will return again.
Teeth with periodontitis become darker. X-rays during a dental examination can reveal destroyed dentin and bone tissue.
CAUSES AND DESCRIPTION OF PATHOLOGY
The disease is caused by pathogenic bacteria that attack the periodontium, a fibrous tissue with a dense network of capillaries and nerve endings located between the root cement and the alveoli. Infection occurs as a complication of deep caries, when pathological microorganisms reach first the pulp and then the periodontium. In areas of bone tissue destruction and constant inflammation, pathological granulation tissue begins to form and grow rapidly.
Another reason may be unskilled filling of root canals, penetration of aggressive materials and pastes into the periodontal tissue that stimulate the growth of colonies of anaerobic bacteria.
Types of periodontitis
p>Treatment of the disease depends on the degree of its development. To do this, you need to know about the different types of periodontitis. These include:
- Fibrous. Chronic stage. Diagnostics show that this disease often affects older people, whose periodontal tissues lose their strength over time.
- Granulating periodontitis. One of the most dangerous types of diseases. Usually the disease develops when there is no treatment for caries. Leads to the appearance of granular formations on the gums, which can subsequently grow.
- Granulomatous. Characterized by the appearance of formations in the area of the tooth root.
The disease can occur in three stages: acute, chronic or acute. In the latter case, periodontitis is chronic, but sometimes signs of exacerbation of the disease appear, followed by remission.
Diagnostics
The diagnosis is carried out by a doctor in a dental office. The process begins with listening to the patient's complaints and collecting an anamnesis, and this is followed by examination of the oral cavity, palpation of the site of inflammation and x-ray examination.
Granulating periodontitis has three stages of disease development:
- Swelling and bleeding of the gums, rapid formation of tartar.
- The necks of the teeth become exposed and become sensitive to external influences.
- An inflammatory process begins, causing destruction of bone and connective tissue.
Treatment methods for periodontitis
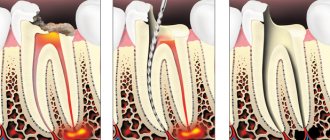
Chronic periodontitis, like the disease in its acute form, should be treated immediately after its detection. However, the ways to combat it differ depending on the type of disease. The standard algorithm for getting rid of the problem includes:
- Preparation. First, the doctor takes an x-ray to check the root canal.
- Nerve removal. Depulpation is required to further clean the canal.
- After drilling the tooth, the nerves are removed and the canals are cleaned. The old filling is also removed.
- Sometimes expansion of channels is required. Depends on the stage of the disease and the shape of the tooth.
- After treating the canal with an antiseptic, temporary filling is performed using special medications.
- Next is the reuse of antiseptics.
- If the inflammation has subsided, a permanent filling is applied.
- An x-ray is taken to monitor the outcome of the treatment.
Treating the disease is not as easy as it seems. Sometimes a temporary filling can be applied several times, and treatment can continue for several months. It depends on the severity of the disease and the experience of the doctor. Therefore, it is important to contact practicing specialists in licensed clinics.
Doctor's orders during therapy
At the beginning of treatment of periodontitis, a specific medicine such as Crezofen, which is considered an excellent antiseptic, is usually placed inside the opened tooth canals.
Additionally, rinses with Miramistin or analogues are prescribed, a drug against the development of allergic reactions (Suprastin, for example) and an anesthetic are suggested.
If necessary, the doctor prescribes antibiotics if he sees that the situation is advanced and almost borders on sepsis. A locally acting antibiotic like Lincomycin, which is routinely preferred by dentists, is not suitable here. You will need weapons of mass destruction of bacterial microflora - Ciprofloxacin, Augmentin, Amoxicillin, etc.
If the patient experiences undesirable changes in health status or increased pain, it is recommended not to delay going to the hospital.
In case of exacerbations of chronic periodontitis, when the acute picture of the disease is leveled, therapy involves the installation of temporary fillings in the root canals. This is both obstruction and treatment at the same time. Calcium hydroxide, which is part of the filling material, acts as the basis for the regeneration of bone tissue in the area of inflammation. This procedure takes up to 90 days and all this time a temporary filling in the canal promotes healing of the affected area.
Such conservative therapy for small granulomas becomes a great help for the doctor in healing the disease and allows, in most cases, to avoid traumatic surgery. However, intervention cannot be avoided if the diameter of the cyst exceeds one and a half centimeters. It is not possible to heal formations of this size in a gentle way.
Complications of periodontitis
Periodontitis itself is dangerous due to tooth loss and significant deterioration of periodontal tissue. The disease is characterized by a rapid transition to chronic stages, which lead to more severe oral problems.
Exacerbation of granulating periodontitis can lead to the formation of an odontogenic fistula. These are holes on the mucous surface through which pus comes out.
The danger is that the appearance of a fistula is not always limited to the oral cavity. In dentistry, there are cases where fistulas due to periodontitis appear on the cheeks and the outer surface of the face. This causes discomfort and worsens the appearance of patients.
The appearance of a fistula is characteristic of the chronic course of the disease with alternating stages of exacerbation. When the pus passes through the fistula canal, the patient feels lighter. A period of remission begins.
However, soon the pus appears again, the pain increases and becomes more frequent, and the tooth tissue continues to rapidly deteriorate. Therefore, you should not expect that after the first release of pus from the fistula canal, the disease will recede on its own.
Surgical methods
The arsenal of a dental surgeon in the treatment of periodontitis includes the following manipulations:
- Opening the gums - used to facilitate the drainage of pus that has accumulated at the apex of the root and caused the formation of an abscess on the gum.
- Hemisection is an operation to remove the root of a multi-rooted tooth, at the apex of which a focus of inflammation is found, while at the same time the crown part of the tooth adjacent to the root is removed. The canals of the remaining roots must be thoroughly treated before surgery. The hole remaining after hemisection is filled with osteoplastic material, and the mucous membrane is sutured. The tooth is later covered with a crown.
- Root amputation is an operation to remove the root of a multi-rooted tooth, but preserving the crown part.
- Root apex resection – the root apex is removed through a hole formed on the outer surface of the jaw in the area of the projection of the root apex of the diseased tooth. The operation is often performed in combination with cystectomy - removal of a granuloma or cyst. The cavity formed after their removal is filled with osteoplastic material. Also, resection is indicated if it is not possible to unseal the canal (provided that it is thoroughly sealed throughout its entire length, except for the apical part).
- Tooth replantation is a complex operation that involves removing a tooth and then returning it to the socket after curettage of the alveoli, filling of the canals and resection of the apex (sometimes resection is not performed). The method is used on multi-rooted teeth, the healing of the replanted tooth can last up to 10 weeks, during which time the tooth must be kept at rest using splints or trays. Even with successful engraftment, a replanted tooth must be removed on average after five years due to root resorption and loss of stability.
- Tooth extraction – if it is impossible to use other methods of treating periodontitis, they resort to tooth extraction. Subsequently, it is recommended to carry out implantation - implantation of an artificial root (implant) with further installation of a crown. Thanks to implantation, full chewing function is preserved, and the appearance of the artificial tooth does not differ from the natural one.
Modern methods of treating periodontitis allow, in most cases, to save the tooth, but if the patient seeks dental care late, it may be lost. To avoid unpleasant consequences, you need to monitor your dental health, conduct timely preventive examinations of the oral cavity and treat identified diseases.
Prevention of periodontitis
Periodontitis is usually a consequence of advanced caries. Therefore, at the first sign of problems with your teeth, you need to start treating them. In people aged 50 years and older, problems with periodontal tissues are more common. Therefore, they should take more care of the oral cavity: the disease can progress more rapidly, with severe pain syndromes.
To avoid getting periodontitis, you should go to the dentist every 5-6 months to remove caries at its first manifestations. Cleaning stones should also become a regular hygiene procedure.
Rehabilitation period and prevention
To speed up the healing process, in some situations the patient is prescribed a course of antibiotics and vitamin complexes in order to enhance the natural protective functions of his body. Special medicinal baths and mouth rinses may be prescribed to relieve inflammation.
Following simple preventive measures will help prevent the disease. It is necessary to follow the correct diet - food should be rich in vitamins and minerals. Be sure to brush your teeth with a suitable toothpaste and brush. It is recommended to stop smoking, as well as drinking alcohol, coffee and carbonated drinks. And, of course, even after complete recovery, it is necessary to visit the dentist regularly twice a year.
Features of the pathological and clinical picture
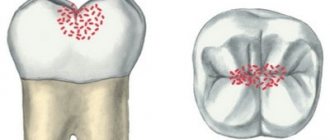
Granulation tissue grows unevenly, and many cellular elements are formed. Partial osteoclastic resorption of bone tissue is observed. The cement and dentin of the affected teeth also dissolve.
The disease often occurs without pain. There may be complaints about the formation of a fistula and pus, and there is also a change in the color of the crown. A closed carious cavity with softened dentin appears in the tooth. This is explained by the fact that at this age, caries, as a rule, is acute, and the pulp does not sufficiently perform a protective function, so periodontal infection occurs very quickly.
The hard tissues of baby teeth differ from permanent ones. Their enamel and dentin are thinner, the degree of mineralization leaves much to be desired, and the dentinal tubules are shorter and wider.
Causes of dental periodontitis
Various reasons can lead to the appearance and development of dental periodontitis, but in the vast majority of cases the disease appears:
- Against the background of untreated dental caries and pulpitis;
- Due to poor quality treatment of tooth canals, or more precisely, mistakes made when filling the canals.
Less commonly, periodontitis occurs after injuries, incorrectly installed dental fillings, or violation of the dosage of dental medications.
Whatever the cause of periodontitis, its treatment cannot be delayed due to fear of dentists. It is important to understand that you will not stop the inflammation on your own, with pills or folk remedies, and the more it progresses, the less chance you have of saving the tooth. In addition, periodontitis can also affect neighboring healthy teeth.
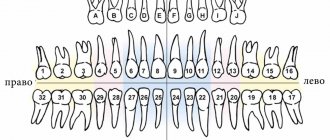
How to identify periodontitis and not confuse it with caries or pulpitis? We already talked about the most striking symptom of the disease at the very beginning of the article, but the signs of periodontitis may vary depending on the form of the disease. Therefore, below we will consider the main types of dental periodontitis, as well as talk about their characteristic symptoms.
Take a short test and calculate the cost of treatment!
Take a short test
- Which teeth have caries?
- Visual assessment
- Reaction to stimuli
- Cost calculation
×
Manukyan Artavazd Genrikovich
Chief physician of the clinic
Chronic periodontitis? Neomed Clinic will help!
No matter how chronic periodontitis hides under different masks, the Neomed clinic will professionally eliminate it. We know the features of granulating, granulomatous and fibrous forms, and correct diagnosis and identification of causes determine the effectiveness of treatment.
Symptoms can be superficial, so it is problematic to identify chronic periodontitis on your own. The Neomed clinic will help diagnose the disease and say goodbye to troublesome microbes forever.
Symptoms
The pathology is characterized by periods of relapse and recession. During the recession, there are no signs of the disease. During the period of dynamic development, the patient experiences paroxysmal pain in the affected unit, increasing with temperature or mechanical influence, as well as the following symptoms:
– swelling, redness of the gums;
– mobility of the problem unit;
– enlargement and pain of the lymph nodes on the part of the diseased tooth;
– the appearance of a fistula at the site of the infiltrate, from which purulent or serous fluid oozes.
With a long course of the disease, the patient experiences general weakness, headaches that get worse when moving the head, increased body temperature, decreased appetite and irritability.
Those around you may notice darkening of the diseased tooth and an unpleasant odor from the mouth.
Diagnostics
To separate the granulating form of periodontitis from the fibrous or granulomatous form, electroodontodiagnosis is performed, which demonstrates an increase in the threshold of pulp excitability. Using radiography, the diagnosis is confirmed, since the image demonstrates the presence of pathology and its shape.
At the initial appointment, the doctor determines the pathology based on the following symptoms:
– the tooth is largely destroyed;
– the problem unit has a dark shade;
– the caries cavity reaches the root canals;
– there are incorrectly installed fillings, crowns and bridges.
When probing the cavity, the patient does not feel pain; he experiences minor discomfort during percussion. When pressed with an instrument, a depression is formed in the gum, and the soft tissue may turn pale.
Treatment
After diagnosing chronic granulating periodontitis, the following measures are carried out:
- remove pus;
- treat and disinfect the canals;
- restore damaged bone tissue;
- cement the cavity;
- restore the crown (install a prosthesis).
When removing the pus, the fistula is incised under local anesthesia.
If inflammation occurs under the filling, it is removed, expanded and the cavity is cleaned.
For high-quality disinfection, antiseptic drugs are administered for a certain period, protecting the cavity with a temporary filling.
Contraindications to treatment
Absolute contraindications for this type of treatment include:
- Severe changes in periapical tissues (cyst, cystogranuloma) with the presence of focally caused ailments.
- Obstruction of the canals at the acute stage.
- Tooth mobility of 1I-IV degrees, when the alveolar arch at the level of the diseased tooth has atrophied.
- Cysts of peri-root teeth with root penetration into the pathological process.
- Irreversibility of the course of the disease and the impossibility of performing post-apical therapy.
- Perforation of a cavity or tooth root.