Granuloma annulare
Granuloma annulare is a benign dermatological disease of an often relapsing nature, in which dense rashes slightly raised above the skin, resembling a ring in shape, appear.
The nodules are usually pink in color, but can be flesh-colored or bluish in color. There are single and multiple. Granuloma annulare of the skin is a fairly rare disease, diagnosed in 0.3% of patients who consult a dermatologist. Most often these are school-age children and young people, less often adults. In men, the disease occurs almost 2 times less often than in women.
Classification of granulomas and forms
In medicine, granulomas are classified according to several criteria: etiology, pathogenesis and morphology. Specific varieties are collected in a separate group. In the group according to the criterion of etiology there are types of established and unidentified etiology: infectious and non-infectious. The latter include dust granulomas, drug-type granulomas and neoplasms around foreign bodies. Pathogenesis group: immune and non-immune. The first type includes epithelioid cell granulomas. Non-immune ones occur due to toxic factors and acute infections. The morphological group is divided into two main groups: mature and epithelioid cell. According to the morphology of granulomas, there is the formation of a diffuse-type granulomatous infiltrate and the formation of tuberculoid-type granulomas.
Main types of granulomas
In medical practice, there are many types of neoplasms of this type. They can be single or multiple. It is not always possible to see the beginning of their formation, since pathogenic cells are located deep in the layers of the dermis. Granuloma in children and adults can appear and disappear without treatment. This should justify the need for gentle therapy in the future. Granulomas of the following type are most often diagnosed in children and adults:
- ring-shaped;
- pyogenic;
- tuberculosis.
Causes of granuloma annulare
The etiology of the disease has not been precisely established, but it is assumed that pathologies of the immune system underlie its development.
Granuloma is not associated with systemic disorders, except in cases of multiple rashes in adults, in whom a disorder of glucose metabolism is often detected.
It is believed that the manifestation of the disease may be a reaction to the following risk factors:
- introduction of tuberculosis vaccine (BCG);
- performing a Mantoux test;
- insect bites;
- exposure to ultraviolet rays;
- overdose of vitamin D;
- skin injuries;
- viral infections;
- tick-borne borreliosis;
- diabetes;
- autoimmune thyroiditis;
- tuberculosis.
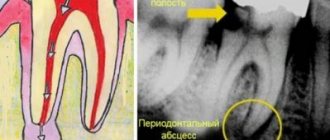
Granuloma on the root of the tooth
Periapical and apical granulomas are those that develop at or around the apex of the tooth root. They consist of a proliferating mass of granulation tissue inhabited by bacteria. The formation of “dental” granulomas is an attempt by the body to stop the spread of the infectious process from the teeth to other organs and tissues.
Periapical granulomas grow slowly. They can reach several centimeters in diameter. Small formations (several millimeters in diameter) do not have clearly defined boundaries and are therefore difficult to identify. Typically, periapical granulomas do not show any symptoms. Only an associated secondary infection can trigger the development of pain.
Granuloma of the tooth root apex is a manifestation of apical periodontitis with the formation of granulation tissue. The main factor in the formation of granuloma on the tooth root is a bacterial infection. A capsule of collagen fibers forms around the granuloma. When a tooth is removed, the sac-like formation is usually removed along with the tooth.
Removal of granuloma on the tooth root is carried out by apical resection. Unfortunately, the only alternative is tooth extraction.
Types and symptoms of granuloma annulare
There are four forms of the disease, differing in clinical picture:
- Localized is the most commonly diagnosed granuloma (about 90% of all cases, especially in childhood). It is characterized by the appearance of small (up to 5 mm) dense hemispherical nodules of flesh-colored or pinkish color, smooth to the touch. They are arranged in the form of an arc or ring, touching each other. Typically appear on the extensor surfaces of the hands and upper arms, legs and feet. Sometimes the scalp and area around the eyes are affected. Gradually, the lesions increase in diameter, reaching 5 or more centimeters. In the center, the skin may be normal or have a bluish tint. There are no signs of epidermal damage.
- Subcutaneous granuloma annulare differs in that the nodules form not on the skin, but in the subcutaneous layer. Nodules can be either single or multiple. They appear on the back of the hands, upper arms (up to the elbows), scalp, legs, fingers, and less often in the area around the eyes. This granuloma annulare occurs in children only before the age of 6 years. May recur if removed.
- Disseminated granuloma is characterized by the appearance of multiple purple rashes of different shapes and sizes on different areas of the skin. The disease is almost always diagnosed in adults; it rarely affects young people. The formations can be scattered and merging, due to which the lesions acquire a multiform character, are rarely located in a ring-shaped position, and symmetry is a typical feature. Disseminated granuloma annulare is prone to a chronic relapsing course. Resistant to standard treatment.
- The perforating form occurs in only 5% of cases, mainly in children and young adults. Papules appear on the skin, which merge into large plaques. There is a “plug” in the central part of the hearth. When you press on it, the contents of a jelly-like consistency are released. Then the plaque becomes covered with a crust and acquires a relatively flat surface with a slightly depressed center. In its place, atrophic scars may subsequently form.
Laboratory and instrumental diagnostics
A general blood test may show an increase in ESR, eosinophilia, leukocytosis, and a decrease in hemoglobin levels.
The use of various imaging methods (radiography, CT, MRI) allows us to identify foci of destruction up to 5 cm in size with clear boundaries without sclerotic changes, sometimes pathological fractures, flattening of the affected vertebrae (vertebra plana).
Pathomorphological examination is of decisive importance in the diagnosis of histiocytosis in adults and children. Microscopy reveals infiltrates of Langerhans cells (large oval cells with irregularly shaped nuclei), eosinophils, lymphocytes, and macrophages. Immunohistochemical analysis reveals the expression of CD1a, langerin, and S-100 proteins, characteristic of Langerhans cells. Electron microscopy allows one to see the Birbeck granules characteristic of Langerhans cells.
Differential diagnosis for EG is carried out with osteomyelitis, primary tumors or metastatic bone lesions, lymphoma, multiple myeloma, Papillon-Lefevre syndrome and bone cysts.
Figure 6. Birbeck granules, characteristic of Langerhans cells (electron microscopy data)
Treatment of granuloma annulare
Since the nodules usually do not cause any discomfort, therapy may not be required. When planning treatment, it is recommended to take into account the tendency of the disease to spontaneously resolve within 2 years. Relapses occur in approximately 40% of cases, however, new nodules can disappear spontaneously.
If formations create an aesthetic problem or are accompanied by atypical manifestations, you should consult a dermatologist. If any skin formations are detected in a child, it should be shown to a doctor.
The doctor decides how to treat granuloma annulare, depending on the form of the disease, its location and prevalence, as well as the age of the patient.
For rapid healing of the skin, external medications can be prescribed. Effective creams and ointments for granuloma annulare contain corticosteroids: hydrocortisone, betamethasone, methylprednisolone, mometasone, clobetasol. During the first 2 weeks, the drug should be applied to the affected areas once a day. Over the next 2-3 weeks - once every two days. In rare cases, intradermal administration of corticosteroid drugs is required.
Additionally, patients are recommended to take oral vitamin E or ascorbic acid and rutin.
If external therapy with glucocorticosteroids does not produce the expected effect, topical calcineurin inhibitors are prescribed in the form of ointments (pimecrolimus or tacrolimus). They should be applied twice daily.
To treat all forms of granuloma in adults (they are not recommended for children), physiotherapeutic methods can be used: ultraviolet irradiation, phototherapy, PUVA therapy.
In cosmetology, cryodestruction is often used to remove nodules. However, most medical specialists do not advise resorting to such technology and note that this method causes progression of the disease, which is manifested by the growth of lesions along the periphery.
Surgical excision of granulomas is not performed due to the nature of the skin lesions.
If necessary, it is worth adjusting blood glucose levels, treating chronic infections and concomitant pathologies.
Pyogenic granuloma as an interdisciplinary problem
Pyogenic granulomas can be considered as benign vascular tumors or as reactive vascular changes arising at sites of previous injury or inflammation [1].
Synonyms: botryomycomoma, telangiectatic granuloma, benign pedunculated granuloma, granuloma of pregnancy, lobular capillary hemangioma, eruptive angioma, etc.
The variety of listed synonyms indicates the absence of a common view on the etiopathogenesis of the disease and, as a result, causes significant difficulties in classification, diagnosis, treatment tactics and prognosis of this pathology.
The term “botryomycosis” was proposed by Boullinger, who in 1887 described lung lesions in horses, caused, according to the then assumption, by Botryomyces equina. Ten years later, in 1897, Poncet and Dor first presented patients with what they then believed to be equine botryomycosis. Further research proved the untenability of ideas about the mycotic nature of this disease, however, the term “botryomycoma” is still widely used today.
Different points of view are still expressed about the etiology of pyogenic granuloma. Previously, the disease was regarded as vegetative pyoderma; it is now considered a type of angiomas, developing as a reactive process at the site of microtrauma in the form of a vascular node with profiling capillaries, resembling granulation tissue. Since this formation is essentially neither infectious nor granulomatous, its most accurate name is “lobular capillary hemangioma” [2].
Most often, pyogenic granuloma is observed in young people and adolescents, as well as during pregnancy (in 5% of all pregnancies). Pyogenic granuloma has been reported in the gastrointestinal tract, larynx, nasal mucosa, conjunctiva and cornea [3].
Trauma (including microtrauma), pregnancy, infectious diseases or previous dermatosis are suggested as provoking factors. However, a history of trauma is noted in only 25% of cases.
Cases of the occurrence of multiple pyogenic granulomas on burn surfaces have been described after taking oral contraceptives, protease inhibitors and acne treatment with isotretinoin. It is known that pyogenic granulomas regress after pregnancy. In one study, an increased concentration of vascular endothelial growth factor was found in pyogenic granulomas during pregnancy; after childbirth, the content of this factor was practically not determined; apoptosis of endothelial cells and regression of the granuloma were noted [4].
Clinically, pyogenic granuloma is a soft or densely elastic, painless tumor-like formation on a stalk, 0.5–2.0 cm in diameter, dark red in color, with a smooth or lobulated surface. The stalk, surrounded by a “collar” of exfoliated epithelium, can be of varying length and sometimes gives the tumor a mushroom-like appearance. Appearing several weeks or months later at the site of injury (cut, burn, injection, abrasion, etc.), the granuloma quickly grows, darkens (may become cyanotic), and thickens. Its surface, initially moist, vascular (like a raspberry), erodes, becomes crusty, and bleeds easily with minimal trauma. Often a secondary infection occurs, ulcerations form (sometimes occupying the entire surface of the tumor), necrosis, and bloody-purulent discharge. Palpation is usually painless. More often it is presented by a solitary focus (multiple tumors are rare, but are sometimes observed after extensive burn injuries). Most often it is localized on the hands (especially on the fingers), feet, face, but can also be located on other areas of the skin - on the trunk, genitals, in the perianal area, along the edge of the eyelids and on the tongue. According to observations, in approximately half of cases, pyogenic granuloma is found at the site of an ingrown nail and is one of the most common complications of this pathology [5].
Giant granulomas, with a diameter of 3.0–5.0 cm or more, are traditionally considered a rare phenomenon, but in practice they are detected quite often. According to observations, they periodically occur in bedridden patients at the site of bedsores.
The course of pyogenic granuloma is characterized by rapid growth, the presence of a stabilization phase of the process, and complications in the form of a secondary infection with all the ensuing consequences. This tumor is not characterized by spontaneous regression, but it is not prone to dissemination and malignancy.
Differential diagnosis is usually not difficult. It is carried out with vegetative pyoderma, melanoma, Kaposi's sarcoma, angiosarcoma, glomus tumor, keratoacanthoma, spinous cell epithelioma.
To prevent bleeding and exclude malignancy, removal of the lesion is recommended [6].
Pyogenic granulomas are removed using tangential excision and electrodesiccation; in the latter case, the number of relapses is noticeably lower. During manipulation and excision, the lesions bleed heavily. Lidocaine with epinephrine must be used (with a ten-minute delay of manipulation - the effect of epinephrine), electrocoagulation is used for hemostasis. The focus of pyogenic granuloma, cut off with a scalpel blade, is sent for histological examination. Then curettage of the base of the lesion is performed, which helps stop bleeding and prevent relapse. Curettage and electrodesiccation of the base are carried out until bleeding stops.
There are reports of the effectiveness of cryo- and laser therapy.
We present a clinical case of a patient with pyogenic granuloma.
The patient, born in 1987, complained of a painless formation on the skin of the right hand, bleeding in the area of the rash. She was ill for about 2 weeks when the above complaints first appeared without a clear causal connection. Denies the fact of skin trauma. I did not contact a dermatovenerologist and did not treat myself. Education progressively increased in size.
Life history: tuberculosis, helminthic infestations, viral hepatitis, denies sexually transmitted diseases in the past. Current chronic diseases: denies. Operations, injuries: denies. Allergy history: not burdened. Currently, she is being seen by an obstetrician-gynecologist for pregnancy at 30 weeks.
Objectively: general condition is satisfactory. Position: active. Body temperature 36.7 °C. Upon examination, no pathology was found in the internal organs and systems.
Local status: the pathological skin process is limited in nature, localized on the skin of the palmar surface of the third finger of the right hand. It is represented by a bright red node up to 1.0 cm in diameter, along the periphery there is a rim of exfoliated epidermis, the phalanx of the finger is slightly swollen. On palpation, the formation is soft-elastic, heterogeneous, immobile, painless. Peripheral lymph nodes are not enlarged. Dermographism is mixed. There are no other pathological rashes on the skin or visible mucous membranes (Fig. 1).
During the examination: general blood test, general urinalysis, biochemical blood test - without pathology. Examination for hepatitis HBsAg - not detected. ELISA for antibodies to HIV - negative.
On dermoscopic examination, the formation was of a non-melanocytic nature; Large vascular lacunae of pink-red color and superficial ulceration are visualized.
Considering the bleeding of the formation, progressive increase in size, and state of pregnancy, the patient was referred to a surgeon for excision. Within a week, she was consulted by three surgeons from different health care facilities in Surgut, who doubted the correctness of the diagnosis. There were suggestions of “cancer”, “wart”, etc. A 2-week observation was recommended. During the observation period, the formation slightly increased in size. At the next visit, the surgeon performed outpatient excision of the pyogenic granuloma and treatment with antiseptic solutions (Fig. 2). When examined after 10 days, active epithelization was noted in the lesion and the absence of new rashes (Fig. 3).
Conclusion. Pyogenic granuloma, due to the lack of uniform approaches to treatment, is an interdisciplinary problem and presents certain difficulties for diagnosis among doctors of different specialties. It is advisable to conduct a preliminary dermoscopic examination for the purpose of differential diagnosis with malignant neoplasms of the skin and its appendages.
Literature
- Domanin A. A., Solovyova O. N. Calculation of the diagnostic significance of the morphological signs of pyogenic granuloma and capillary hemangioma. In the book: Treatment-diagnostic, morphofunctional and humanitarian aspects of medicine. Tver, 2011. pp. 57–59.
- Aladin A. S., Yaitsev S. V., Korolev V. N. A case of pyogenic granuloma of the anterior surface of the neck, simulating a malignant tumor (clinical observation) // Tumors of the head and neck. 2011. No. 2. pp. 49–54.
- Novoselov V. S., Gostroverkhova I. P., Novoselova N. V. Clinical cases from the practice of a dermatologist // Russian Medical Journal. 2008. No. 23. P. 1559.
- Skripkin Yu. K. Skin and venereal diseases. M.: Triada-Farm, 2005. 168 p.
- Hebif T.P. Skin diseases: diagnosis and treatment / Trans. from English V. P. Adaskevich; edited by A. A. Kubanova. 4th ed. M.: MEDpress-inform, 2016. 700 p.
- Bogatov V.V., Zemlyakova L.I. Use of a laser scalpel in the treatment of pyogenic granulomas of the maxillofacial region // Bulletin of the Smolensk Medical Academy. 2010. No. 2. pp. 30–32.
E. N. Efanova*, 1, Candidate of Medical Sciences Yu. E. Rusak*, Doctor of Medical Sciences, Professor E. A. Vasilyeva* I. N. Lakomova** R. R. Keldasova*
* BU VO KHMAO-Yugra Surgut State University, Surgut ** BU KHMAO-Yugra Surgut KKVD, Surgut
1 Contact information
Prevention in children
Any granuloma in a child is treated only after consultation with a dermatologist. There are no special methods of prevention. Granuloma annulare in children has variable causes for the development of the disease. Taking into account the influence of immunity on the occurrence of formations, it is necessary to undergo timely treatment. It is necessary to take into account the infectious nature and metabolism in the body. Any disease should receive therapy to reduce risks. This is what prevention consists of – eliminating factors that can provoke the disease.
How to make an appointment with a dermatologist
You can make an appointment with a dermatologist using the special form “Make an appointment with a doctor” - just enter your data so that the administrator can call you back and coordinate the time of the visit. During the consultation, the doctor will examine the clinical picture, prescribe tests if necessary, and select treatment. You can make an appointment with a dermatologist using the number. JSC "Medicine" (clinic of academician Roitberg) has a convenient location at the address: 2nd Tverskoy-Yamskaya lane, building 10. Nearby there are metro stations: "Mayakovskaya", "Tverskaya", "Novoslobodskaya", "Belorusskaya", "Chekhovskaya" .