If caries is not treated in time, serious complications can develop. Periodontitis is one of the most common. This is an inflammation of the connective tissue surrounding the root of the tooth. It is accompanied by acute toothache that cannot be tolerated. Symptoms also include bad breath, mobility of teeth, swelling of the gums, and a cyst at the apex of the root. The disease must be quickly eliminated, otherwise you may lose the tooth.
Does your tooth hurt for a long time after periodontitis treatment? Find out what this might be related to. We tell you in what cases you need the help of a specialist and where to go in Moscow.
Features of periodontitis treatment
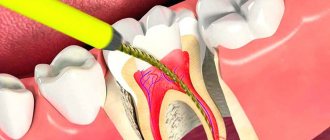
With periodontitis, the inflammatory process often spreads to the entire ligamentous apparatus of the tooth. The disease is often complicated by an abscess, so its treatment is a difficult task. It is aimed at eliminating pain and eliminating the source of inflammation. As a rule, doctors perform the following manipulations:
- remove accumulated exudate,
- thoroughly clean the root canals,
- treat them with medications,
- filled with filling material.
When choosing treatment tactics, the form of the disease, the degree of pathological changes and the clinical picture are taken into account.
Why does periodontitis start?
- As we have already noted, most often periodontitis is a consequence of untreated or poorly treated caries and pulpitis.
There may also be other reasons:
- Mechanical trauma and damage to the pulp, in which inflammation develops over time.
- As a complication of periodontal diseases.
- As a complication of rhinitis, sinusitis, osteomyelitis.
- As a consequence of weakening of the body, vitamin deficiency.
- As a concomitant disease with diabetes mellitus.
- As a result of poor oral hygiene and the presence of tartar in the cervical area.
Possible causes of pain
After treatment of periodontitis, discomfort may persist for 7-14 days. This is due to injury to the tooth tissue. If you follow the recommendations of your doctor, regeneration will accelerate and discomfort will disappear.
If the pain persists for longer, you should consult a specialist. The main reasons for this problem include:
- poor-quality filling – lack or excess of filling material;
- the presence of foreign bodies in the root canals – most often these are elements of dental instruments;
- the emergence of a new focus of inflammation - due to the spread of pathogenic bacteria, tooth tissue can become inflamed again.
These are the most common causes of tooth pain after treatment. A doctor will help determine the provoking factor.
Pain after tooth extraction
In some cases, effective treatment of advanced diseases involves the removal of a diseased tooth followed by prosthetics. After tooth extraction, pain, swelling and redness of the gums are a normal reaction of the body to tissue injury. You should be concerned if:
- the intensity of the pain does not decrease over time and is poorly removed by painkillers;
- the hole does not overgrow for a long time;
- purulent discharge appears from the wound;
- severe swelling of the mucous membrane occurs;
- body temperature rises.
The above symptoms indicate the development of an infectious process in the gum tissue. This happens if the tooth extraction technique is not followed or if the patient does not follow the doctor’s recommendations for oral care.
When should you see a doctor?
Have you recently had a root canal treatment? Does your tooth hurt a lot after periodontitis treatment? Do the unpleasant sensations persist? Make an appointment with your dentist. The specialist will conduct a diagnosis and determine the exact cause of the pain syndrome. If errors were made during treatment, the canals will have to be re-processed and filled.
You should also consult your doctor:
- if the tooth loosens easily,
- When closing the jaws and chewing, there is a sharp pain,
- the gums are very swollen, the lip or cheek is swollen,
- body temperature rises to 38-39 degrees,
- health deteriorates significantly.
You should not endure toothache and drown it out with pills. It may indicate pathological processes occurring inside the tooth. You need to see a doctor and get medical help as soon as possible.
Insidious periodontitis: crept up unnoticed, left without a tooth
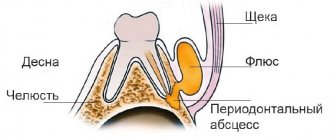
Periodontitis is the next stage of inflammation after pulpitis. The infection is localized at the apex of the tooth root and surrounding tissues. The disease is often asymptomatic, but without timely help it leads to tooth loss.
Causes:
- Untreated pulpitis. If a tooth hurts and then stops, it means that the inflammation has entered a chronic stage. Chronic pulpitis will slowly spread throughout the tooth and turn into periodontitis.
- Pulpitis treated using outdated methods. Before the advent of the apex locator, there was nothing to measure the length of the root canal, and the doctor acted blindly. If the canal is not completely treated and particles of infected pulp remain in it, complications arise. To avoid this, the doctor may have overdone it and brought the dental material beyond the root apex. Over the years, a focus of infection sometimes develops around a lump of paste.
- Tooth injury. A common problem in active children. Due to injury (the incisors are often affected), the pulp dies, and periodontitis develops after this. In fact, the reason is the same pulpitis that was not noticed and not treated in time.
Types of periodontitis
| Form | View | How it hurts |
| Spicy | Serous | Mild aching pain in the tooth area. |
| Purulent | Throbbing pain. Tooth mobility may increase. Possible swelling of the cheek, weakness, fever, flux. | |
| Chronic | Fibrous | No symptoms or slight darkening, dull color of the crown of the tooth. |
| Granulating | Mild pain when biting eventually turns into pain from heat, chewing, or pressure. The gums become red and swollen. | |
| Granulomatous | No symptoms. A fistula appears to drain the discharge, but the patient cannot always see it. |
The most aggressive is granulating periodontitis, which very quickly spreads to neighboring tissues. With this diagnosis, most often the tooth cannot be saved.
In the granulomatous type of the disease, the inflammation site has a hard shell, and inside it is filled with pus. Depending on the size, these neoplasms are called granuloma (up to 5 mm), cystogranuloma or radicular cyst (more than 1 cm).
Thus, granuloma and tooth root cyst are manifestations of chronic periodontitis.
Diagnostics
Do not confuse fistula with stomatitis. The fistula looks like a pimple, is located on the gum near the roots of the tooth, and does not hurt when pressed. If a fistula appears, contact your dentist as soon as possible.
The doctor can suspect a problem before the formation of a fistula or gumboil based on complaints. It is very important that the patient describes all the symptoms and does not hesitate to complain about mild, unexpressed, occasional pain and discomfort.
X-rays help to accurately establish the diagnosis. Periodontitis is visible even on a small targeted photograph. Next, to plan treatment, the dentist will suggest taking a panoramic image (all teeth in one frame) or a computer tomogram (a three-dimensional image of the dental system).
CT - 3D computer tomogram
allows you to see the type of periodontitis, the location and size of cystogranuloma, and give a prognosis for treatment.
Positive dynamics
visible on a repeat tomogram 2 years later
From all sides
The advantage of CT is the ability to examine the tooth and the tissue around it from different angles
Treatment
Depending on the stage and form of the disease, the doctor will select the optimal method.
1. Therapeutic treatment. Typically, three visits to the dental office are required.
- Urgent Care. The dentist will remove the source of inflammation: clean and disinfect the canals using medications and laser sterilization. If necessary, the doctor will install a drainage to drain the pus.
- Treatment of tooth canals and installation of a temporary filling. If there are doubts that the immune system will cope with the remaining microorganisms, the dentist may prescribe antibiotics, physiotherapy, rinses and medicinal baths.
- Tooth restoration. At the last visit, the dentist will take an x-ray to make sure that the inflammation has been removed. After this, you can begin filling and restoring the aesthetics and chewing function of the tooth.
- Observation. We can talk about the positive dynamics of the tissues surrounding the tooth after 1-2 years based on the results of an x-ray examination.
2. Tooth-preserving operations. Sometimes conservative methods are not enough. A dental surgeon can perform a cystectomy (removal of the cyst) or apex resection (cutting off part of the tooth along with the cyst).
3. Tooth extraction. In advanced stages, it will not be possible to completely defeat foci of infection. Attempts to save a tooth will lead to large financial expenses and jeopardize neighboring teeth. The best solution would be to install an implant in place of the affected tooth.
If a tooth is left without treatment, it will be removed prematurely. The inflammation will grow and go into an acute stage, and at the most unfortunate moment.
Doctors call chronic periodontitis a ticking time bomb. Exacerbation is provoked by stress, exertion, hypothermia or climate change. That is, it will happen on a long-awaited trip to the sea, while working on an important project, before an exam, or during an infectious disease.
Periodontitis in children
In a child, periodontal inflammation can develop on both milk and permanent teeth. Features of childhood periodontitis:
- high flow rate,
- severe symptoms (temperature, pain, swelling, possible suppuration),
- increased risk of complications. If urgent measures are not taken, the rudiments of permanent teeth will suffer.
Treatment follows the same scheme as for adults. If there is less than a year left before a baby tooth falls out or the roots have already resolved, the pediatric dentist will suggest removing the tooth.
Prevention
Simple and inexpensive measures will reduce the risks of periodontitis and tooth loss.
- Maintain good oral hygiene.
- Eat right. Excess carbohydrate foods provoke the development of pathogenic microorganisms.
- Contact a specialist for dental treatment in a timely manner. Come for a routine examination every six months, even if nothing hurts. Voice all complaints.
- Treat with understanding the doctor’s suggestion to undergo a panoramic radiography or computed tomography. Complete information will allow you to notice and cure the disease.
For expert assistance in writing the article and providing examples of work, we thank dentist-therapist Olga Yuryevna Yuryeva.
PS
In this article, we deliberately do not touch upon mistakes made by dentists that may cause pain. God forbid that a seed of doubt should be planted in you. It is very important to trust your doctor or better look for another! Any doctor will say that the most difficult patient is the patient who does not believe in his recovery. But if you have doubts about the doctor’s competence, then the best decision is to go to another for a second opinion. Take pictures before and immediately after treatment, and keep these pictures for yourself. This will help prove you are right if something goes wrong. And trust your doctor!
The situation where pain may occur is quite predictable. In such cases, the dentist always warns the patient about possible pain. And if the pain goes away after a week or two, then there is nothing to worry about.
Forms of periodontitis and their symptoms.
There are two main forms of periodontitis and it is important not to get confused by their symptoms, because some of them are insidious:
- Acute periodontitis.
Acute periodontitis can begin sluggishly and unnoticeably.
Then the symptoms begin to increase, and as acute inflammation develops in the periodontium, the following symptoms appear:
- Aching pain that intensifies with pressure and gradually becomes unbearable.
- Reaction to hot food.
- Swelling of the gums and/or cheeks.
- “Big tooth” syndrome, in which the patient feels that the tooth has “increased in volume” and is protruding from the dental arch.
- The tooth becomes mobile in the socket.
- A fistula may form to drain pus.
- General intoxication of the body - temperature, fever, headache, leukocytosis.
A feature of acute periodontitis is that it is not determined by an x-ray, because at this stage of the disease there are no characteristic changes in the periodontal fissure.
- Chronic periodontitis
Chronic periodontitis develops latently, there is no pronounced tissue inflammation, it develops gradually. This form of the disease is dangerous because the symptoms of chronic periodontitis are virtually absent, and at this time tissue damage progresses and irreversible processes occur in them - atrophy of the tooth socket, tooth loosening, formation of cysts and granulomas.
The main symptoms of chronic periodontitis are:
- Heaviness.
- Feeling of fullness.
- Discomfort when chewing on the affected side.
In addition, from time to time chronic periodontitis can worsen, and then it is characterized by the same symptoms as the acute form.
Very often, chronic periodontitis is diagnosed incidentally using an x-ray, usually taken for another dental problem.
We would like to add that the earlier periodontitis is diagnosed in a patient, the higher the likelihood of complete recovery and preservation of the tooth, even without the use of surgical treatment methods.