The most common form of gingivitis is catarrhal gingivitis, which affects the gums, causing superficial inflammation. Most often, this disease affects children and young people under 35 years of age. In older patients, as a rule, chronic catarrhal gingivitis is diagnosed.
Teeth polishing with pastes - 1,200 rubles.
Polishing one tooth with paste - 50 rubles.
Coating with a fluoride-containing product (1 row of teeth) - RUB 1,500.
Coating with fluorine-containing varnish (1 tooth) - 250 rubles.
Retraction of hypertrophied gums in the area of 1 tooth - 600 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Classification of gingivitis according to ICD:
- K05.0. Acute gingivitis
- K05.00 Acute streptococcal gingivostomatitis
- K05.08 Other specified acute gingivitis
- K05.09 Acute unspecified gingivitis
- K05.1. Chronic gingivitis
- K05.10 Simple marginal gingivitis
- K05.19 Chronic unspecified gingivitis
- K06.0. Gum recession.
- K06.1. Gingival hypertrophy.
- K06.2. Lesions of the gums and edentulous alveolar margin caused by trauma.
- K06.9. Changes in the gingiva and edentulous alveolar margin, unspecified.
Causes of gingivitis
1) Local factors4
- Poor oral hygiene. This is the most popular reason, since bacteria multiply in plaque and tartar, which are formed due to insufficient hygiene, which provoke gum inflammation.
- Injuries and burns to the mucous membrane due to eating hard or hot foods. If they are regular, the wounds can become infected, which also contributes to inflammation.
- Injury to gums from old fillings, crowns, and braces.
- Smoking. Tar and other substances from cigarettes settle on the teeth, forming plaque and irritating the gum mucosa; nicotine, in turn, impairs blood flow to the gums.
- Eruption of wisdom teeth. If a tooth is cut for a long time and incorrectly, it can become a source of constant inflammation and provoke gingivitis.
2) General factors
- Poor diet with insufficient vitamins
- Weakened immunity, immunodeficiency states
- Long-term, incorrect use of antibiotics
- Allergy
- Impaired metabolism
- Digestive system diseases (Crohn's disease)
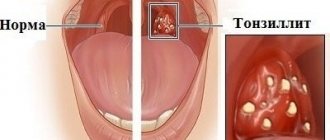
- Frequent sore throats, tonsillitis, sinusitis
- Stress
- Pregnancy, as it changes hormonal levels and the worst effect is on the gums
- Diabetes
Symptoms of gingivitis
- Bleeding gums are the main symptom of gingivitis. Bleeding can occur both while brushing your teeth and when eating. Spontaneous bleeding also occurs
- Swelling and swelling of the gums, which can make teeth appear smaller.
- Pain of varying severity
- Change in gum color: it becomes bright red or blue.
- Deterioration of general condition, fever, weakness, headache
The presence of symptoms and their severity depends on the form and severity of the disease.
Where to treat?
By contacting the Good Hands clinic, you can undergo diagnosis and treatment of catarrhal gingivitis using modern techniques and effective drugs. Our specialists have extensive experience in successfully treating this disease and give a positive prognosis in the vast majority of cases when promptly seeking professional dental care. You can sign up with us for a free consultation if you are concerned about certain symptoms and find out whether we have the disease or how to exclude its development.
Forms of gingivitis
Catarrhal gingivitis
The most common form of gingivitis is the classic form. Many people encounter it at school, but do not pay attention. If you experience even slight bleeding while brushing your teeth, you should immediately consult a doctor. In addition to bleeding, symptoms such as bad breath, itching, and burning may occur.
Hypertrophic gingivitis
With this form of the disease, the gum increases in size and can cover half of the tooth or more. This form of gingivitis can be caused by hormonal changes in pregnant women and adolescents, as well as by taking medications.
Ulcerative gingivitis
The most dangerous and difficult to tolerate form of gingivitis, it causes necrosis (death) of the gums, severe pain, and a very sharp and unpleasant odor from the mouth. Sometimes it is painful for a person suffering from ulcerative gingivitis to even eat and speak, and the general condition is also disturbed. This form of gingivitis affects people with weakened immune systems.
Desquamative gingivitis
It manifests itself as swelling, bleeding and pain in the gums. The gums become bright red, “glazed”, and are easily injured.5
Atrophic gingivitis
It is characterized by a decrease in the size of the gums: it becomes thin, easily injured, and the roots of the teeth are exposed. The teeth seem longer, pain appears from cold or hot things. This form of the disease is rare.
Symptoms depend on the form of the disease:
Edema form
The gums between the teeth are red, swollen, glossy, and a false pocket forms between the enlarged gum and the tooth. There is a change in the appearance of the gums, it looks swollen, bleeds, hurts when brushing teeth, and there is a feeling of burning and swelling. The edematous form develops as a complication of catarrhal gingivitis under the influence of an irritating factor (crown edge, fillings, braces, etc.). During pregnancy, hypertrophic gingivitis develops if the woman already had catarrhal gingivitis before pregnancy. The disease may resolve spontaneously after childbirth.
Fibrous form
The gum, as normal, is pale pink, there is no pain or bleeding, but its growth is observed, there are false pockets between the tooth and the gum. Abundant dental deposits are found above and below the gum. The fibrous form often develops when taking medications or in the presence of general diseases, i.e. this is the reaction of the gums to internal changes.
Diagnosis of gingivitis
It is always important to collect a complete history of the disease, because gingivitis is often a chronic disease that occurs in childhood.6
It is also worth paying attention to the general condition of the body; the dentist may refer you to other specialists.
Consultation with an endocrinologist – in diseases of the endocrine system (diabetes mellitus, hyperfunction of the thyroid gland and adrenal glands), gum inflammation is more active.
Consultation with a hematologist – in case of blood diseases, gum inflammation is only a symptom of the underlying disease. Consultation with a hematologist is required for differential diagnosis and comprehensive treatment.
Consultation with a gastroenterologist – gingivitis is usually accompanied by chronic diseases of the digestive system.
Related doctors, in turn, prescribe a number of other tests to treat pathology, for example, a general blood test, biochemical blood test, gastroscopy, ultrasound, etc.
The dental office conducts diagnostic tests such as:
- Probing is a diagnostic method in which the characteristics of the attachment of the gums to the teeth are determined.
- Staining the gums with iodine-containing solutions: this shows whether the gums are inflamed. With gingivitis, the gums turn shades of brown.
- Determining the level of hygiene, that is, how well a person brushes his teeth.
- Panoramic X-ray of the teeth: This is necessary to see whether the inflammation has affected the bone or not, and also shows the condition of all teeth, fillings and crowns.
Acute gingivitis
The diagnosis of “acute gingivitis” is based on the collected medical history, physical examination data, and the results of additional research methods. During an examination for catarrhal gingivitis, the dentist identifies hyperemic, swollen gums. The papillae are tense and bleed when touched lightly. The integrity of the dental epithelial attachment in acute gingivitis is preserved; there are no periodontal pockets. In the desquamative form of acute gingivitis, along with swelling and bleeding in the gum area, areas of desquamation of the surface epithelium are diagnosed.
Ulcerative gingivitis is characterized by the formation of ulcers. The gingival margin is corroded and the interproximal spaces are gaping. Regional lymph nodes in patients with the ulcerative form of acute gingivitis are enlarged. The Schiller-Pisarev test for acute gingivitis is positive. After applying iodine-containing preparations, the color of the mucous membrane changes from light yellow to dark brown. The intensity of staining correlates with the severity of inflammation. The PMA index in acute gingivitis is positive. When the interdental papillae are affected, PMA is 25%; when the marginal part of the gums is involved in the pathological process, PMA is 50%. If the PMA index is more than 50%, this indicates the presence of inflammatory changes in the alveolar gum area.
When assessing the level of hygiene in acute gingivitis, high numbers of Green-Vermillion indicators are revealed, which indicates an unsatisfactory hygiene index. On a targeted radiograph and orthopantomogram, there are no pathological changes in the bone tissue of the alveolar process. In the ulcerative form of acute gingivitis, using bacterioscopic examination, it is possible to detect in the surface layer of the mucosa, along with the resident microflora of the oral cavity, an increased content of fusobacteria and spirochetes. The deeper tissues contain exclusively pure culture of fusispirillary symbiosis. When conducting bacterioscopy in patients with the catarrhal form of acute gingivitis, an increased number of actinomycetes is detected.
It is necessary to differentiate acute gingivitis of infectious origin not only from periodontitis, but also from a secondary inflammatory process that develops with blood diseases, pathologies of the endocrine system, and disorders of the functioning of the gastrointestinal tract. To exclude symptomatic acute gingivitis, consultations with specialized specialists are indicated: hematologist, endocrinologist, gastroenterologist.
Answers to popular questions
How to stop bleeding gums at home?
Herbal rinses (for example, oak bark) will help stop the bleeding, but they only give a temporary effect and mask the problem.
Can a hard brush cause gingivitis?
No, the brush itself does not cause gingivitis, but too hard bristles can damage the enamel. For most people, medium-hard brushes are suitable.
I don’t have problems with my gums, but my gums often hurt and bleed in only one place, what should I do?
It's worth seeing a doctor. Most likely, there is an old filling in this place, in which food gets stuck and inflammation begins.
Is gingivitis curable or is it permanent?
Fortunately, yes, if you follow all the recommendations, you will not only cure gingivitis, but also not see it again.
Treatment of gingivitis
Treatment of gingivitis is always complex.
- Local treatment
- General treatment
Local treatment of gingivitis
1. Removing plaque and stone. Since stone and plaque are the main causes of gingivitis, they must be removed to get rid of the disease. This is done using special dental instruments, ultrasound, laser, hand instruments - the method is selected depending on the condition of the gums. If gingivitis has already occurred, simply brushing your teeth well at home will not be enough; you need to consult a doctor.
2. Treatment of caries and its complications , replacement of old crowns and fillings.
If there are injuries from braces, it is necessary to use special wax. 3. Drug therapy includes antiseptics, anti-inflammatory, antibacterial and painkillers, depending on the form of gingivitis.
4. Surgical operations. If the gums have grown excessively, or, conversely, have exposed the roots of the teeth too much, surgical intervention may be required.
5. Training in proper hygiene. This is necessary to consolidate the results of treatment and speedy recovery. The doctor helps you choose the right medications
hygiene and teaches proper teeth brushing.
Gingivitis: treatment at home
Gingivitis can result not only from the accumulation of plaque on the edge of the gum due to the use of inappropriate hygiene products, but also develops due to internal problems in the body. At home, it is quite possible to combat the results of the initial stages of catarrhal gingivitis, but you will not be able to get rid of stones with rinses and prepared solvents. You still have to sit in the doctor's chair.
In addition, self-medication of ulcerative or hypertrophic gingivitis is unacceptable. There is an extremely high risk of harming a person and worsening the patient’s condition.
Doctors also advise critically perceiving information about miracle cures presented in advertising. The phrase “Specialist consultation required,” which is now demonstrated in every video, took a lot of persistence from doctors. The fact is that any product is advertised as effective, but it is not specified that we are talking about symptomatic effects. The patient will be able to get rid of the symptoms, but the advertising product is not able to cure the cause that causes them - periodontal plaque, mineralized deposits. Therefore, consultation with a professional is absolutely required.
Prevention of gingivitis
It's always easier to prevent something than to treat it. Therefore, it is very important to follow the recommendations below:10
- You need to brush your teeth 2 times a day: morning and evening
- After each appointment, it is not necessary to brush your teeth, but you should rinse your mouth with water
- It is very important to use all personal hygiene products and do it correctly, you need dental brushes and dental floss
- Visit your dentist once or twice a year for a checkup and professional cleaning. It will remove plaque and be able to recognize gingivitis at an early stage
- Treat all concomitant diseases of the body.
- If installed structures in the mouth (fillings, dentures, braces) injure the mucous membrane, consult a doctor.
- Lead a healthy lifestyle: exercise, exercise, eat right
These measures will help you avoid gum disease and keep your mouth healthy.
Colored plaque
The brightest color is painted on the denser plaque; it is in these areas that teeth are most often not cleaned, which leads to gum inflammation.
After the final diagnosis, the dentist selects treatment tactics depending on the identified form of gingivitis.